Community Strategy for Pandemic Influenza Mitigation
February 2007
Contents
I. Executive Summary
II. Introduction
III. Rationale for Proposed Nonpharmaceutical Interventions
IV. Pre-pandemic Planning: the Pandemic Severity Index
V. Use of Nonpharmaceutical Interventions by Severity Category
VI. Triggers for Initiating Use of Nonpharmaceutical Interventions
VII. Duration of Implementation of Nonpharmaceutical Interventions
VIII. Critical Issues for the Use of Nonpharmaceutical Interventions
IX. Assessment of the Public on Feasibility of Implementation and Adherence
X. Planning to Minimize Consequences of Community Mitigation Strategy
XI. Testing and Exercising Community Mitigation Interventions
XII. Research Needs
XIII. Conclusions
XIV. References
XV. Figures
XVI. Tables
XVII. Appendices
Appendix 1. Glossary of Terms
Appendix 2. Interim Guidance Development Process
Appendix 3: WHO Phases of a Pandemic/U.S. Government Stages of a Pandemic
Appendix 4. Pandemic Influenza Community Mitigation Interim Planning Guide for Businesses and Other Employers
Appendix 5. Pandemic Influenza Community Mitigation Interim Planning Guide for Childcare Programs
Appendix 6. Pandemic Influenza Community Mitigation Interim Planning Guide for Elementary and Secondary Schools
Appendix 7. Pandemic Influenza Community Mitigation Interim Planning Guide for Colleges and Universities
Appendix 8. Pandemic Influenza Community Mitigation Interim Planning Guide for Faith-based and Community Organizations
Appendix 9. Pandemic Influenza Community Mitigation Interim Planning Guide for Individuals and Families
I. Executive Summary
Purpose
This document provides interim planning guidance for State, territorial, tribal and local communities that focuses on several measures other than vaccination and drug treatment that might be useful during an influenza pandemic to reduce its harm. Communities, individuals and families, employers, schools, and other organizations will be asked to plan for the use of these interventions to help limit the spread of a pandemic, prevent disease and death, lessen the impact on the economy, and keep society functioning. This interim guidance introduces a Pandemic Severity Index to characterize the severity of a pandemic, provides planning recommendations for specific interventions that communities may use for a given level of pandemic severity, and suggest when these measures should be started and how long they should be used. The interim guidance will be updated when significant new information about the usefulness and feasibility of these approaches emerges.
Introduction
The Centers for Disease Control and Prevention, U.S. Department of Health and Human Services in collaboration with other Federal agencies and partners in the public health, education, business, healthcare, and private sectors, has developed this interim planning guidance on the use of nonpharmaceutical interventions to mitigate an influenza pandemic. These measures may serve as one component of a comprehensive community mitigation strategy that includes both pharmaceutical and nonpharmaceutical measures, and this interim guidance includes initial discussion of a potential strategy for combining the use of antiviral medications with these interventions. This guidance will be updated as new information becomes available that better defines the epidemiology of influenza transmission, the effectiveness of control measures, and the social, ethical, economic, and logistical costs of mitigation strategies. Over time, exercises at the local, State, regional, and Federal level will help define the feasibility of these recommendations and ways to overcome barriers to successful implementation.
The goals of the Federal Government’s response to pandemic influenza are to limit the spread of a pandemic; mitigate disease, suffering, and death; and sustain infrastructure and lessen the impact on the economy and the functioning of society. Without mitigating interventions, even a less severe pandemic would likely result in dramatic increases in the number of hospitalizations and deaths. In addition, an unmitigated severe pandemic would likely overwhelm our nation’s critical healthcare services and impose significant stress on our nation’s critical infrastructure. This guidance introduces, for the first time, a Pandemic Severity Index in which the case fatality ratio (the proportion of deaths among clinically ill persons) serves as the critical driver for characterizing the severity of a pandemic. The severity index is designed to enable better prediction of the impact of a pandemic and to provide local decision-makers with recommendations that are matched to the severity of future influenza pandemics.
It is highly unlikely that the most effective tool for mitigating a pandemic (i.e., a well-matched pandemic strain vaccine) will be available when a pandemic begins. This means that we must be prepared to face the first wave of the next pandemic without vaccine and potentially without sufficient quantities of influenza antiviral medications. In addition, it is not known if influenza antiviral medications will be effective against a future pandemic strain. During a pandemic, decisions about how to protect the public before an effective vaccine is available need to be based on scientific data, ethical considerations, consideration of the public’s perspective of the protective measures and their impact on society, and common sense. Evidence to determine the best strategies for protecting people during a pandemic is very limited. Retrospective data from past influenza pandemics and the conclusions drawn from those data need to be examined and analyzed within the context of modern society. Few of those conclusions may be completely generalizable; however, they can inform contemporary planning assumptions. When these assumptions are integrated into the current mathematical models, the limitations need to be recognized, as they were in a recent Institute of Medicine report (Institute of Medicine. Modeling Community Containment for Pandemic Influenza. A Letter Report. Washington, DC.: The National Academies Press; 2006).
The pandemic mitigation framework that is proposed is based upon an early, targeted, layered application of multiple partially effective nonpharmaceutical measures. It is recommended that the measures be initiated early before explosive growth of the epidemic and, in the case of severe pandemics, that they be maintained consistently during an epidemic wave in a community. The pandemic mitigation interventions described in this document include:
- Isolation and treatment (as appropriate) with influenza antiviral medications of all persons with confirmed or probable pandemic influenza. Isolation may occur in the home or healthcare setting, depending on the severity of an individual’s illness and/or the current capacity of the healthcare infrastructure.
- Voluntary home quarantine of members of households with confirmed or probable influenza case(s) and consideration of combining this intervention with the prophylactic use of antiviral medications, providing sufficient quantities of effective medications exist and that a feasible means of distributing them is in place.
- Dismissal of students from school (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs, coupled with protecting children and teenagers through social distancing in the community to achieve reductions of out-of-school social contacts and community mixing.
- Use of social distancing measures to reduce contact between adults in the community and workplace, including, for example, cancellation of large public gatherings and alteration of workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services. Enable institution of workplace leave policies that align incentives and facilitate adherence with the nonpharmaceutical interventions (NPIs) outlined above.
All such community-based strategies should be used in combination with individual infection control measures, such as hand washing and cough etiquette.
Implementing these interventions in a timely and coordinated fashion will require advance planning. Communities must be prepared for the cascading second- and third-order consequences of the interventions, such as increased workplace absenteeism related to child-minding responsibilities if schools dismiss students and childcare programs close.
Decisions about what tools should be used during a pandemic should be based on the observed severity of the event, its impact on specific subpopulations, the expected benefit of the interventions, the feasibility of success in modern society, the direct and indirect costs, and the consequences on critical infrastructure, healthcare delivery, and society. The most controversial elements (e.g., prolonged dismissal of students from schools and closure of childcare programs) are not likely to be needed in less severe pandemics, but these steps may save lives during severe pandemics. Just as communities plan and prepare for mitigating the effect of severe natural disasters (e.g., hurricanes), they should plan and prepare for mitigating the effect of a severe pandemic.
Rationale for Proposed Nonpharmaceutical Interventions
The use of NPIs for mitigating a community-wide epidemic has three major goals: 1) delay the exponential growth in incident cases and shift the epidemic curve to the right in order to “buy time” for production and distribution of a well-matched pandemic strain vaccine, 2) decrease the epidemic peak, and 3) reduce the total number of incident cases, thus reducing community morbidity and mortality. Ultimately, reducing the number of persons infected is a primary goal of pandemic planning. NPIs may help reduce influenza transmission by reducing contact between sick and uninfected persons, thereby reducing the number of infected persons. Reducing the number of persons infected will, in turn, lessen the need for healthcare services and minimize the impact of a pandemic on the economy and society. The surge of need for medical care that would occur following a poorly mitigated severe pandemic can be addressed only partially by increasing capacity within hospitals and other care settings. Reshaping the demand for healthcare services by using NPIs is an important component of the overall mitigation strategy. In practice, this means reducing the burdens on the medical and public health infrastructure by decreasing demand for medical services at the peak of the epidemic and throughout the epidemic wave; by spreading the aggregate demand over a longer time; and, to the extent possible, by reducing net demand through reduction in patient numbers and case severity.
No intervention short of mass vaccination of the public will dramatically reduce transmission when used in isolation. Mathematical modeling of pandemic influenza scenarios in the United States, however, suggests that pandemic mitigation strategies utilizing multiple NPIs may decrease transmission substantially and that even greater reductions may be achieved when such measures are combined with the targeted use of antiviral medications for treatment and prophylaxis. Recent preliminary analyses of cities affected by the 1918 pandemic show a highly significant association between the early use of multiple NPIs and reductions in peak and overall death rates. The rational targeting and layering of interventions, especially if these can be implemented before local epidemics have demonstrated exponential growth, provide hope that the effects of a severe pandemic can be mitigated. It will be critical to target those at the nexus of transmission and to layer multiple interventions together to reduce transmission to the greatest extent possible.
Pre-Pandemic Planning: the Pandemic Severity Index
This guidance introduces, for the first time, a Pandemic Severity Index, which uses case fatality ratio as the critical driver for categorizing the severity of a pandemic (Figure A, abstracted and reprinted from Figure 4 in the main text). The index is designed to enable estimation of the severity of a pandemic on a population level to allow better forecasting of the impact of a pandemic and to enable recommendations to be made on the use of mitigation interventions that are matched to the severity of future influenza pandemics.
Figure A. Pandemic Severity Index
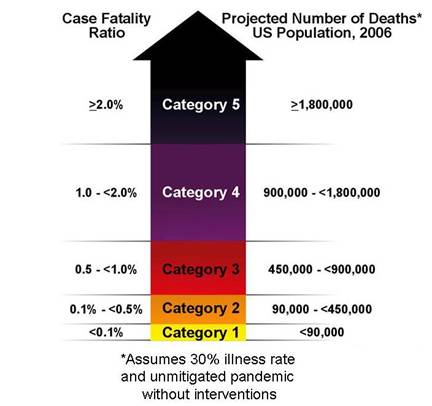
Future pandemics will be assigned to one of five discrete categories of increasing severity (Category 1 to Category 5). The Pandemic Severity Index provides communities a tool for scenario-based contingency planning to guide local pre-pandemic preparedness efforts. Accordingly, communities facing the imminent arrival of pandemic disease will be able to use the pandemic severity assessment to define which pandemic mitigation interventions are indicated for implementation.
Use of Nonpharmaceutical Interventions by Severity Category
This interim guidance proposes a community mitigation strategy that matches recommendations on planning for use of selected NPIs to categories of severity of an influenza pandemic. These planning recommendations are made on the basis of an assessment of the possible benefit to be derived from implementation of these measures weighed against the cascading second- and third-order consequences that may arise from their use. Cascading second- and third-order consequencesarechains of effects that may arise because of the intervention and may require additional planning and intervention to mitigate. The term generally refers to foreseeable unintended consequences of intervention. For example, dismissal of students from school may lead to the second-order effect of workplace absenteeism for child minding. Subsequent workplace absenteeism and loss of household income could be especially problematic for individuals and families living at or near subsistence levels. Workplace absenteeism could also lead to disruption of the delivery of goods and services essential to the viability of the community.
