Introduction
The Kidneys
Understanding Cancer
Kidney Cancer: Who's at Risk?
Symptoms
Diagnosis
Staging
Treatment
Side Effects of Cancer Treatment
Nutrition
Follow-up Care
Support for People with Kidney Cancer
The Promise of Cancer Research
National Cancer Institute Booklets
National Cancer Institute Information Resources
Introduction
This National Cancer Institute (NCI) booklet (NIH Publication No. 03-1569) has important information about
cancer*
of the kidney. It discusses possible causes, symptoms, diagnosis, and treatment. It also has information to help patients cope with kidney cancer.
Scientists are studying kidney cancer to learn more about this disease. They are finding out more about its causes, and doctors also are exploring new ways to treat it. This research keeps increasing our knowledge about kidney cancer. The NCI provides the most up-to-date information over the telephone and on the Internet:
Telephone: Information Specialists at NCI's Cancer Information Service at
1-800-4-CANCER can answer questions about cancer and can send materials published by NCI.
Internet: People can ask questions online and get immediate help through LiveHelp 1 on the Internet. Many NCI booklets and fact sheets can be viewed at
http://cancer.gov/publications. People in the United States and its territories may use this Web site to order publications. This Web site also explains how people outside the United States can mail or fax their requests for NCI publications.
*Words that may be new to readers appear in italics. The
"Dictionary 2" section explains these terms. Some words in the
"Dictionary" have a "sounds-like" spelling to show how to
pronounce them.
The Kidneys
The
kidneys
are a pair of
organs
on either side of the spine in the lower
abdomen. Each kidney is about the size of a fist. Attached to the top of each kidney is an
adrenal gland. A mass of fatty
tissue
and an outer layer of
fibrous
tissue
(Gerota's fascia)
enclose the kidneys and adrenal glands.
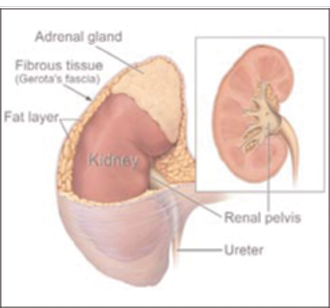
|
| This picture shows the kidney and adrenal gland. |
The kidneys are part of the
urinary tract. They make
urine
by removing wastes and extra water from the
blood.
Urine collects in a hollow space
(renal pelvis)
in the middle of each kidney.
It passes from the renal pelvis into the
bladder
through a tube called a
ureter.
Urine leaves the body through another tube (the
urethra).
The kidneys also make substances that help control
blood pressure and the production of
red blood cells.
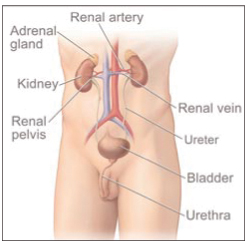
|
| This picture shows the male urinary tract. |
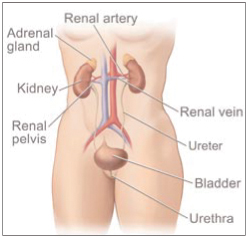
|
| This picture shows the female urinary tract. |
Understanding Cancer
Cancer begins in
cells,
the building blocks that make up tissues. Tissues make up the organs of the body.
Normally, cells grow and divide to form new cells as the body needs them. When cells grow old, they die, and new cells take their place.
Sometimes this orderly process goes wrong. New cells form when the body does not need them, and old cells do not die when they should. These extra cells can form a mass of tissue called a growth or
tumor.
Tumors can be
benign
or
malignant:
- Benign tumors are not cancer:
- Benign tumors are rarely life threatening.
- Usually, benign tumors can be removed, and they seldom grow back.
- Cells from benign tumors do not invade tissues around them or spread to other parts of the body.
- Malignant tumors are cancer:
- Malignant tumors are generally more serious than benign tumors. They may be life threatening.
- Malignant tumors often can be removed, but they can grow back.
