Urostomy and Continent Urinary Diversion
On this page:
Your kidneys filter waste and excess fluid from your blood, making urine. The urine then travels from the kidneys to the bladder through tubes called ureters. The bladder stores urine until you have the sensation to void. If your bladder is injured or diseased, you may not be able to urinate in the normal way.
A urinary diversion is a way to release urine from the body when you can’t urinate because the urinary system is damaged or not working. You will need a urinary diversion, for example, if your bladder has been removed to stop the spread of cancer, or if your bladder has nerve damage. Any problem in the bladder that blocks the flow of urine and causes it to accumulate in the ureters and kidneys may result in the need for a urinary diversion.
A urinary diversion may mean a urostomy, which requires a pouch to be worn outside the body, or a continent diversion, which involves the creation of a pouch or bladder inside the body, usually using part of the digestive tract.
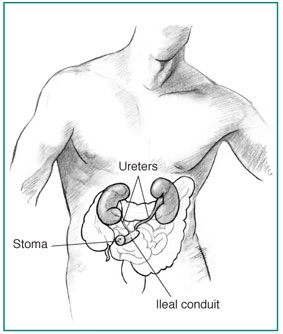
The ileal conduit is made from a short segment of the small intestine. The ureters are attached to one end of the conduit. The other end is placed at the skin’s surface to create a stoma. Urostomy
A surgeon creates a urostomy by redirecting your urine to an opening created in the abdomen. The opening is called a stoma. Two main types of urostomy are available.
- Ileal conduit. To create an ileal conduit, the surgeon takes a short segment of the small intestine and reconnects the remaining intestine so that it functions normally. One end of the removed short segment of intestine is placed at the skin surface to create the stoma. The ureters, which normally carry urine from the kidneys to the bladder, are then attached to the other end of the segment of intestine. The urine travels through the newly formed ileal conduit and the stoma into an external collecting pouch. The pouch has an outlet for releasing urine into a toilet without removing it from your stoma.
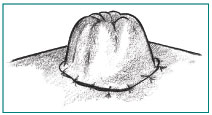
A stoma is an opening in the abdomen used for releasing urine from the body.
- Ureterostomy. Very rarely, the surgeon connects the ureters directly to the abdominal wall to create a stoma. Like the ileal conduit, a ureterostomy requires a collecting pouch placed over the stoma because there are no muscles around the stoma to control the flow of urine.
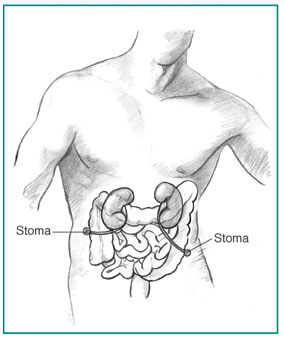
In a ureterostomy, the ureters are connected directly to the abdominal wall to create two stomas.
[Top]
Continent Diversion
Another method of storing and eliminating urine is the continent diversion. In this method, the surgeon creates a pouch, or reservoir, inside your body from a section of your stomach or small or large intestine. The ureters carry urine to the pouch, where it is stored. Depending on the type of continent diversion, you may or may not have a stoma.
- Continent cutaneous reservoir. This form of continent diversion does include a stoma. This method requires you to empty the reservoir, the internal pouch, regularly through the stoma using a catheter or thin plastic tube.
If your urethra is preserved during the operation, you may be able to have a urinary diversion that does not require a stoma or catheter.
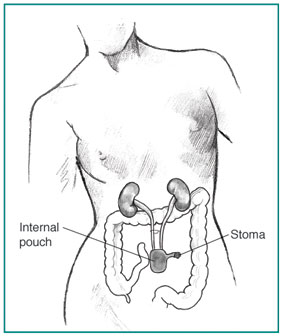
With a continent cutaneous reservoir, an internal pouch stores urine. The patient uses a catheter or plastic tube to empty urine through the stoma.
- Bladder substitute. This method lets you urinate through your own urethra as you did with your original bladder, or you may have to empty using a catheter through your urethra. The surgeon creates an internal pouch that stores urine as your bladder did. It is connected to your urethra so you may be able to empty your bladder in the normal way, although you will need to use different muscles to expel the urine.
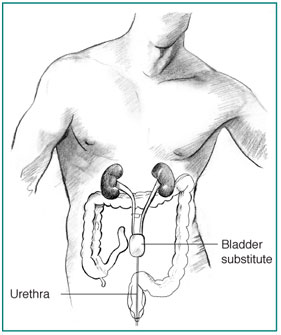
With a bladder substitute, the patient can urinate through the urethra.
[Top]
Caring for Your Urinary Diversion
After your surgery, a wound, ostomy, and continence (WOC) nurse can work with you to help you learn how to take care of your urinary diversion. WOC nurses are experienced and knowledgeable, so don’t be shy about asking questions if you have any concerns.
Changing Pouches
If you have an ileal conduit or ureterostomy, you will work with your doctor or WOC nurse to learn how to change your pouch. Your pouching system may consist of two pieces—a barrier that sticks to your skin and a pouch that attaches to the barrier. In some systems, the barrier and pouch are a single unit.