For Category 4 or Category 5 pandemics, a planning recommendation is made for use of all listed NPIs (Table A, abstracted and reprinted here from Table 2 in the main text). In addition, planning for dismissal of students from schools and school-based activities and closure of childcare programs, in combination with means to reduce out-of-school social contacts and community mixing for these children, should encompass up to 12 weeks of intervention in the most severe scenarios. This approach to pre-pandemic planning will provide a baseline of readiness for community response. Recommendations for use of these measures for pandemics of lesser severity may include a subset of these same interventions and potentially for shorter durations, as in the case of social distancing measures for children.
Table A. Summary of the Community Mitigation Strategy by Pandemic Severity
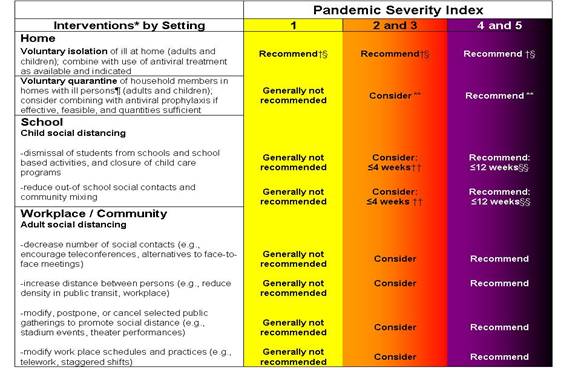
Generally Not Recommended = Unless there is a compelling rationale for specific populations or jurisdictions, measures are generally not recommended for entire populations as the consequences may outweigh the benefits.
Consider = Important to consider these alternatives as part of a prudent planning strategy, considering characteristics of the pandemic, such as age-specific illness rate, geographic distribution, and the magnitude of adverse consequences. These factors may vary globally, nationally, and locally.
Recommended = Generally recommended as an important component of the planning strategy.
*All these interventions should be used in combination with other infection control measures, including hand hygiene, cough etiquette, and personal protective equipment such as face masks. Additional information on infection control measures is available at www.pandemicflu.gov.
†This intervention may be combined with the treatment of sick individuals using antiviral medications and with vaccine campaigns, if supplies are available
§Many sick individuals who are not critically ill may be managed safely at home
¶The contribution made by contact with asymptomatically infected individuals to disease transmission is unclear. Household members in homes with ill persons may be at increased risk of contracting pandemic disease from an ill household member. These household members may have asymptomatic illness and may be able to shed influenza virus that promotes community disease transmission. Therefore, household members of homes with sick individuals would be advised to stay home.
**To facilitate compliance and decrease risk of household transmission, this intervention may be combined with provision of antiviral medications to household contacts, depending on drug availability, feasibility of distribution, and effectiveness; policy recommendations for antiviral prophylaxis are addressed in a separate guidance document.
††Consider short-term implementation of this measure—that is, less than 4 weeks.
§§Plan for prolonged implementation of this measure—that is, 1 to 3 months; actual duration may vary depending on transmission in the community as the pandemic wave is expected to last 6-8 weeks.
Triggers for Initiating Use of Nonpharmaceutical Interventions
The timing of initiation of various NPIs will influence their effectiveness. Implementing these measures prior to the pandemic may result in economic and social hardship without public health benefit and over time, may result in “intervention fatigue” and erosion of public adherence. Conversely, implementing these interventions after extensive spread of pandemic influenza illness in a community may limit the public health benefits of employing these measures. Identifying the optimal time for initiation of these interventions will be challenging because implementation needs to be early enough to preclude the initial steep upslope in case numbers and long enough to cover the peak of the anticipated epidemic curve while avoiding intervention fatigue.
This guidance suggests that the primary activation trigger for initiating interventions be the arrival and transmission of pandemic virus. This trigger is best defined by a laboratory-confirmed cluster of infection with a novel influenza virus and evidence of community transmission (i.e., epidemiologically linked cases from more than one household).
Defining the proper geospatial-temporal boundary for this cluster is complex and should recognize that our connectedness as communities goes beyond spatial proximity and includes ease, speed, and volume of travel between geopolitical jurisdictions (e.g., despite the physical distance, Hong Kong, London, and New York City may be more epidemiologically linked to each other than they are to their proximate rural provinces/areas). In order to balance connectedness and optimal timing, it is proposed that the geopolitical trigger be defined as the cluster of cases occurring within a U.S. State or proximate epidemiological region (e.g., a metropolitan area that spans more than one State’s boundary). It is acknowledged that this definition of “region” is open to interpretation; however, it offers flexibility to State and local decision-makers while underscoring the need for regional coordination in pre-pandemic planning.
From a pre-pandemic planning perspective, the steps between recognition of a pandemic threat and the decision to activate a response are critical to successful implementation. Thus, a key component is the development of scenario-specific contingency plans for pandemic response that identify key personnel, critical resources, and processes. To emphasize the importance of this concept, the guidance section on triggers introduces the terminology of Alert, Standby, and Activate, which reflect key steps in escalation of response action. Alert includes notification of critical systems and personnel of their impending activation, Standby includes initiation of decision-making processes for imminent activation, including mobilization of resources and personnel, and Activate refers to implementation of the specified pandemic mitigation measures. Pre-pandemic planning for use of these interventions should be directed to lessening the transition time between Alert, Standby, and Activate. The speed of transmission may drive the amount of time decision-makers are allotted in each mode, as does the amount of time it takes to fully implement the intervention once a decision is made to Activate.
For the most severe pandemics (Categories 4 and 5), Alert is implemented during WHO Phase 5/U.S. Government Stage 2 (confirmed human outbreak overseas), and Standby is initiated during WHO Phase 6/U.S. Government Stage 3 (widespread human outbreaks in multiple locations overseas). Standby is maintained through Stage 4 (first human case in North America), with the exception of the State or region in which a cluster of laboratory-confirmed human pandemic influenza cases with evidence of community transmission is identified. The recommendation for that State or region is to Activate the appropriate NPIs when identification of a cluster with community transmission is made. Other States or regions Activate appropriate interventions when they identify laboratory-confirmed human pandemic influenza case clusters with evidence of community transmission in their jurisdictions.
For Category 1, 2, and 3 pandemics, Alert is declared during U.S. Government Stage 3, with step-wise progression by States and regions to Standby based on U.S. Government declaration of Stage 4 and the identification of the first human pandemic influenza case(s) in the United States. Progression to Activate by a given State or region occurs when that State or region identifies a cluster of laboratory-confirmed human pandemic influenza cases with evidence of community transmission in their jurisdiction.
Duration of Implementation of Nonpharmaceutical Interventions
It is important to emphasize that as long as susceptible individuals are present in large numbers, disease spread may continue. Immunity to infection with a pandemic strain can only occur after natural infection or immunization with an effective vaccine. Preliminary analysis of historical data from selected U.S. cities during the 1918 pandemic suggests that duration of implementation is significantly associated with overall mortality rates. Stopping or limiting the intensity of interventions while pandemic virus was still circulating within the community was temporally associated with increases in mortality due to pneumonia and influenza in many communities.
It is recommended for planning purposes that communities be prepared to maintain interventions for up to 12 weeks, especially in the case of Category 4 or Category 5 pandemics, where recrudescent epidemics may have significant impact. However, for less severe pandemics (Category 2 or 3), a shorter period of implementation may be adequate for achieving public health benefit. This planning recommendation acknowledges the uncertainty around duration of circulation of pandemic virus in a given community and the potential for recrudescent disease when use of NPIs is limited or stopped, unless population immunity is achieved.
Critical Issues for the Use of Nonpharmaceutical Interventions
A number of outstanding issues should be addressed to optimize the planning for use of these measures. These issues include the establishment of sensitive and timely surveillance, the planning and conducting of multi-level exercises to evaluate the feasibility of implementation, and the identification and establishment of appropriate monitoring and evaluation systems. Policy guidance in development regarding the use of antiviral medications for prophylaxis, community and workplace-specific use of personal protective equipment, and safe home management of ill persons must be prioritized as part of future components of the overall community mitigation strategy. In addition, generating appropriate risk communication content/materials and an effective means for delivery, soliciting active community support and involvement in strategic planning decisions, and assisting individuals and families in addressing their own preparedness needs are critical factors in achieving success.
Assessment of the Public on Feasibility of Implementation and Compliance
A Harvard School of Public Health public opinion poll on community mitigation interventions, conducted with a nationally representative sample of adults over the age of 18 years in the United States in September and October 2006, indicated that most respondents were willing to follow public health recommendations for the use of NPIs, but it also uncovered financial and other concerns. More information on “Pandemic Influenza and the Public: Survey Findings” is available at www.keystone.org/Public_Policy/pandemic_control.html.
The Public Engagement Project on Community Control Measures for Pandemic Influenza (see link at www.keystone.org/Public_Policy/pandemic_control.html), carried out in October and November 2006, found that approximately two-thirds of both citizens and stakeholders supported all the nonpharmaceutical measures. Nearly half of the citizens and stakeholders supported implementation when pandemic influenza first strikes the United States, and approximately one-third of the public supported implementation when influenza first strikes in their State.
Although the findings from the poll and public engagement project reported high levels of willingness to follow pandemic mitigation recommendations, it is uncertain how the public might react when a pandemic occurs. These results need to be interpreted with caution in advance of a severe pandemic that could cause prolonged disruption of daily life and widespread illness in a community. Issues such as the ability to stay home if ill, job security, and income protection were repeatedly cited as factors critical to ensuring compliance with these NPI measures.
Planning to Minimize Consequences of Community Mitigation Strategy
It is recognized that implementing certain NPIs will have an impact on the daily activities and lives of individuals and society. For example, some individuals will need to stay home to mind children or because of exposure to ill family members, and for some children, there will be an interruption in their education or their access to school meal programs. These impacts will arise in addition to the direct impacts of the pandemic itself. Communities should undertake appropriate planning to address both the consequences of these interventions and direct effects of the pandemic. In addition, communities should pre-identify those for whom these measures may be most difficult to implement, such as vulnerable populations and persons at risk (e.g., people who live alone or are poor/working poor, elderly [particularly those who are homebound], homeless, recent immigrants, disabled, institutionalized, or incarcerated). To facilitate preparedness and to reduce untoward consequences from these interventions, Pandemic Influenza Community Mitigation Interim Planning Guideshave been included (see Appendices 4-9) to provide broad planning guidance tailored for businesses and other employers, childcare programs, elementary and secondary schools, colleges and universities, faith-based and community organizations, and individuals and families. It is also critical for communities to begin planning their risk communication strategies. This includes public engagement and messages to help individuals, families, employers, and many other stakeholders to prepare.
The U.S. Government recognizes the significant challenges and social costs that would be imposed by the coordinated application of the measures described above. It is important to bear in mind, however, that if the experience of the 1918 pandemic is relevant, social distancing and other NPI strategies would, in all likelihood, be implemented in most communities at some point during a pandemic. The potential exists for such interventions to be implemented in an uncoordinated, untimely, and inconsistent manner that would impose economic and social costs similar to those imposed by strategically implemented interventions but with dramatically reduced effectiveness. The development of clear interim pre-pandemic guidance for planning that outlines a coordinated strategy, based upon the best scientific evidence available, offers communities the best chance to secure the benefits that such strategies may provide. As States and local communities exercise the potential tools for responding to a pandemic, more will be learned about the practical realities of their implementation. Interim recommendations will be updated accordingly.