- Cells from malignant tumors can invade and damage
nearby tissues and organs. Also,
cancer cells can break away from a malignant tumor
and enter the bloodstream or
lymphatic system. That is how cancer cells spread from the original cancer
(primary tumor)
to form new tumors in other organs. The spread of cancer is called
metastasis.
Several types of cancer can start in the kidney. This booklet is about
renal cell cancer,
the most common type of kidney cancer in adults.
This type is sometimes called
renal adenocarcinoma
or
hypernephroma.
Another type of cancer,
transitional cell carcinoma,
affects the renal pelvis. It is similar to bladder
cancer and is often treated like bladder cancer.
Wilms' tumor
is the most common type of childhood kidney cancer. It is different from adult kidney cancer and requires different treatment. Information about transitional cell carcinoma and Wilms' tumor is available from the Cancer Information Service at
1-800-4-CANCER and at
http://www.cancer.gov.
When kidney cancer spreads outside the kidney,
cancer cells are often found in nearby
lymph nodes.
Kidney cancer also may spread to the lungs, bones, or liver. And it may spread from one kidney to the other.
When cancer spreads (metastasizes) from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary tumor. For example, if kidney cancer spreads to the lungs, the cancer cells in the lungs are actually kidney cancer cells. The disease is metastatic kidney cancer, not lung cancer. It is treated as kidney cancer, not lung cancer. Doctors sometimes call the new tumor metastatic or "distant" disease.
Kidney Cancer: Who's at Risk?
Kidney cancer develops most often in people over 40, but no one knows the exact causes of this disease. Doctors can seldom explain why one person develops kidney cancer and another does not. However, it is clear that kidney cancer is not contagious. No one can "catch" the disease from another person.
Research has shown that people with certain
risk factors
are more likely than others to develop kidney cancer. A risk factor is anything that increases a person's chance of developing a disease.
Studies have found the following risk factors for kidney cancer:
- Smoking: Cigarette smoking is a major risk factor. Cigarette smokers are twice as likely as nonsmokers to develop kidney cancer. Cigar smoking also may increase the risk of this disease.
- Obesity: People who are
obese
have an increased risk of kidney cancer.
- High blood pressure: High blood pressure increases the risk of kidney cancer.
- Long-term
dialysis: Dialysis is a treatment for people whose kidneys do not work well. It removes wastes from the blood. Being on dialysis for many years is a risk factor for kidney cancer.
-
Von Hippel-Lindau (VHL) syndrome: VHL is a rare disease that runs in some families.
It is caused by changes in the VHL
gene.
An abnormal VHL gene increases the risk of
kidney cancer. It also can cause
cysts
or tumors in the eyes, brain, and other parts of the body. Family members of those with this syndrome can have a test to check for the abnormal VHL gene. For people with the abnormal VHL gene, doctors may suggest ways to improve the detection of kidney cancer and other diseases before
symptoms
develop.
- Occupation: Some people have a higher risk of getting kidney cancer because they come in contact with certain chemicals or substances in their workplace. Coke oven workers in the iron and steel industry are at risk. Workers exposed to
asbestos
or
cadmium
also may be at risk.
- Gender: Males are more likely than females to be diagnosed with kidney cancer. Each year in the United States, about 20,000 men and 12,000 women learn they have kidney cancer.
Most people who have these risk factors do not get kidney cancer. On the other hand, most people who do get the disease have no known risk factors. People who think they may be at risk should discuss this concern with their doctor. The doctor may be able to suggest ways to reduce the risk and can plan an appropriate schedule for checkups.
Symptoms
Common symptoms of kidney cancer include:
- Blood in the urine (making the urine slightly rusty to deep red)
- Pain in the side that does not go away
- A lump or mass in the side or the abdomen
- Weight loss
- Fever
- Feeling very tired or having a general feeling of poor health
Most often, these symptoms do not mean cancer. An infection, a cyst, or another problem also can cause the same symptoms. A person with any of these symptoms should see a doctor so that any problem can be diagnosed and treated as early as possible.