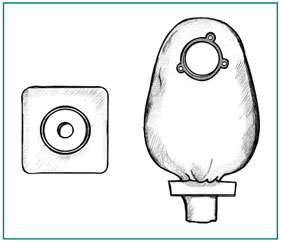
A two-piece pouch system. The square barrier sticks to the skin. The pouch attaches to the barrier. Using a Catheter
If you have a continent reservoir, you will learn how to insert a catheter through the stoma or your urethra to drain your reservoir. You may do this either by standing in front of the toilet or by sitting on the toilet and then emptying the catheter between your legs. In the first few weeks, you will need to use the catheter every couple of hours. Soon, you will be able to go 4 to 6 hours between catheterizations. Wash your hands with soap and water each time you use a catheter.
Cleaning
If you use a pouch, you can clean your skin with a wet towelette or washcloth as you change the pouch. Let your skin dry completely before you apply the new pouch. If your skin becomes irritated, you can use protective skin wipes or an ostomy powder designed to protect the skin around a stoma.
If you have a continent diversion, you will need to irrigate, or flush out, the reservoir using sterile water or normal saline and a syringe. Since the reservoir may be made from a part of the intestine, it may produce mucus that normally lines the digestive tract. Irrigating or flushing the reservoir clears this mucus from the reservoir. Talk with your health care provider about how often you should irrigate the reservoir.
Recognizing Infection
Urostomies and continent urinary diversions can get infected. Symptoms of infection include
- dark urine or urine containing excess mucus
- strong-smelling urine
- pain in the back
- poor appetite
- nausea
- vomiting
Call your health care provider if you notice any of these warning signs. Drinking eight full glasses of water every day can help prevent infection by flushing out bacteria.
Diet
You probably will be able to eat your normal diet. You may find that some foods, such as asparagus and seafood, cause urine to have a stronger odor. Talk with your health care provider about your dietary needs.
Clothing
Wearing a urostomy pouch does not require special clothing. Modern pouches are designed to lie flat against the body so they can’t be noticed. You may wear the pouch tucked inside your underwear or between your underwear and your outer clothing. Women may wear a pouch under a girdle as long as it is made of stretchy material. Men may wear the pouch inside an athletic supporter.
Activities
You will need to restrict your activity during the first 2 to 3 weeks after surgery. Avoid driving and heavy lifting to help your stoma heal. Once healed, you should be able do most of the activities you enjoyed before your surgery. The only exceptions may be contact sports like football or karate. If your job includes hard physical labor, talk with your doctor and your employer about making adjustments to your job responsibilities.
Relationships
You may worry that people will have negative reactions regarding your surgery. Most people will never know that you are wearing a pouch, unless you choose to tell them. Friends and relatives are likely to be aware of your health problems, but only a spouse, intimate partner, or primary care taker need know the details of your urinary diversion surgery. Still, many people find being open about their situation is easier than keeping it a secret. You can choose how much you will share about your condition.
You can still maintain a satisfying sexual relationship with your partner. Your doctor or WOC nurse will tell you when you may safely resume sexual activity after your surgery. Talk with your health care provider about any concerns you have with maintaining intimate relations. Your nurse or doctor can give you information about ways to protect your stoma during sex. You may also want to ask about specially designed apparel to enhance intimacy for people with ostomies. Communicating with your partner is essential. Share your concerns and wishes, and listen carefully to your partner’s concerns.
[Top]
Hope through Research
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) has many research programs aimed at finding and improving treatments for urinary disorders. Researchers supported by the
NIDDK are working to understand the growth of bladder tissue in order to find artificial methods of generating that kind of tissue. In an experimental setting, a patient whose bladder must be removed may be given a replacement bladder made from bioengineered tissues instead of from a segment of the patient’s bowel. The bioengineered tissue would function much more like a natural bladder.
[Top]
For More Information
American Urological Association, Inc.
1000 Corporate Boulevard
Linthicum, MD 21090
Phone: 1–800–RING–AUA (746–4282) or 410–689–3700
Email: aua@auanet.org
Internet: www.urologyhealth.org
Wound, Ostomy & Continence Nurses Society
4700 W. Lake Avenue
Glenview, IL 60025–1485
Phone: 1–888–224–9626
Email: info@wocn.org
Internet: www.wocn.org
[Top]
National Kidney and Urologic Diseases Information Clearinghouse
3 Information Way
Bethesda, MD 20892–3580
Phone: 1–800–891–5390
TTY: 1–866–569–1162
Fax: 703–738–4929
Email: nkudic@info.niddk.nih.gov
Internet: www.kidney.niddk.nih.gov
The National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC) is a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The NIDDK is part of the National Institutes of Health of the U.S. Department of Health and Human Services. Established in 1987, the Clearinghouse provides information about diseases of the kidneys and urologic system to people with kidney and urologic disorders and to their families, health care professionals, and the public. The NKUDIC answers inquiries, develops and distributes publications, and works closely with professional and patient organizations and Government agencies to coordinate resources about kidney and urologic diseases.
This publication was reviewed by Susan Appleby, WOCN, Banner Home Care; and Anthony Atala, M.D., Wake Forest University.
This publication is not copyrighted. The Clearinghouse encourages users of this publication to duplicate and distribute as many copies as desired.
NIH Publication No. 06–5629
May 2006
[Top]
|