Testing and Exercising Community Mitigation Interventions
Since few communities have experienced disasters on the scale of a severe pandemic, drills and exercises are critical in testing the efficacy of plans. A severe pandemic would challenge all facets of governmental and community functions. Advance planning is necessary to ensure a coordinated communications strategy and the continuity of essential services. Realistic exercises considering the effect of these proposed interventions and the cascading second- and third-order consequences will identify planning and resource shortfalls.
Research Needs
It is recognized that additional research is needed to validate the proposed interventions, assess their effectiveness, and identify adverse consequences. This research will be conducted as soon as practicable and will be used in providing updated guidance as required. A proposed research agenda is outlined within this document.
Conclusions
Planning and preparedness for implementing mitigation strategies during a pandemic are complex tasks requiring participation by all levels of government and all segments of society. Community-level intervention strategies will call for specific actions by individuals, families, employers, schools, and other organizations. Building a foundation of community and individual and family preparedness and developing and delivering effective risk communication for the public in advance of a pandemic are critical. If embraced earnestly, these efforts will result in enhanced ability to respond not only to pandemic influenza but also to multiple other hazards and threats. While the challenge is formidable, the consequences of facing a severe pandemic unprepared will be intolerable. This interim pre-pandemic planning guidance is put forth as a step in our commitment to address the challenge of mitigating a pandemic by building and enhancing community resiliency.
II. Introduction
A severe pandemic in a fully susceptible population, such as the 1918 pandemic or one of even greater severity, with limited quantities of antiviral medications and pre-pandemic vaccine represents a worst-case scenario for pandemic planning and preparedness.1 However, because pandemics are unpredictable in terms of timing, onset, and severity, communities must plan and prepare for the spectrum of pandemic severity that could occur. The purpose of this document is to provide interim planning guidance for what are believed currently to be the most effective combinations of pharmaceutical and nonpharmaceutical interventions (NPIs) for mitigating the impact of an influenza pandemic across a wide range of severity scenarios.
The community strategy for pandemic influenza mitigation supports the goals of the Federal Government’s response to pandemic influenza to limit the spread of a pandemic; mitigate disease, suffering, and death; and sustain infrastructure and lessen the impact to the economy and the functioning of society.2 In a pandemic, the overarching public health imperative must be to reduce morbidity and mortality. From a public health perspective, if we fail to protect human health we are likely to fail in our goals of preserving societal function and mitigating the social and economic consequences of a severe pandemic.3-8
A severe pandemic could overwhelm acute care services in the United States and challenge our nation’s healthcare system.9-11 To preserve as many lives as possible, it is essential to keep the healthcare system functioning and to deliver the best care possible.12 The projected peak demand for healthcare services, including intensive care unit (ICU) admissions and the number of individuals requiring mechanical ventilation, would vastly exceed current inventories of physical assets (emergency services capacity, inpatient beds, ICU beds, and ventilators) and numbers of healthcare professionals (nurses and physicians). The most prudent approach, therefore, would appear to be to expand medical surge capacity as much as possible while reducing the anticipated demand for services by limiting disease transmission. Delaying a rapid upswing of cases and lowering the epidemic peak to the extent possible would allow a better match between the number of ill persons requiring hospitalization and the nation’s capacity to provide medical care for such people (see Figure 1).
The primary strategies for combating influenza are 1) vaccination, 2) treatment of infected individuals and prophylaxis of exposed individuals with influenza antiviral medications, and 3) implementation of infection control and social distancing measures.5, 7, 8, 13, 14 The single most effective intervention will be vaccination. However, it is highly unlikely that a well-matched vaccine will be available when a pandemic begins unless a vaccine with broad cross-protection is developed.15-18 With current vaccine technology, pandemic strain vaccine would not become available for at least 4 to 6 months after the start of a pandemic, although this lag time may be reduced in the future. Furthermore, once an effective pandemic vaccine is developed and being produced, it is likely that amounts will be limited due to the production process and will not be sufficient to cover the entire population. Pre-pandemic vaccine may be available at the onset of a pandemic, but there is no guarantee that it will be effective against the emerging pandemic strain. Even if a pre-pandemic vaccine did prove to be effective, projected stockpiles of such a vaccine would be sufficient for only a fraction of the U.S. population.
These realities mean that we must be prepared to face the first wave of the next pandemic without vaccine—the best countermeasure—and potentially without sufficient quantities of influenza antiviral medications.19 In addition, it is not known if influenza antiviral medications will be effective against a future pandemic strain. During a pandemic, decisions about how to protect the public before an effective vaccine is available need to be based on scientific data, ethical considerations, consideration of the public’s perspective of the protective measures and their impact on society, and common sense. Evidence to determine the best strategies for protecting people during a pandemic is very limited. Retrospective data from past epidemics and the conclusions drawn from those data need to be examined and analyzed within the context of modern society. Few of those conclusions may be completely generalizable; however, they can inform contemporary planning assumptions. When these assumptions are integrated into the current mathematical models, the limitations need to be recognized, as they were in a recent Institute of Medicine report.20
This document provides interim pre-pandemic planning guidance for the selection and timing of selected NPIs and recommendations for their use matched to the severity of a future influenza pandemic. While it is not possible, prior to emergence, to predict with certainty the severity of a pandemic, early and rapid characterization of the virus and initial clusters of human cases may give insight into its potential severity and determine the initial public health response. The main determinant of a pandemic’s severity is its associated mortality.21-27 This may be defined by case fatality ratio or excess mortality rate—key epidemiological parameters that may be available shortly after the emergence of a pandemic strain from investigations of initial outbreaks or from more routine surveillance data. Other factors, such as efficiency of transmission, are important for consideration as well.
The Centers for Disease Control and Prevention (CDC) developed this guidance with input from other Federal agencies, key stakeholders, and partners, including a working group of public health officials and other stakeholders (seeAppendix 2, Interim Guidance Development Process). A community mitigation framework is proposed that is based upon an early, targeted, layered mitigation strategy involving the directed application of multiple partially effective nonpharmaceutical measures initiated early and maintained consistently during an epidemic wave.20, 28-33 These interventions include the following:
- Isolation and treatment (as appropriate) with influenza antiviral medications of all persons with confirmed or probable pandemic influenza. Isolation may occur in the home or healthcare setting, depending on the severity of an individual’s illness and/or the current capacity of the healthcare infrastructure.
- Voluntary home quarantine of members of households with confirmed or probable influenza case(s) and consideration of combining this intervention with the prophylactic use of antiviral medications, providing sufficient quantities of effective medications exist and that a feasible means of distributing them is in place.
- Dismissal of students from school (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs, coupled with protecting children and teenagers through social distancing in the community to achieve reductions of out-of-school social contacts and community mixing.
- Use of social distancing measures to reduce contact among adults in the community and workplace, including, for example, cancellation of large public gatherings and alteration of workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services. Enable institution of workplace leave policies that align incentives and facilitate adherence with the nonpharmaceutical interventions (NPIs) outlined above.
The effectiveness of individual infection control measures (e.g., cough etiquette, hand hygiene) and the role of surgical masks or respirators in preventing the transmission of influenza are currently unknown. However, cough etiquette and hand hygiene will be recommended universally, and the use of surgical masks and respirators may be appropriate in certain settings (specific community face mask and respirator use guidance is forthcoming as is guidance for workplaces and will be available on www.pandemicflu.gov).
Decisions about what tools should be used during a pandemic should be based on the observed severity of the event, its impact on specific subpopulations, the expected benefit of the interventions, the feasibility of success in modern society, the direct and indirect costs, and the consequences on critical infrastructure, healthcare delivery, and society. The most controversial elements (e.g., prolonged dismissal of students from schools and closure of childcare programs) are not likely to be needed in less severe pandemics, but these steps may save lives during severe pandemics. Just as communities plan and prepare for mitigating the effect of severe natural disasters (e.g., hurricanes), they should plan and prepare for mitigating the effect of a severe pandemic.
The U.S. Government recognizes the significant challenges and social costs that would be imposed by the coordinated application of the measures described above. 2, 10, 34 It is important to bear in mind, however, that if the experience of the 1918 pandemic is relevant, social distancing and other NPI strategies would, in all likelihood, be implemented in most communities at some point during a pandemic. The potential exists for such interventions to be implemented in an uncoordinated, untimely, and inconsistent manner that would impose economic and social costs similar to those imposed by strategically implemented interventions but with dramatically reduced effectiveness. The development of clear interim pre-pandemic guidance for planning that outlines a coordinated strategy, based upon the best scientific evidence available, offers communities the best chance to secure the benefits that such strategies may provide. As States and local communities exercise the potential tools for responding to a pandemic, more will be learned about the practical realities of their implementation. Interim recommendations will be updated accordingly.
This document serves as interim public health planning guidance for State, local, territorial, and tribal jurisdictions developing plans for using community mitigation interventions in response to a potential influenza pandemic in the United States. Given the paucity of evidence for the effectiveness of some of the interventions and the potential socioeconomic implications, some interventions may draw considerable disagreement and criticism.20 Some interventions that may be highly useful tools in the framework of a disease control strategy will need to be applied judiciously to balance socioeconomic realities of community functioning. CDC will regularly review this document and, as appropriate, issue updates based on the results from various ongoing historical, epidemiological, and field studies. Response guidance will need to remain flexible and likely will require modification during a pandemic as information becomes available and it can be determined if ongoing pandemic mitigation measures are useful for mitigating the impact of the pandemic. Pandemic planners need to develop requirements for community-level data collection during a pandemic and develop and test a tool or process for accurate real-time and post-wave evaluation of pandemic mitigation measures, with guidelines for modifications.
Communities will need to prepare in advance if they are to accomplish the rapid and coordinated introduction of the measures described while mitigating the potentially significant cascading second- and third-order consequences of the interventions themselves. Cascading second- and third-order consequencesarechains of effects that may arise because of the intervention and may require additional planning and intervention to mitigate. The terms generally refer to foreseeable unintended consequences of intervention. For example, dismissal of students from school classrooms may lead to the second-order effect of workplace absenteeism for child minding. Subsequent workplace absenteeism and loss of household income could be especially problematic for individuals and families living at or near subsistence levels. Workplace absenteeism could also lead to disruption of the delivery of goods and services essential to the viability of the community. If communities are not prepared for these untoward effects, the ability of the public to comply with the proposed measures and, thus, the ability of the measures to reduce suffering and death may be compromised.
Federal, State, local, territorial, and tribal governments and the private sector all have important and interdependent roles in preparing for, responding to, and recovering from a pandemic. To maintain public confidence and to enlist the support of private citizens in disease mitigation efforts, public officials at all levels of government must provide unambiguous and consistent guidance that is useful for planning and can assist all segments of society to recognize and understand the degree to which their collective actions will shape the course of a pandemic. The potential success of community mitigation interventions is dependent upon building a foundation of community and individual and family preparedness. To facilitate preparedness, Pandemic Influenza Community Mitigation Interim Planning Guideshave been included as appendices to provide broad but tailored planning guidance for businesses and other employers, childcare programs, elementary and secondary schools, colleges and universities, faith-based and community organizations, and individuals and families (see Appendices 4-9). See also the Department of Homeland Security’s Pandemic Influenza Preparedness, Response and Recovery Guide for Critical Infrastructure and Key Resources (available at www.pandemicflu.gov/plan/pdf/cikrpandemicinfluenzaguide.pdf).