Diagnosis
If a patient has symptoms that suggest kidney cancer, the doctor may perform one or more of the following procedures:
- Physical exam: The doctor checks general signs of health and tests for fever and high blood pressure. The doctor also feels the abdomen and side for tumors.
- Urine tests: Urine is checked for blood and other signs of disease.
- Blood tests: The lab checks the blood to see
how well the kidneys are working. The lab may check
the level of several substances, such as
creatinine.
A high level of creatinine may mean the kidneys are not doing their job.
-
Intravenous pyelogram (IVP):
The doctor injects dye into a vein in the arm.
The dye travels through the body and collects
in the kidneys. The dye makes them show up on
x-rays.
A series of x-rays then tracks the dye as it moves through the kidneys to the ureters and bladder. The
x-rays can show a kidney tumor or other problems.
-
CT scan
(CAT scan): An x-ray machine linked to a computer takes a series of detailed pictures of the kidneys. The patient may receive an injection of dye so the kidneys show up clearly in the pictures. A CT scan can show a kidney tumor.
-
Ultrasound test: The ultrasound device uses sound waves that people cannot hear. The waves bounce off the kidneys, and a computer uses the echoes to create a picture called a
sonogram.
A solid tumor or cyst shows up on a sonogram.
-
Biopsy:
In some cases, the doctor may do a biopsy.
A biopsy is the removal of tissue to look for cancer cells. The doctor inserts a thin needle through the skin into the kidney to remove a small amount of tissue. The doctor may use ultrasound or x-rays to guide the needle.
A
pathologist
uses a microscope to look for cancer cells in the tissue.
- Surgery: In most cases, based on the results of the CT scan, ultrasound, and x-rays,
the doctor has enough information to recommend surgery to remove part or all of the kidney. A pathologist makes the final diagnosis by examining the tissue under a microscope.

|
|
 |
Staging
To plan the best treatment, the doctor needs to know the
stage
(extent) of the disease. The stage is based on the size of the tumor, whether the cancer has spread and, if so, to what parts of the body.
Staging
may involve
imaging
tests such as an ultrasound or a CT scan. The doctor also may use an
MRI.
For this test, a powerful magnet linked to a computer makes detailed pictures of organs and blood vessels.
Doctors describe kidney cancer by the following stages:
- Stage I is an early stage of kidney cancer. The tumor measures up to 2 3/4 inches (7 centimeters). It is no bigger than a tennis ball. The cancer cells are found only in the kidney.
- Stage II is also an early stage of kidney cancer, but the tumor measures more than 2 3/4 inches. The cancer cells are found only in the kidney.
- Stage III is one of the following:
- The tumor does not extend beyond the kidney, but cancer cells have spread through the lymphatic system to one nearby lymph node; or
- The tumor has invaded the adrenal gland or the layers of fat and fibrous tissue that surround the kidney, but cancer cells have not spread beyond the fibrous tissue. Cancer cells may be found in one nearby lymph node; or
- The cancer cells have spread from the kidney to a nearby large blood vessel. Cancer cells may be found in one nearby lymph node.
- Stage IV is one of the following:
- The tumor extends beyond the fibrous tissue that surrounds the kidney; or
- Cancer cells are found in more than one nearby lymph node; or
- The cancer has spread to other places in the body such as the lungs.
-
Recurrent cancer is cancer that has come back (recurred) after treatment. It may come back in the kidney or in another part of the body.
 |
Treatment
Many people with kidney cancer want to take an active part in making decisions about their medical care. They want to learn all they can about their disease and their treatment choices. However, shock and stress after the diagnosis can make it hard to think of everything they want to ask the doctor. It often helps to make a list of questions before an appointment. To help remember what the doctor says, people may take notes or ask whether they may use a tape recorder. Some also want to have a family member or friend with them when they talk to the doctor—to take part in the discussion, to take notes, or just to listen.