U.S. and Global Preparedness Planning
The suggested strategies contained in this document are aligned with the World Health Organization (WHO) phases of a pandemic.35 WHO has defined six phases, occurring before and during a pandemic, that are linked to the characteristics of a new influenza virus and its spread through the population (see Appendix 2. WHO Phases of a Pandemic/U.S. Government Stages of a Pandemic). This document specifically provides pre-pandemic planning guidance for the use of NPIs in WHO Phase 6. These phases are described below:
Inter-Pandemic Period
Phase 1: No new influenza virus subtypes have been detected in humans. An influenza virus subtype that has caused human infection may be present in animals. If present in animals, the risk of human disease is considered to be low.
Phase 2: No new influenza virus subtypes have been detected in humans. However, a circulating animal influenza virus subtype poses a substantial risk of human disease.
Pandemic Alert Period
Phase 3: Human infection(s) with a new subtype, but no human-to-human spread, or at most rare instances of spread to a close contact.
Phase 4: Small cluster(s) with limited human-to-human transmission but spread is highly localized, suggesting that the virus is not well adapted to humans.
Phase 5: Larger cluster(s) but human-to-human spread still localized, suggesting that the virus is becoming increasingly better adapted to humans, but may not yet be fully transmissible (substantial pandemic risk).
Pandemic Period
Phase 6: Pandemic phase: increased and sustained transmission in general population.
The WHO phases provide succinct statements about the global risk for a pandemic and provide benchmarks against which to measure global response capabilities. However, to describe the U.S. Government’s approach to the pandemic response, it is more useful to characterize the stages of an outbreak in terms of the immediate and specific threat a pandemic virus poses to the U.S. population.2 The following stages provide a framework for Federal Government actions:
Stage 0: New Domestic Animal Outbreak in At-Risk Country
Stage 1: Suspected Human Outbreak Overseas
Stage 2: Confirmed Human Outbreak Overseas
Stage 3: Widespread Human Outbreaks in Multiple Locations Overseas
Stage 4: First Human Case in North America
Stage 5: Spread throughout United States
Stage 6: Recovery and Preparation for Subsequent Waves
Using the Federal Government’s approach, this document provides pre-pandemic planning guidance from Stages 3 through 5 for step-wise escalation of activity, from pre-implementation preparedness, through active preparation for initiation of NPIs, to actual use.
III. Rationale for Proposed Nonpharmaceutical Interventions
The three major goals of mitigating a community-wide epidemic through NPIs are 1) delay the exponential increase in incident cases and shift the epidemic curve to the right in order to “buy time” for production and distribution of a well-matched pandemic strain vaccine, 2) decrease the epidemic peak, and 3) reduce the total number of incident cases and, thus, reduce morbidity and mortality in the community (Figure 1). These three major goals of epidemic mitigation may all be accomplished by focusing on the single goal of saving lives by reducing transmission. NPIs may help reduce influenza transmission by reducing contact between sick persons and uninfected persons, thereby reducing the number of infected persons. Reducing the number of persons infected will also lessen the need for healthcare services and minimize the impact of a pandemic on the economy and society. The surge of need for medical care associated with a poorly mitigated severe pandemic can be only partially addressed by increasing capacity within hospitals and other care settings. Thus, reshaping the demand for healthcare services by using NPIs is an important component of the overall strategy for mitigating a severe pandemic
Principles of Disease Transmission
Decreasing the Basic Reproductive number, R0
The basic reproductive number, R0, is the average number of new infections that a typical infectious person will produce during the course of his/her infection in a fully susceptible population in the absence of interventions.36-38 R0 is not an intrinsic property of the infectious agent but is rather an epidemic characteristic of the agent acting within a specific host within a given milieu. For any given duration of infection and contact structure, R0 provides a measure of the transmissibility of an infectious agent. Alterations in the pathogen, the host, or the contact networks can result in changes in R0 and thus in the shape of the epidemic curve. Generally speaking, as R0 increases, epidemics have a sharper rise in the case curve, a higher peak illness rate (clinical attack rate), a shorter duration, and a higher percentage of the population infected before the effects of herd immunity begin to exert an influence (in homogeneous contact networks, herd immunity effects should dominate when the percentage of the population infected or otherwise rendered immune is equivalent to 1 – 1/ R0). Rt is the change in the reproductive number at a given point in time. Thus, as shown in Figure 2, decreasing Rt by decreasing host susceptibility (through vaccination or the implementation of individual infection control measures) or reducing transmission by diminishing the number of opportunities for exposure and transmission (through the implementation of community-wide NPIs) will achieve the three major goals of epidemic mitigation.39 Mathematical modeling of pandemic influenza scenarios in the United States suggests that pandemic mitigation strategies utilizing NPIs separately and in combination with medical countermeasures may decrease the Rt.20, 28-31, 40 This potential to reduce Rt is the rationale for employing early, targeted, and layered community-level NPIs as key components of the public health response.
Influenza: Infectiousness and Transmissibility
Assuming the pandemic influenza strain will have transmission dynamics comparable to those for seasonal influenza and recent pandemic influenza strains, the infection control challenges posed will be considerable. Factors responsible for these challenges include 1) a short incubation period (average of 2 days, range 1-4 days); 2) the onset of viral shedding (and presumably of infectiousness) prior to the onset of symptoms; and 3) the lack of specific clinical signs and symptoms that can reliably discriminate influenza infections from other causes of respiratory illness.41, 42 Although the hallmarks of a pandemic strain will not be known until emergence, patients with influenza may shed virus prior to the onset of clinical symptoms and may be infectious on the day before illness onset. Most people infected with influenza develop symptomatic illness (temperature of 100.4° F or greater, plus cough or sore throat), and the amount of virus they shed correlates with their temperature; however, as many as one-third to one-half of those who are infected may either have very mild or asymptomatic infection. This possibility is important because even seemingly healthy individuals with influenza infection as well as those with mild symptoms who are not recognized as having influenza could be infectious to others.
Early, Targeted Implementation of Interventions
The potential for significant transmission of pandemic influenza by asymptomatic or minimally symptomatic individuals to their contacts suggests that efforts to limit community transmission that rely on targeting only symptomatic individuals would result in diminished ability to mitigate the effects of a pandemic. Additionally, the short intergeneration time of influenza disease suggests that household members living with an ill individual (who are thus at increased risk of infection with pandemic virus) would need to be identified rapidly and targeted for appropriate intervention to limit community spread.20, 28-31, 40 Recent estimates have suggested that while the reproductive number for most strains of influenza is less than 2, the intergeneration time may be as little as 2.6 days. These parameters predict that in the absence of disease mitigation measures, the number of cases of epidemic influenza will double about every 3 days, or about a tenfold increase every 1-2 weeks. Given the potential for exponential growth of a pandemic, it is reasonable to expect that the timing of interventions will be critical. Planning for community response that is predicated on reactive implementation of these measures may limit overall effectiveness. Measures instituted earlier in a pandemic would be expected to be more effective than the same measures instituted after a pandemic is well established. Although subject to many limitations, mathematical models that explored potential source mitigation strategies that make use of vaccine, antiviral medications, and other infection control and social distancing measures for use in an influenza outbreak identified critical time thresholds for success.20, 28, 31 These results suggest that the effectiveness of pandemic mitigation strategies will erode rapidly as the cumulative illness rate prior to implementation climbs above 1 percent of the population in an affected area. Thus, pre-pandemic, scenario-based contingency planning for the early, targeted use of NPIs likely provides the greatest potential for an effective public health response.
To summarize, isolation of ill individuals will reduce the onward transmission of disease after such individuals are identified. However, influenza is a disease in which infected persons may shed virus prior to onset of symptoms and thus are potentially infectious for approximately 1 day before becoming symptomatic. In addition, not all infected individuals will be identified because mild or asymptomatic cases may be relatively common. Isolation strategies are thus, at best, a partial solution. Similarly, voluntary quarantine of members of households with ill persons will facilitate the termination of transmission chains, but quarantine strategies are limited to the extent that they can be implemented only after cases are identified. Consequently, only a percentage of transmission chains will be interrupted in this fashion. Given the very short generation times (time between a primary and secondary case) observed with influenza and the fact that peak infectiousness occurs around the time of symptom onset, the identification of cases and simultaneous implementation of isolation and quarantine must occur very rapidly or the efficacy of these strategies will erode significantly.
Antiviral Therapy/Prophylaxis
Four approved influenza antiviral agents are available in the United States: amantadine, rimantadine, zanamivir, and oseltamivir. The role of influenza antiviral medications as therapy for symptomatic individuals is primarily to improve individual outcomes not to limit the further transmission of disease; although, recent clinical trials have demonstrated that prophylaxis of household contacts of symptomatic individuals with neuraminidase inhibitors can reduce household transmission. 43-48
Current antiviral medication stockpiles are thought to be inadequate to support antiviral prophylaxis of members of households with ill individuals.49, 50 Moreover, the feasibility of rapidly (within 48 hours after exposure) providing these medications to ill individuals and those who live in household with ill individuals has not been tested and mechanisms to support such distribution need to be developed. As with the use of antiviral medications for treatment, concerns exist regarding the emergence of resistance if the use of antiviral medications for prophylaxis is widespread.51, 52 Although mathematical models illustrate the additive effects that antiviral prophylaxis offers in reducing disease transmission, these challenges must be addressed to make this a realistic measure for implementation during a pandemic.20 Future updates of this guidance will address feasibility concerns and incorporate any new recommendations regarding use of antiviral prophylaxis for members of households with ill individuals.
Targeting Interventions by Exploiting Heterogeneities in Disease Transmission
Our social connectedness provides a disease transmission network for a pandemic to spread.50, 53-58 Variation exists with respect to individual social connectedness and contribution to disease transmission. Such a distribution is characteristic of a “scale-free” network. A scale-free network is one in which connectivity between nodes follows a distribution in which there are a few highly connected nodes among a larger number of less connected nodes. Air travel provides an example of this concept. In this example, a relatively small number of large hub airports are highly connected with large numbers of originating and connecting flights from a much larger number of small regional airports with a limited number of flights and far lesser degree of connectedness to other airports. Because of the differences in connectivity, the closure of a major hub airport, compared with closure of a small regional airport, would have a disproportionately greater affect on air travel. Given the variation of social connectedness and its contribution to the formation of disease transmission networks, it is useful to identify the nodes of high connectivity since eliminating transmission at these nodes could most effectively reduce disease transmission.
Social Density
One measure for decreasing transmission of an influenza virus is by increasing the distances among people in work, community, and school settings.31, 50, 59 Schools and pre-schools represent the most socially dense of these environments. Social density is greatest in pre-school classrooms, with guidelines for occupancy density specifying 35-50 square feet per child.60, 61 Published criteria for classroom size based upon the number of students and one teacher recommend an elementary school and high school classroom density of 49 and 64 square feet per person, respectively.62 There is more space per person in work and healthcare settings, with high variability from one setting to another; for example, occupancy density in hospitals is about 190 square feet per person.63 Office buildings and large retail buildings have an average occupational density of 390-470 square feet per person.64, 65 Homes represent the least socially dense environment (median occupancy density of 734 square feet per person in single-family homes).66
Public transportation, including subways and transit buses, represents another socially dense environment. There were on average 32.8 million unlinked passenger trips each weekday for all public transportation across the United States in 2004—nearly 20 million of which were by bus.67 More than half these 32.8 million passenger trips are work related (54 percent) and about 15 percent of these trips are school related.68 Each day, 144,000 public transit vehicles, including 81,000 buses, are in use.
More than half the children attending school (K-12) in the United States travel on a school bus—that equates to an estimated 58 million person trips daily (to school and back home).69 The number of schoolchildren traveling via school bus and via public transportation during a school day is twice the number of people taking all public transportation in the United States in terms of number of trips and number of individuals during a weekday.
Targeting Schools, Childcare, and Children
Biological, social, and maturational factors make children especially important in the transmission of influenza. Children without pre-existing immunity to circulating influenza viruses are more susceptible than adults to infection and, compared with adults, are responsible for more secondary transmission within households.70, 71 Compared with adults, children usually shed more influenza virus, and they shed virus for a longer period. They also are not skilled in handling their secretions, and they are in close proximity with many other children for most of the day at school. Schools, in particular, clearly serve as amplification points of seasonal community influenza epidemics, and children are thought to play a significant role in introducing and transmitting influenza virus within their households.20, 27, 70-76, 78 A recent clinical trial demonstrated that removing a comparatively modest number of school children from the transmission pool through vaccination (vaccinating 47 percent of students with a live attenuated vaccine whose efficacy was found in a separate trial, to be no greater than 57 percent) resulted in significant reductions in influenza-related outcomes in households of children (whether vaccinated or unvaccinated) attending intervention schools. 77
Therefore, given the disproportionate contribution of children to disease transmission and epidemic amplification, targeting their social networks both within and outside of schools would be expected to disproportionately disrupt influenza spread. Given that children and teens are together at school for a significant portion of the day, dismissal of students from school could effectively disrupt a significant portion of influenza transmission within these age groups. There is evidence to suggest that school closure can in fact interrupt influenza spread. While the applicability to a U.S. pandemic experience is not clear, nationwide school closure in Israel during an influenza epidemic resulted in significant decreases in the diagnoses of respiratory infections (42 percent), visits to physicians (28 percent) and emergency departments (28 percent), and medication purchases (35 percent).56 The New York City Department of Health and Mental Hygiene recently examined the impact of routine school breaks (e.g., winter break) on emergency department visits for influenza-like illness from 2001 to 2006. Emergency department visits for complaints of febrile illness among school-age children (aged 5 to 17 years) typically declined starting 2-3 days after a school break began, remained static during the school break, and then increased within several days after school recommenced. A similar pattern was not seen in the adult age group.78
Dismissal of students from school could eliminate a potential amplifier of transmission. However, re-congregation and social mixing of children at alternate settings could offset gains associated with disruption of their social networks in schools. For this reason, dismissal of students from schools and, to the extent possible, protecting children and teenagers through social distancing in the community, to include reductions of out-of-school social contacts and community mixing, are proposed as a bundled strategy for disrupting their social networks and, thus, the associated disease transmission pathways for this age group.79
Targeting Adults—Social Distancing at Work and in the Community
Eliminating schools as a focus of epidemic amplification and reducing the social contacts for children and teens outside the home will change the locations and dynamics of influenza virus transmission. The social compartments within which the majority of disease transmission will likely take place will be the home and workplace, and adults will play a more important role in sustaining transmission chains.20, 53, 73 Disrupting adult-to-adult transmission will offer additional opportunities to suppress epidemic spread. The adoption by individuals of infection control measures, such as hand hygiene and cough etiquette, in the community and workplace will be strongly encouraged.
In addition, adults may further decrease their risk of infection by practicing social distancing and minimizing their non-essential social contacts and exposure to socially dense environments. Low-cost and sustainable social distancing strategies can be adopted by individuals within their community (e.g., going to the grocery store once a week rather than every other day, avoiding large public gatherings) and at their workplace (e.g., spacing people farther apart in the workplace, teleworking when feasible, substituting teleconferences for meetings) for the duration of a community outbreak. Employers will be encouraged to establish liberal/unscheduled leave policies, under which employees may use available paid or unpaid leave without receiving prior supervisory approval so that workers who are ill or have ill family members are excused from their responsibilities until their or their family members’ symptoms have resolved. In this way, the amount of disease transmission that occurs in the workplace can be minimized, making the workplace a safer environment for other workers.
Healthcare workers may be prime candidates for targeted antiviral prophylaxis once supplies of the drugs are adequate to support this use. Moreover, beyond the healthcare arena, employers who operate or contract for occupational medical services could consider a cache of antiviral drugs in anticipation of a pandemic and provide prophylactic regimens to employees who work in critical infrastructure businesses, occupy business-critical roles, or hold jobs that put them at repeated high risk of exposure to the pandemic virus. This use of antiviral drugs may be considered for inclusion in a comprehensive pandemic influenza response and may be coupled with NPIs. Strategies ensuring workplace safety will increase worker confidence and may discourage unnecessary absenteeism.
Value of Partially Effective Layered Interventions
Pandemic mitigation strategies generally include 1) case containment measures, such as voluntary case isolation, voluntary quarantine of members of households with ill persons, and antiviral treatment/prophylaxis; 2) social distancing measures, such as dismissal of students from classrooms and social distancing of adults in the community and at work; and 3) infection control measures, including hand hygiene and cough etiquette. Each of these interventions may be only partially effective in limiting transmission when implemented alone.
To determine the usefulness of these partially effective measures alone and in combination, mathematical models were developed to assess these types of interventions within the context of contemporary social networks. The “Models of Infectious Disease Agents Study” (MIDAS), funded by the National Institutes of Health, has been developing agent-based computer simulations of pandemic influenza outbreaks with various epidemic parameters, strategies for using medical countermeasures, and patterns of implementation of community-based interventions (case isolation, household quarantine, child and adult social distancing through school or workplace closure or restrictions, and restrictions on travel).20, 28-30, 32, 39, 40
Mathematical modeling conducted by MIDAS participants demonstrates general consistency in outcome for NPIs and suggests the following within the context of the model assumptions:
- Interventions implemented in combination, even with less than complete levels of public compliance, are effective in reducing transmission of pandemic influenza virus, particularly for lower values of R0.
- School closure and generic social distancing are important components of a community mitigation strategy because schools and workplaces are significant compartments for transmission.
- Simultaneous implementation of multiple tools that target different compartments for transmission is important in limiting transmission because removing one source of transmission may simply make other sources relatively more important.
- Timely intervention may reduce the total number of persons infected with pandemic influenza.
Each of the models generally suggest that a combination of targeted antiviral medications and NPIs can delay and flatten the epidemic peak, but the degree to which they reduce the overall size of the epidemic varies. Delay of the epidemic peak is critically important because it allows additional time for vaccine development and antiviral production. However, these models are not validated with empiric data and are subject to many limitations.20
Supporting evidence for the role of combinations of NPIs in limiting transmission can also be found in the preliminary results from several historical analyses.20 One statistical model being developed based on analysis of historical data for the use of various combinations of selected NPIs in U.S. cities during the 1918 pandemic demonstrates a significant association between early implementation of these measures by cities and reductions in peak death rate.80, 81
Taken together, these strands of evidence are consistent with the hypothesis that there may be benefit in limiting or slowing the community transmission of a pandemic virus by the use of combinations of partially effective NPIs. At the present time, this hypothesis remains unproven, and more work is needed before its validity can be established.
IV. Pre-pandemic Planning: the Pandemic Severity Index
Appropriate matching of the intensity of intervention to the severity of a pandemic is important to maximize the available public health benefit that may result from using an early, targeted, and layered strategy while minimizing untoward secondary effects. To assist pre-pandemic planning, this interim guidance introduces the concept of a Pandemic Severity Index based primarily on case fatality ratio 23-27, a measurement that is useful in estimating the severity of a pandemic on a population level and which may be available early in a pandemic for small clusters and outbreaks. Excess mortality rate may also be available early and may supplement and inform the determination of the Pandemic Severity Index.82 Pandemic severity is described within five discrete categories of increasing severity (Category 1 to Category 5). Other epidemiologic features that are relevant in overall analysis of mitigation plans include total illness rate, age-specific illness and mortality rates, the reproductive number, intergeneration time, and incubation period. However, it is unlikely that estimates will be available for most of these parameters during the early stages of a pandemic; thus, they are not as useful from a planning perspective.
The Pandemic Severity Index provides U.S. communities a tool for scenario-based contingency planning to guide pre-pandemic planning efforts. Upon declaration by WHO of having entered the Pandemic Period (Phase 6) and further determination of U.S. Government Stage 3, 4, or 5, the CDC’s Director shall designate the category of the emerging pandemic based on the Pandemic Severity Index and consideration of other available information. Pending this announcement, communities facing the imminent arrival of pandemic disease will be able to define which pandemic mitigation interventions are most indicated for implementation based on the level of pandemic severity.
Multiple parameters may ultimately provide a more complete characterization of a pandemic. The age-specific and total illness and mortality rates, reproductive number, intergeneration time, and incubation period as well as population structure and healthcare infrastructure are important factors in determining pandemic impact. Although many factors may influence the outcome of an event, it is reasonable to maintain a single criterion for classification of severity for the purposes of guiding contingency planning. If additional epidemiologic characteristics become well established during the course of the next pandemic through collection and analysis of surveillance data, then local jurisdictions may develop a subset of scenarios, depending upon, for example, age-specific mortality rates.
Table 1 provides a categorization of pandemic severity by case fatality ratio—the key measurement in determining the Pandemic Severity Index—and excess mortality rate. In addition, Table 1 displays ranges of illness rates with potential numbers of U.S. deaths per category, with recent U.S. pandemic experience and U.S. seasonal influenza to provide historical context. Figure 3a plots prior U.S. pandemics from the last century and a severe seasonal influenza season based on case fatality ratio and illness rate and demonstrates the great variability in pandemics based on these parameters (and the clear distinctiveness of pandemics from even a severe influenza season). Figure 3b demonstrates that the primary factor determining pandemic severity is case fatality ratio. Incremental increases in case fatality ratio result in proportionally greater mortality in comparison to increasing illness rates, which result in proportionally much smaller increases in mortality. Figure 4 provides a graphic depiction of the Pandemic Severity Index by case fatality ratio, with ranges of projected U.S. deaths at a constant 30 percent illness rate and without mitigation by any intervention.
Data on case fatality ratio and excess mortality in the early course of the next pandemic will be collected during outbreak investigations of initial clusters of human cases, and public health officials may make use of existing influenza surveillance systems once widespread transmission starts. However, it is possible that at the onset of an emerging pandemic, very limited information about cases and deaths will be known. Efforts now to develop decision algorithms based on partial data and efforts to improve global surveillance systems for influenza are needed.