The doctor may refer the patient to a specialist, or the patient may ask for a referral. Specialists who treat kidney cancer include doctors who specialize in diseases of the urinary system
(urologists)
and doctors who specialize in cancer
(medical oncologists and
radiation oncologists).
Before starting treatment, a person with kidney cancer might want a second opinion about the diagnosis and the treatment plan. Some insurance companies require a second opinion; others may cover a second opinion if the patient or doctor requests it.
There are a number of ways to find a doctor for a second opinion:
- The patient's doctor may refer the patient to one or more specialists. At cancer centers, several specialists often work together as a team.
- The Cancer Information Service, at 1-800-4-CANCER, can tell callers about nearby treatment centers.
- A local or state medical society, a nearby hospital, or a medical school can usually provide the names of specialists.
- The American Board of Medical Specialties (ABMS)
offers a list of doctors who have met specific
education and training requirements and have
passed a specialty examination. Their
directory—the
Official ABMS Directory of Board Certified Medical Specialists—lists doctors' names along with their specialty and their educational background. The directory is available in most public libraries. Also, ABMS offers this information by telephone and on the Internet. The toll-free telephone number is 1-866-ASK-ABMS (1-866-275-2267). The Internet address is
http://www.abms.org.
- The NCI provides a helpful fact sheet on how to find a doctor called
"How To Find a Doctor or Treatment Facility If You Have Cancer 3." It is available on the Internet at
http://www.cancer.gov/publications.

|
|
Treatment depends mainly on the stage of disease and the patient's general health and age. The doctor can describe treatment choices and discuss the expected results. The doctor and patient can work together to develop a treatment plan that fits the patient's needs.
|
People may want to ask the doctor these questions before treatment begins:
- What is the stage of the disease? Has the cancer spread? If so, where?
- What are my treatment choices? Which do you recommend for me? Will I have more than one kind of treatment?
- What are the expected benefits of each kind of treatment? Will it cure or control the disease?
- What are the risks and possible
side effects
of each treatment? Will I be given anything to control side effects?
- How long will treatment last?
- Will I have to stay in the hospital?
- What is the treatment likely to cost? Is this treatment covered by my insurance plan?
- How will treatment affect my normal activities?
- How often should I have checkups?
- Would a
clinical trial (research study) be appropriate for me?
|
People do not need to ask all their questions or understand all the answers at once. They will have other chances to ask the doctor to explain things that are not clear and to ask for more information.
People with kidney cancer may have
surgery,
arterial embolization,
radiation therapy,
biological therapy, or
chemotherapy. Some may have a combination of treatments.
At any stage of disease, people with kidney cancer may have treatment to control
pain and other symptoms, to relieve the side effects of
therapy, and to ease emotional and practical problems.
This kind of treatment is called
supportive care,
symptom management, or
palliative care.
Information about supportive care is available on NCI's Web site at
http://www.cancer.gov and from NCI's Cancer Information Service at 1-800-4-CANCER.
A patient may want to talk to the doctor about taking part in a clinical trial, a research study of new treatment methods. The section on
"The Promise of Cancer Research 4" has more information about clinical trials.
Surgery is the most common treatment for kidney cancer. It is a type of
local therapy. It treats cancer in the kidney and the area close to the tumor.
An operation to remove the kidney is called a
nephrectomy. There are several types of nephrectomies. The type depends mainly on the stage of the tumor. The doctor can explain each operation and discuss which is most suitable for the patient:
-
Radical nephrectomy: Kidney cancer is usually treated with radical nephrectomy. The
surgeon
removes the entire kidney along with the adrenal gland and some tissue around the kidney. Some lymph nodes in the area also may be removed.
-
Simple nephrectomy: The surgeon removes only the kidney. Some people with Stage I kidney cancer may have a simple nephrectomy.
-
Partial nephrectomy: The surgeon removes only the part of the kidney that contains the tumor. This type of surgery may be used when the person has only one kidney, or when the cancer affects both kidneys. Also, a person with a small kidney tumor (less than 4 centimeters or three-quarters of an inch) may have this type of surgery.
|
People may want to ask the doctor these questions before having surgery:
- What kind of operation do you recommend for me?