V. Use of Nonpharmaceutical Interventions by Pandemic Severity Category
This section provides interim pre-pandemic planning recommendations for use of pandemic mitigation interventions to limit community transmission. These planning recommendations are likely to evolve as more information about their effectiveness and feasibility becomes available. To minimize economic and social costs, it will be important to judiciously match interventions to the pandemic severity level. However, at the time of an emerging pandemic, depending on the location of the first detected cases, there may be scant information about the number of cases and deaths resulting from infection with the virus. Although surveillance efforts may initially only detect the “herald” cases, public health officials may choose to err on the side of caution and implement interventions based on currently available data and iteratively adjust as more accurate and complete data become available. These pandemic mitigation measures include the following:
- Isolation and treatment (as appropriate) with influenza antiviral medications of all persons with confirmed or probable pandemic influenza. Isolation may occur in the home or healthcare setting, depending on the severity of the individual’s illness and/or the current capacity of the healthcare infrastructure.
- Voluntary home quarantine of members of households with confirmed or probable influenza case(s) and consideration of combining this intervention with the prophylactic use of antiviral medications, providing sufficient quantities of effective medications exist and that a feasible means of distributing them is in place.
- Dismissal of students from schools (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs, coupled with protecting children and teenagers through social distancing in the community to achieve reductions of out-of-school social contacts and community mixing.
- Use of social distancing measures to reduce contact between adults in the community and workplace, including, for example, cancellation of large public gatherings and alteration of workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services. Enable institution of workplace leave policies that align incentives and facilitate adherence with the nonpharmaceutical interventions (NPIs) outlined above.
Planning for use of these NPIs is based on the Pandemic Severity Index, which may allow more appropriate matching of the interventions to the magnitude of the pandemic. These recommendations are summarized in Table 2. All interventions should be combined with infection control practices, such as good hand hygiene and cough etiquette. In addition, the use of personal protective equipment, such as surgical masks or respirators, may be appropriate in some cases, and guidance on community face mask and respirator use will be forthcoming. Guidance on infection control measures, including those for workplaces, may be accessed at www.pandemicflu.gov.
For Category 4 or Category 5 pandemics, a planning recommendation is made for use of all listed NPIs (Table 2). In addition, planning for dismissal of students from schools and school-based activities and closure of childcare programs, in combination with means to reduce out-of-school social contacts and community mixing for these children, should encompass up to 12 weeks of intervention in the most severe scenarios. This approach to pre-pandemic planning will provide a baseline of readiness for community response even if the actual response is shorter. Recommendations for use of these measures for pandemics of lesser severity may include a subset of these same interventions and, possibly, suggestions that they be used for shorter durations, as in the case of the social distancing measures for children.
For Category 2 or Category 3 pandemics, planning for voluntary isolation of ill persons is recommended, whereas other measures (voluntary quarantine of household contacts, social distancing measures for children and adults) are to be implemented only if local decision-makers have determined that characteristics of the pandemic in their community warrant these additional mitigation measures. However, within these categories, pre-pandemic planning for social distancing measures for children should be undertaken with a focus on a duration of 4 weeks or less, distinct from the longer timeframe recommended for pandemics with a greater Pandemic Severity Index. For Category 1 pandemics, only voluntary isolation of ill persons is recommended on a community-wide basis, although local communities may still choose to tailor their response to Category 1-3 pandemics differently by applying NPIs on the basis of local epidemiologic parameters, risk assessment, availability of countermeasures, and consideration of local healthcare surge capacity. Thus, from a pre-pandemic planning perspective for Category 1, 2, and 3 pandemics, capabilities for both assessing local public health capacity and healthcare surge, delivering countermeasures, and implementing these measures in full and in combination should be assessed.
Nonpharmaceutical Interventions
Voluntary Isolation of Ill Persons
The goal of this intervention is to reduce transmission by reducing contact between persons who are ill and those who are not. Ill individuals not requiring hospitalization would be requested to remain at home voluntarily for the infectious period, approximately 7-10 days after symptom onset. This would usually be in their homes, but could be in a home of a friend or relative. Voluntary isolation of ill children and adults at home is predicated on the assumption that many ill individuals who are not critically ill can and will need to be cared for in the home. In addition, this intervention may be combined with the use of influenza antiviral medications for treatment (as appropriate), as long as such medications are effective and sufficient in quantity and that feasible plans and protocols for distribution are in place.
Requirements for success include prompt recognition of illness, appropriate use of hygiene and infection control practices in the home setting (specific guidance is forthcoming and will be available on www.pandemicflu.gov); measures to promote voluntary compliance (e.g., timely and effective risk communications); commitment of employers to support the recommendation that ill employees stay home; and support for the financial, social, physical, and mental health needs of patients and caregivers. In addition, ill individuals and their household members need clear, concise information about how to care for an ill individual in the home and when and where to seek medical care. Special consideration should be made for persons who live alone, as many of these individuals may be unable to care for themselves if ill.
Voluntary Quarantine of Household Members of Ill Persons
The goal of this intervention is to reduce community transmission from members of households in which there is a person ill with pandemic influenza. Members of households in which there is an ill person may be at increased risk of becoming infected with a pandemic influenza virus. As determined on the basis of known characteristics of influenza, a significant proportion of these persons may shed virus and present a risk of infecting others in the community despite having asymptomatic or only minimally symptomatic illness that is not recognized as pandemic influenza disease. Thus, members of households with ill individuals may be recommended to stay home for an incubation period, 7 days (voluntary quarantine) following the time of symptom onset in the household member. If other family members become ill during this period, the recommendation is to extend the time of voluntary home quarantine for another incubation period, 7 days from the time that the last family member becomes ill. In addition, consideration may be given to combining this intervention with provision of influenza antiviral medication to persons in quarantine if such medications are effective and sufficient in quantity and if a feasible means of distributing them is in place.
Requirements for success of this intervention include the prompt and accurate identification of an ill person in the household, voluntary compliance with quarantine by household members, commitment of employers to support the recommendation that employees living in a household with an ill individual stay home, the ability to provide needed support to households that are under voluntary quarantine, and guidance for infection control in the home. Additionally, adherence to ethical principals in use of quarantine during pandemics, along with proactive anti-stigma measures should be assured.83, 84
Child Social Distancing
The goal of these interventions is to protect children and to decrease transmission among children in dense classroom and non-school settings and, thus, to decrease introduction into households and the community at large. Social distancing interventions for children include dismissal of students from classrooms and closure of childcare programs, coupled with protecting children and teenagers through social distancing in the community to achieve reductions of out-of-school social contacts and community mixing. Childcare facilities and schools represent an important point of epidemic amplification, while the children themselves, for reasons cited above, are thought to be efficient transmitters of disease in any setting. The common sense desire of parents to protect their children by limiting their contacts with others during a severe pandemic is congruent with public health priorities, and parents should be advised that they could protect their children by reducing their social contacts as much as possible.
However, it is acknowledged that maintaining the strict confinement of children during a pandemic would raise significant problems for many families and may cause psychosocial stress to children and adolescents. These considerations must be weighed against the severity of a given pandemic virus to the community at large and to children in particular. Risk of introduction of an infection into a group and subsequent transmission among group members is directly related to the functional number of individuals in the group. Although the available evidence currently does not permit the specification of a “safe” group size, activities that recreate the typical density and numbers of children in school classrooms are clearly to be avoided. Gatherings of children that are comparable to family-size units may be acceptable and could be important in facilitating social interaction and play behaviors for children and promoting emotional and psychosocial stability.
A recent study of children between the ages of 25 and 36 months found that children in group care with six or more children were 2.2 times as likely to have an upper respiratory tract illness as children reared at home or in small-group care (defined as fewer than six children).85 If a recommendation for social distancing of children is advised during a pandemic and families must nevertheless group their children for pragmatic reasons, it is recommended that group sizes be held to a minimum and that mixing between such groups be minimized (e.g., children should not move from group to group or have extended social contacts outside the designated group).
Requirements for success of these interventions include consistent implementation among all schools in a region being affected by an outbreak of pandemic influenza, community and parental commitment to keeping children from congregating out of school, alternative options for the education and social interaction of the children, clear legal authorities for decisions to dismiss students from classes and identification of the decision-makers, and support for parents and adolescents who need to stay home from work. Interim recommendations for pre-pandemic planning for this intervention include a three-tiered strategy: 1) no dismissal of students from schools or closure of childcare facilities in a Category 1 pandemic, 2) short-term (up to 4 weeks) dismissal of students and closure of childcare facilities during a Category 2 or Category 3 pandemic, and 3) prolonged (up to 12 weeks) dismissal of students and closure of childcare facilities during a severe influenza pandemic (Category 4 or Category 5). The conceptual thinking behind this recommendation is developed more fully in Section VII, Duration of Implementation of Nonpharmaceutical Interventions.
Colleges and universities present unique challenges in terms of pre-pandemic planning because many aspects of student life and activity encompass factors that are common to both the child school environment (e.g., classroom/dormitory density) and the adult sphere (e.g., commuting longer distances for university attendance and participating in activities and behaviors associated with an older student population). Questions remain with regard to the optimal strategy for managing this population during the early stages of an influenza pandemic.
The number of college students in the United States is significant. There are approximately 16.6 million college students attending both 2- and 4-year universities 86, a large number of whom live away from home.87 Of the 8.3 million students attending public or private 4-year colleges and universities, less than 20 percent live at home with their parents.
At the onset of a pandemic, many parents may want their children who are attending college or university to return home from school. Immediately following the announcement of an outbreak, colleges and universities should prepare to manage or assist large numbers of students departing school and returning home within a short time span. Where possible, policies should be explored that are aligned with the travel of large numbers of students to reunite with family and the significant motivations behind this behavior. Pre-pandemic planning to identify those students likely to return home and those who may require assistance for imminent travel may allow more effective management of the situation. In addition, planning should be considered for those students who may be unable to return home during a pandemic.
Adult Social Distancing
Social distancing measures for adults include provisions for both workplaces and the community and may play an important role in slowing or limiting community transmission pressure. The goals of workplace measures are to reduce transmission within the workplace and thus into the community at large, to ensure a safe working environment and promote confidence in the workplace, and to maintain business continuity, especially for critical infrastructure. Workplace measures such as encouragement of telework and other alternatives to in-person meetings may be important in reducing social contacts and the accompanying increased risk of transmission. Similarly, modifications to work schedules, such as staggered shifts, may also reduce transmission risk.
Within the community, the goals of these interventions are to reduce community transmission pressures and thus slow or limit transmission. Cancellation or postponement of large gatherings, such as concerts or theatre showings, may reduce transmission risk. Modifications to mass transit policies/ridership to decrease passenger density may also reduce transmission risk, but such changes may require running additional trains and buses, which may be challenging due to transit employee absenteeism, equipment availability, and the transit authority’s financial ability to operate nearly empty train cars or buses.
Requirements for success of these various measures include the commitment of employers to providing options and making changes in work environments to reduce contacts while maintaining operations; whereas, within communities, the support of political and business leaders as well as public support is critical.
VI. Triggers for Initiating Use of Nonpharmaceutical Interventions
The timing of initiation of various NPIs will influence their effectiveness. Implementing these measures prior to the pandemic may result in economic and social hardship without public health benefit and may result in compliance fatigue. Conversely, implementing these interventions after extensive spread of a pandemic influenza strain may limit the public health benefits of an early, targeted, and layered mitigation strategy. Identifying the optimal time for initiation of these interventions will be challenging, as implementation likely needs to be early enough to preclude the initial steep upslope in case numbers and long enough to cover the peak of the anticipated epidemic curve while avoiding intervention fatigue. In this document, the use of these measures is aligned with declaration by WHO of having entered the Pandemic Period Phase 6 and a U.S. Government declaration of Stage 3, 4, or 5.
Case fatality ratio and excess mortality rates may be used as a measure of the potential severity of a pandemic and, thus, suggest the appropriate nonpharmaceutical tools; however, mortality estimates alone are not suitable trigger points for action. This guidance suggests the primary activation trigger for initiating interventions be the arrival and transmission of pandemic virus. This trigger is best defined by a laboratory-confirmed cluster of infection with a novel influenza virus and evidence of community transmission (i.e., epidemiologically linked cases from more than one household). Other factors that will inform decision-making by public health officials include the average number of new infections that a typical infectious person will produce during the course of his/her infection (R0) and the illness rate. For the recommendations in this interim guidance, trigger points for action assume an R0 of 1.5-2.0 and an illness rate of 20 percent for adults and 40 percent for children. In this context, in all categories of pandemic severity, it is recommended that State health authorities activate appropriate interventions (as described in Table 2) when a laboratory-confirmed human pandemic influenza case cluster is reported in their State or region (as appropriate) and there is evidence of community transmission.
Defining the proper geospatial-temporal boundary for this cluster is complex and should recognize that our connectedness as communities goes beyond spatial proximity and includes ease, speed, and volume of travel between geopolitical jurisdictions (e.g., despite the physical distance, Hong Kong, London, and New York City may be more epidemiologically linked to each other than they are to their proximate rural provinces/areas). In this document in order to balance connectedness and the optimal timing referenced above, it is proposed that the geopolitical trigger be defined as the cluster of cases occurring within a U.S. State or proximate epidemiological region (e.g., a metropolitan area that spans more than one State’s boundary). It is acknowledged this definition of region is open to interpretation; however, it offers flexibility to State and local decision-makers while underscoring the need for regional coordination in pre-pandemic planning.
From a pre-pandemic planning perspective, the steps between recognition of pandemic threat and the decision to activate a response are critical to successful implementation. Thus, a key component is the development of scenario-specific contingency plans for pandemic response that identify key personnel, critical resources, and processes. To emphasize the importance of this concept, this guidance section on triggers introduces the terminology of Alert, Standby, and Activate, which reflect key steps in escalation of response action. Alert includes notification of critical systems and personnel of their impending activation, Standby includes initiation of decision-making processes for imminent activation, including mobilization of resources and personnel, and Activate refers to implementation of the specified pandemic mitigation measures. Pre-pandemic planning for use of these interventions should be directed to lessening the transition time between Alert, Standby, and Activate. The speed of transmission may drive the amount of time decision-makers are allotted in each mode, as does the amount of time it takes to truly implement the intervention once a decision is made to activate.
These triggers for implementation of NPIs will be most useful early in a pandemic and are summarized in Table 3. This table provides recommendations arrayed by Pandemic Severity Index and U.S. Government Stage for step-wise escalation of action from Alert, to Standby, to Activate.
For the most severe pandemics (Categories 4 and 5), Alert is implemented during WHO Phase 5/U.S. Government Stage 2 (confirmed human outbreak overseas), and Standby is initiated during WHO Phase 6/U.S. Government Stage 3 (widespread human outbreaks in multiple locations overseas). Standby is maintained through Stage 4 (first human case in North America), with the exception of the State or region in which a laboratory-confirmed human pandemic influenza case cluster with evidence of community transmission is identified. The recommendation for that State or region is to Activate the appropriate NPIs as defined in Table 2 when identification of a cluster and community transmission is made. Other States or regions Activate appropriate interventions when they identify laboratory-confirmed human pandemic influenza case clusters with evidence of community transmission in their jurisdictions.
For Category 1, 2, and 3 pandemics, Alert is declared during U.S. Government Stage 3, with step-wise progression by States and regions to Standby based on U.S. Government declaration of Stage 4 and the identification of the first human pandemic influenza case(s) in the United States. Progression to Activate by a given State or region occurs when that State or region identifies a laboratory-confirmed human pandemic influenza case cluster with evidence of community transmission.
Determining the likely time frames for progression through Alert, Standby, and Activate postures is difficult. Predicting this progression would involve knowing 1) the speed at which the pandemic is progressing and 2) the segments of the population most likely to have severe illness. These two factors are dependent on a complex interaction of multiple factors, including but not limited to the novelty of the virus, efficiency of transmission, seasonal effects, and the use of countermeasures. Thus it is not possible to use these two factors to forecast progression prior to recognition and characterization of a pandemic outbreak, and predictions within the context of an initial outbreak investigation are subject to significant limitations. Therefore, from a pre-pandemic planning perspective and given the potential for exponential spread of pandemic disease, it is prudent to plan for a process of rapid implementation of the recommended measures.
Once the pandemic strain is established in the United States, it may not be necessary for States to wait for documented pandemic strain infections in their jurisdictions to guide their implementation of interventions, especially for a strain that is associated with a high case fatality ratio or excess mortality rate. When a pandemic has demonstrated spread to several regions within the United States, less direct measures of influenza circulation (e.g., increases in influenza-like illness, hospitalization rates, or other locally available data demonstrating an increase above expected rates of respiratory illness) may be used to trigger implementation; however, such indirect measures may play a more prominent role in pandemics within the lower Pandemic Severity Index categories.
Once WHO has declared that the world has entered Pandemic Phase 5 (substantial pandemic risk), CDC will frequently provide guidance on the Pandemic Severity Index. These assessments of pandemic severity will be based on the most recent data available, whether obtained from the United States or from other countries, and may use case fatality ratio data, excess mortality data, or other data, whether available from outbreak investigations or from existing surveillance.
VII. Duration of Implementation of Nonpharmaceutical Interventions
Preliminary analysis of historical data from selected U.S. cities during the 1918 pandemic suggests that duration of implementation of NPIs is significantly associated with overall mortality rates. Stopping or limiting the intensity of interventions while pandemic virus was still circulating within the community was temporally associated with recrudescent increases in mortality due to pneumonia and influenza in some communities.20, 81 Total duration of implementation for the measures specified in this guidance will depend on the severity of the pandemic and the total duration of the pandemic wave in the community, which may average about 6-8 weeks in individual communities. However, because early implementation of pandemic mitigation interventions may reduce the virus’s basic reproductive number, a mitigated pandemic wave may have lower amplitude but longer wavelength than an unmitigated pandemic wave (see Figure 2). Communities should therefore be prepared to maintain these measures for up to 12 weeks in a Category 4 or 5 pandemic.
It is important to emphasize that as long as susceptible individuals are present in large numbers, spread may continue. Immunity to infection with a pandemic strain can only occur after natural infection or immunization with an effective vaccine. The significant determinants for movement of a pandemic wave through a community are immunity and herd effect, and there is likely to be a residual pool of susceptible individuals in the community at all times. Thus, while NPIs may limit or slow community transmission, persisting pandemic virus circulating in a community with a susceptible population is a risk factor for re-emergence of the pandemic. Monitoring of excess mortality, case fatality ratios, or other surrogate markers over time will be important for determining both the optimal duration of implementation and the need for resumption of these measures.
While the decisions to stop or limit the intensity of implementation are crucial factors in pandemic response, this document is primarily oriented to providing pre-pandemic planning guidance. It is recommended for planning purposes that a total duration of 12 weeks for implementation of these measures be considered, particularly with regard to severe pandemics of Category 4 or 5 in which recrudescent disease may have significant impact. However, for less severe pandemics, a shorter period of implementation may be adequate to achieving public health benefit.
This guidance recommends a three-tiered strategy for planning with respect to the duration of dismissal of children from schools, colleges and universities, and childcare programs (Table 2):
- No dismissal of students from schools or closure of childcare facilities in a Category 1 pandemic
- Short-term (up to 4 weeks) dismissal of students and closure of childcare facilities during a Category 2 or Category 3 pandemic
- Prolonged (up to 12 weeks) dismissal of students and closure of childcare facilities during a severe influenza pandemic (Category 4 or Category 5 pandemic)
This planning recommendation acknowledges the uncertainty around the length of time a pandemic virus will circulate in a given community and around the potential for recrudescent disease when use of NPIs is limited or stopped. When cancellations and closures are indicated for the most severe pandemics, thoughtful pre-planning for their prolonged duration may allow continued use of this intervention.
VIII. Critical Issues for the Use of Nonpharmaceutical Interventions
A number of outstanding issues should be addressed to optimize the planning for use of these measures. These issues include the establishment of sensitive and timely surveillance, the planning and conducting of multi-level exercises to evaluate the feasibility of implementation, and the identification and establishment of appropriate monitoring and evaluation systems. Policy guidance in development regarding the use of antiviral medications for prophylaxis, community and workplace-specific use of personal protective equipment, and safe home management of ill persons must be fast-tracked and prioritized as part of future versions of the overall community mitigation strategy. As well, developing and delivering appropriate and effective risk communication content and a means for its effective delivery, soliciting active community support and involvement in strategic planning decisions, and assisting individuals and families in identifying their own preparedness needs are critical community factors in achieving success.
Establishing and maintaining sensitive and timely surveillance at national, State, and local levels is critical. Achieving this goal will require enhancing the capability of local physicians and public health authorities to rapidly identify suspect cases of pandemic influenza. This increased capability may be facilitated by the development of point-of-care testing and the appropriate laboratory capacity and ability to transmit specimens and data to reference laboratories.
In addition, establishing protocols for notification of Federal authorities and establishing effective reporting and feedback systems to ensure information is shared appropriately with State and local decision-makers is a key requirement. Within this framework, focused support of established systems, such as the 121 Cities Mortality Reporting System88, and the establishment of electronic mortality records may facilitate the rapid robust reporting of data elements to support the timely and appropriate implementation of NPIs. Similarly, establishing surveillance systems to monitor trends in disease in a community and to provide guidance on adjusting implementation of interventions and determining appropriate durations for intervention are critical component for implementation and will provide valuable data for decision-making around lifting interventions.
Critical issues remain with regard to ensuring both timely implementation and appropriate layering of interventions. Preliminary analysis of historical data and mathematical modeling suggest that the early, coordinated application of multiple interventions may be more effective in reducing transmission than the use of a single intervention. Multi-level exercises to evaluate the feasibility of implementation and identify critical enablers for use of these measures are required. In addition, early planning for appropriate monitoring and evaluation systems to provide assessment of the effectiveness of all proposed pandemic influenza interventions is needed. Policies and plans are required to ensure the availability of rapid diagnostic testing to distinguish influenza-like illness due to seasonal influenza strains and other respiratory pathogens from illnesses due to pandemic influenza strains. Accurate ascertainment of pandemic influenza cases is needed early during the course of a pandemic to minimize unnecessary application of mitigation interventions and in later stages of the pandemic to ascertain persisting community transmission.