- Do I need any lymph nodes removed? Why?
- What are the risks of surgery? Will I have any long-term effects? Will I need dialysis?
- Should I store some of my own blood in case I need a
transfusion?
- How will I feel after the operation?
- How long will I need to stay in the hospital?
- When can I get back to my normal activities?
- How often will I need checkups?
- Would a clinical trial be appropriate for me?
|
Arterial embolization is a type of local therapy that shrinks the tumor. Sometimes it is done before an operation to make surgery easier. When surgery is not possible, embolization may be used to help relieve the symptoms of kidney cancer.
The doctor inserts a narrow tube
(catheter)
into a blood vessel in the leg. The tube is passed up to the main blood vessel
(renal artery)
that supplies blood to the kidney. The doctor injects a substance into the blood vessel to block the flow of blood into the kidney. The blockage prevents the tumor from getting oxygen and other substances it needs to grow.
|
People may want to ask the doctor these questions before having arterial embolization:
- Why do I need this procedure?
- Will I have to stay in the hospital? How long?
- What are the risks and side effects?
- Would a clinical trial be appropriate for me?
|
Radiation therapy (also called
radiotherapy) is another type of local therapy. It uses high-energy rays to kill cancer cells. It affects cancer cells only in the treated area. A large machine directs radiation at the body. The patient has treatment at the hospital or clinic, 5 days a week for several weeks.
A small number of patients have radiation therapy before surgery to shrink the tumor. Some have it after surgery to kill cancer cells that may remain in the area. People who cannot have surgery may have radiation therapy to relieve pain and other problems caused by the cancer.
|
People may want to ask the doctor these questions before having radiation therapy:
- Why do I need this treatment?
- What are the risks and side effects of this treatment?
- Are there any long-term effects?
- When will the treatments begin? When will they end?
- How will I feel during therapy?
- What can I do to take care of myself during therapy?
- Can I continue my normal activities?
- How often will I need checkups?
- Would a clinical trial be appropriate for me?
|
Biological therapy is a type of
systemic therapy.
It uses substances that travel through the bloodstream,
reaching and affecting cells all over the body.
Biological therapy uses the body's natural ability
(immune system)
to fight cancer.
For patients with metastatic kidney cancer, the doctor may suggest interferon alpha or interleukin-2 (also called IL-2 or aldesleukin). The body normally produces these substances in small amounts in response to infections and other diseases. For cancer treatment, they are made in the laboratory in large amounts.
Chemotherapy is also a type of systemic therapy. Anticancer drugs enter the bloodstream and travel throughout the body. Although useful for many other cancers, anticancer drugs have shown limited use against kidney cancer. However, many doctors are studying new drugs and new combinations that may prove more helpful. The section on
"The Promise of Cancer Research 4" has more information about these studies.
|
People may want to ask the doctor these questions before having biological therapy or chemotherapy:
- Why do I need this treatment?
- How does it work?
- What are the expected benefits of the treatment?
- What are the risks and possible side effects of treatment? What can I do about them?
- When will treatment start? When will it end?
- Will I need to stay in the hospital? How long?
- How will treatment affect my normal activities?
- Would a clinical trial be appropriate for me?
|
Side Effects of Cancer Treatment
Because treatment may damage healthy cells and tissues, unwanted side effects are common. These side effects depend mainly on the type and extent of the treatment. Side effects may not be the same for each person, and they may change from one treatment session to the next. Before treatment starts, the health care team will explain possible side effects and suggest ways to help the patient manage them.
The NCI provides helpful booklets about cancer treatments
and coping with side effects, such as
Radiation Therapy and You 5,
Chemotherapy and You 6, and
Eating Hints for Cancer Patients 7.
See the sections
"National Cancer Institute Booklets 8" and
"National Cancer Institute Information Resources 9" for other sources of information about side effects.
It takes time to heal after surgery, and the time needed to recover is different for each person. Patients are often uncomfortable during the first few days. However, medicine can usually control their pain. Before surgery, patients should discuss the plan for pain relief with the doctor or nurse. After surgery, the doctor can adjust the plan if more pain relief is needed.
It is common to feel tired or weak for a while. The health care team watches the patient for signs of kidney problems by monitoring the amount of fluid the patient takes in and the amount of urine produced. They also watch for signs of bleeding, infection, or other problems requiring immediate treatment. Lab tests help the health care team monitor for signs of problems.
If one kidney is removed, the remaining kidney
generally is able to perform the work of both
kidneys. However, if the
remaining kidney is not working well or if
both kidneys are removed,
dialysis is
needed to clean the blood.
For a few patients, kidney
transplantation
may be an option. For this procedure, the transplant surgeon replaces the patient's kidney with a healthy kidney from a donor.
After arterial embolization, some patients have back pain or develop a fever. Other side effects are nausea and vomiting. These problems soon go away.
The side effects of radiation therapy depend mainly on the amount of radiation given and the part of the body that is treated. Patients are likely to become very tired during radiation therapy, especially in the later weeks of treatment. Resting is important, but doctors usually advise patients to try to stay as active as they can.
Radiation therapy to the kidney and nearby areas may cause nausea, vomiting, diarrhea, or urinary discomfort. Radiation therapy also may cause a decrease in the number of healthy white blood cells, which help protect the body against infection. In addition, the skin in the treated area may sometimes become red, dry, and tender. Although the side effects of radiation therapy can be distressing, the doctor can usually treat or control them.
Biological therapy may cause flu-like symptoms, such as chills, fever, muscle aches, weakness, loss of appetite, nausea, vomiting, and diarrhea. Patients also may get a skin rash. These problems can be severe, but they go away after treatment stops.
The side effects of chemotherapy depend mainly on the specific drugs and the amount received at one time. In general, anticancer drugs affect cells that divide rapidly, especially:
- Blood cells: These cells fight infection, help the blood to clot, and carry oxygen to all parts of the body. When drugs affect blood cells, patients are more likely to get infections, may bruise or bleed easily, and may feel very weak and tired.
- Cells in hair roots: Chemotherapy can cause hair loss. The hair grows back, but sometimes the new hair is somewhat different in color and texture.
- Cells that line the digestive tract: Chemotherapy can cause poor appetite, nausea and vomiting, diarrhea, or mouth and lip sores. Many of these side effects can be controlled with drugs.
Nutrition
Patients need to eat well during cancer therapy. They need enough calories to maintain a good weight and protein to keep up strength. Good nutrition often helps people with cancer feel better and have more energy.
But eating well can be difficult. Patients may not feel like eating if they are uncomfortable or tired. Also, the side effects of treatment, such as poor appetite, nausea, or vomiting, can be a problem. Some patients find that foods do not taste as good during cancer therapy.
The doctor, dietitian, or other health care provider
can suggest ways to maintain a healthy diet.
Patients and their families may want to read
the National Cancer Institute booklet
Eating Hints for Cancer Patients 7,
which contains many useful ideas and recipes. The
"National Cancer Institute Booklets 8" section tells how to get this publication.
Follow-up Care
Follow-up care after treatment for kidney cancer is important. Even when the cancer seems to have been completely removed or destroyed, the disease sometimes returns because cancer cells can remain in the body after treatment. The doctor monitors the recovery of the person treated for kidney cancer and checks for recurrence of cancer. Checkups help ensure that any changes in health are noted. The patient may have lab tests, chest x-rays, CT scans, or other tests.
The NCI has prepared a booklet for people who have
completed their treatment to help answer questions
about follow-up care and other concerns.
Facing Forward Series: Life After Cancer Treatment 10
provides tips for making the best
use of medical visits. It describes how to talk
to the doctor about creating a plan of
action for recovery and future health.
Support for People with Kidney Cancer
Living with a serious disease such as kidney cancer is not easy. People with kidney cancer may worry about caring for their families, keeping their jobs, or continuing daily activities. Concerns about treatments and managing side effects, hospital stays, and medical bills are also common. Doctors, nurses, and other members of the health care team can answer questions about treatment, working, or other activities. Meeting with a social worker, counselor, or member of the clergy can be helpful to those who want to talk about their feelings or discuss their concerns. Often, a social worker can suggest resources for financial aid, transportation, home care, or emotional support.
Support groups also can help. In these groups, patients or their family members meet with other patients or their families to share what they have learned about coping with the disease and the effects of treatment. Groups may offer support in person, over the telephone, or on the Internet. Patients may want to talk with a member of their health care team about finding a support group.
The Cancer Information Service at 1-800-4-CANCER can provide information to help patients and their families locate programs, services, and publications.
The Promise of Cancer Research
Doctors all over the country are conducting many types of clinical trials. These are research studies in which people volunteer to take part. In clinical trials, doctors are testing new ways to treat kidney cancer. Research has already led to advances, and researchers continue to search for more effective approaches.
Patients who join these studies have the first chance to benefit from treatments that have shown promise in earlier research. They also make an important contribution to medical science by helping doctors learn more about the disease. Although clinical trials may pose some risks, researchers do all they can to protect their patients.
Researchers are studying surgery,
biological therapy, chemotherapy, and
combinations of these types of treatment.
They also are combining chemotherapy
with new treatments, like
stem cell transplantation.
A
stem cell
transplant allows a patient to be treated with
high doses of drugs. The high doses destroy both cancer cells and normal blood cells in the bone marrow. Later, the patient receives healthy stem cells from a donor. New blood cells develop from the transplanted stem cells.
Other approaches also are under study. For example, researchers are studying cancer vaccines that help the immune system to find and attack kidney cancer cells.
Patients who are interested in being part of a
clinical trial should talk with their doctor.
They may want to read the NCI booklet Taking Part in Cancer Treatment Research Studies 11. It explains how clinical trials are carried out and explains their possible benefits and risks. NCI's Web site includes a section on clinical trials at
http://www.cancer.gov/clinicaltrials with general information about clinical trials and detailed information about specific studies. The Cancer Information Service at
1-800-4-CANCER or at LiveHelp 1 can answer questions and provide information about clinical trials.
National Cancer Institute Booklets
National Cancer Institute (NCI) publications can be ordered by writing to the address below:
Publications Ordering Service
National Cancer Institute
Suite 3036A
6116 Executive Boulevard, MSC 8322
Bethesda, MD 20892-8322
|
Some NCI publications can be viewed, downloaded, and ordered from
http://www.cancer.gov/publications on the Internet. In addition, people in the United States and its territories may order these and other NCI booklets by calling the Cancer Information Service at 1-800-4-CANCER.
See the complete index of What You Need To Know About™ Cancer 12 publications.
National Cancer Institute Information Resources
You may want more information for yourself, your family, and your doctor. The following National Cancer Institute (NCI) services are available to help you.
Cancer Information Service 25 (CIS)
Provides accurate, up-to-date information on cancer to patients and their families, health professionals, and the general public. Information specialists translate the latest scientific information into understandable language and respond in English, Spanish, or on TTY equipment.
Toll-free: 1-800-4-CANCER (1-800-422-6237)
TTY: 1-800-332-8615 (for deaf and hard of hearing callers)
http://www.cancer.gov
The NCI's Cancer.gov™ Web site provides information from numerous NCI sources. It offers current information on cancer prevention, screening, diagnosis, treatment, genetics, supportive care, and ongoing clinical trials. It also provides information about NCI's research programs and funding opportunities, cancer statistics, and the Institute itself.
Cancer.gov also provides live, online assistance through LiveHelp 1. Information specialists are available Monday through Friday from 9:00 AM to 10:00 PM Eastern Time.
|