Policies and planning for distribution of antiviral medications for treatment (and prophylaxis) needs to account for local capabilities, availability of the antiviral medications, and systems for distribution that could leverage the combined capabilities of public health organizations, the private sector, community organizations, and local governments. As well, guidance for community- and workplace-specific use of personal protective equipment is required, as are policies and planning to support their use.
Clear and consistent guidance is required for planning for home care of ill individuals, such as when and where to seek medical care, how to safely care for an ill individual at home, and how to minimize disease transmission in the household. In addition, guidance is required for appropriate use of community resources, such as home healthcare services, telephone care, the 9-1-1 emergency telephone system, emergency medical services, and triage services (nurse-advice lines, self-care guidance, and at-home monitoring systems) that could be deployed to provide resources for home care.
Community engagement is another critical issue for successful implementation and includes building a foundation of community preparedness to ensure compliance with pandemic mitigation measures. Community planners should use media and trusted sources in communities to 1) explain the concepts of pandemic preparedness, 2) explain what individuals and families can do to be better prepared, and 3) disseminate clear information about what the public may be asked to do in the case of a pandemic. In addition, developing and delivering effective risk communications in advance of and during a pandemic to guide the public in following official recommendations and to minimize fear and panic will be crucial to maintaining public trust
IX. Assessment of the Public on Feasibility of Implementation and Adherence
A Harvard School of Public Health public opinion poll was conducted with a nationally representative sample of adults over the age of 18 years in the United States in September-October 2006 to explore the public’s willingness to adhere to community mitigation strategies. A majority of the almost 1,700 respondents reported their willingness to follow public health recommendations for the use of NPIs, but this poll also uncovered serious financial and other concerns.89 The respondents were first read a scenario about an outbreak of pandemic influenza that spreads rapidly among humans and causes severe illness. They were then asked how they would respond to and be affected by the circumstances that would arise from such an outbreak.90
Recognizing that their lives would be disrupted, most participants expressed willingness to limit contact with others at the workplace and in public places. More than three-fourths of respondents said they would cooperate if public health officials recommended that for 1 month they curtail various activities of their daily lives, such as using public transportation, going to the mall, and going to church/religious services. However, the poll respondents were not asked if they would be willing to follow those recommendations for longer periods in the case of a severe pandemic.
More than nine in ten (94 percent) said they would stay at home away from other people for 7-10 days if they had pandemic influenza. Nearly three-fourths (73 percent) said they would have someone to take care of them at home if they became ill with pandemic influenza and had to remain at home for seven to ten days. However, about one in four (24 percent) said they would not have someone to take care of them.
In addition, 85 percent of the respondents said they and all members of their household would stay at home for seven to ten days if another member of their household was ill. However, about three-fourths (76 percent) said they would be worried that if they stayed at home with a household member who was ill from pandemic influenza, they themselves would become ill from the disease. A substantial proportion of the public believed that they or a household member would be likely to experience various problems, such as losing pay, being unable to get the healthcare or prescription drugs they need, or being unable to get care for an older person or a person with a disability, if they stayed at home for 7-10 days and avoided contact with anyone outside their household.
If schools and daycare were closed for 1 month, 93 percent of adults who have major responsibility for children under age 5 who are normally in daycare or for children 5 to 17 years of age and who have at least one employed adult in the household think they would be able to arrange care so that at least one employed adult in the household could go to work. Almost as many (86 percent) believe they would be able to do so if schools were closed for 3 months.
When asked about possible financial difficulties due to missed work, a greater number of respondents reported they would face financial problems. While most employed people (74 percent) believed they could miss 7-10 days of work without having serious financial problems, one in four (25 percent) said they would face such problems. A majority (57 percent) think they would have serious financial problems if they had to miss work for 1 month, and three-fourths of respondents (76 percent) thought they would have such problems if they were away from work for 3 months.
The Public Engagement Project on Community Control Measures Against a Severe Pandemic of Influenza was carried out in October and November 2006.91 Two to three representatives from the organized stakeholder public were chosen from approximately ten major sectors likely to be affected by the measures (e.g., public health, education, private sector) to form a 50-member national level panel. In addition, a representative sample of approximately 260 citizens from the general public was recruited from Seattle, Washington; Syracuse, New York; Lincoln, Nebraska; and Atlanta, Georgia. Participants were presented with a scenario describing a severe pandemic and asked to consider their support for the use of the NPIs outlined above.
Approximately 95 percent or more of the citizens and stakeholders supported encouraging ill persons to stay at home, and the same high percentage supported canceling large public gatherings and altering work patterns for the purpose of social distancing. A lower percentage (83-84 percent) supported encouraging the members of households with ill persons to stay at home, and a similar percentage favored closing schools and large day care facilities for an extended period. Overall, approximately two-thirds of both citizens and stakeholders (64-70 percent) supported all of the interventions. Based on the scenario of a severe pandemic, nearly half (44-48 percent) of the citizens and stakeholders supported implementation of the interventions when pandemic influenza first strikes the United States, and approximately one-third of the public supported implementation when influenza first strikes in their State.
Although the findings from this poll and public engagement activity reported high levels of willingness to follow pandemic mitigation recommendations, it is uncertain how the public might react when a pandemic occurs. These results need to be interpreted with caution in advance of a severe pandemic that could cause prolonged disruption of daily life and widespread illness in a community. Adherence rates may be higher during the early stages of a pandemic and adherence fatigue may increase in the later stages. These results may not be able to predict how the public would respond to a severe pandemic in their community nor predict how the public will tolerate measures that must be sustained for several months. Changes in perceived risk from observed mortality and morbidity during a pandemic relative to the need for income and the level of community and individual/family disruption caused by the mitigation interventions may be major determinants of changes in public adherence.
X. Planning to Minimize Consequences of Community Mitigation Strategy
Pandemic mitigation interventions will pose challenges for individuals and families, employers (both public and private), and local communities. Some cascading second- and third-order effects will arise as a consequence of the use of NPIs. However, until a pandemic-strain vaccine is widely available during a pandemic, these interventions are key measures to reduce disease transmission and protect the health of Americans. The community mitigation strategy emphasizes care in the home and underscores the need for individual, family, and employer preparedness. Adherence to these interventions will test the resiliency of individuals, families, and employers.
The major areas of concern derive from the recommendation to dismiss children from school and closure of childcare programs. The concerns include 1) the economic impact to families; 2) the potential disruption to all employers, including businesses and governmental agencies; 3) access to essential goods and services; and 4) the disruption of school-related services (e.g., school meal programs). Other interventions, such as home isolation and voluntary home quarantine of members of households with ill persons, would also contribute to increased absenteeism from work and affect both business operations and employees. These issues are of particular concern for vulnerable populations who may be disproportionately impacted.
However, these and other consequences may occur in the absence of community-wide interventions because of spontaneous action by the public or as a result of closures of schools and workplaces related to absenteeism of students and employees. These consequences associated with the pandemic mitigation interventions must be weighed against the economic and social costs of an unmitigated pandemic.
Many families already employ a number of strategies to balance childcare and work responsibilities. Pandemic mitigation interventions, especially dismissal of students from school classes and childcare programs, will be even more challenging. These efforts will require the active planning and engagement of all sectors of society.
Impact of School Closure on the Workforce
Workplace absenteeism is the primary issue underlying many of the concerns related to the pandemic mitigation strategies. Absenteeism for child minding could last as long as 12 weeks for a severe pandemic. The potential loss of personal income or employment due to absenteeism related to prolonged cancellation of school classes and the need for child minding can lead to financial insecurity, fear, and worry. Workplace absenteeism, if severe enough, could also affect employers and contribute to some workplaces reducing or closing operations (either temporarily or permanently). Depending on the employers affected, this could limit the availability of essential goods and services provided by the private sector and the government, interrupting critical business supply chains, and potentially threatening the ability to sustain critical infrastructure. Workplace absenteeism and the resulting interruption of household income would test the resiliency of all families and individuals but would be particularly challenging for vulnerable populations. The potential impact on society underscores the need for preparedness of individuals, families, businesses, organizations, government agencies, and communities.
There are 300 million Americans living in 116 million households in the United States.92 Approximately one-third of U.S. households (40 million) include children less than 18 years of age. In slightly more than half of these households (22 million), all adults present are working. Five million of these households have only a single working adult present. These households with children and only one working adult would be impacted disproportionately—potentially requiring the single working adult in the household to remain home to mind the children if students were dismissed from classes or childcare facilities were closed.
Depending upon the age threshold assumed for children requiring adult supervision, the impact of dismissing students from school and closure of childcare programs on working families would vary. The number of households impacted could range from 12.4 million (assuming children <13 years of age would require adult supervision) to 15.4 million (assuming children <15 years of age would require full-time adult supervision).
The projected impact of these estimates, however, does not fully account for the strategies families already employ to care for their children and remain in the workforce. Families with all adults in the household working currently utilize a number of strategies for child minding, including the assistance of other family members, such as grandparents and siblings, assistance from separated/divorced spouses, children minding themselves, staggered work/child-minding shifts for parents, and parents working from home. There are 60 million children under the age of 15. Over half these children (32 million or 56 percent) have a working mother. Nearly one-third (29 percent) of these children have a mother who works a non-day shift. Nearly one-third (29 percent) have a mother working part time. Nearly one-third (30 percent) of children under age 5 living with only their father in the household were regularly cared for by their mother while their father was working or in school. One of seven (14 percent) school age children, 5-14 years of age, living with only one parent in the household were regularly cared for by the other parent while their father or mother was working or attending school.93
The Harvard School of Public Health public opinion poll reported that 86 percent of families with children under age 5 in childcare or children 5-17 years of age would be able to arrange for childcare to allow at least one adult in the household to continue to work if classes and childcare were cancelled for 3 months.89 These findings, when applied to the overall population, suggest that approximately one in seven households with children attending school or childcare would be unable to have at least one adult continue to work during a prolonged period of school and childcare cancellation.
Impact of Voluntary Home Isolation and Voluntary Home Quarantine
The impacts of pandemic mitigation interventions on workplace absenteeism are overlapping. In contrast to possible prolonged absenteeism for child minding, voluntary home quarantine would require all household members of an ill individual to remain home for approximately 1 week (single-person households, representing 27 percent of all U.S. households, would not be impacted by this intervention). In addition, ill individuals would stay home from work for a period of 7-10 days. When estimating overall absenteeism, this hierarchy suggests first considering the impact of child minding, then illness, then quarantine. For example, if a working single parent remains home from work for 12 weeks to mind her children, workplace absenteeism is unaffected if one of her children becomes ill and the home voluntarily quarantines itself (the adult will remain absent from the workplace for 12 weeks due to child minding). If a working adult living in a household of two or more people becomes ill and is absent due to illness, the additional impact of absenteeism related to voluntary home quarantine would only apply if there are other non-ill working adults present in the household.
Absenteeism due to illness is directly related to the rate of clinical illness in the population. The proposed community interventions attempt to reduce disease transmission and illness rates. As illness rates are reduced, absenteeism related to illness and quarantine would be expected to decline, whereas absenteeism related to child minding would remain constant.
The feasibility of following pandemic mitigation interventions is of particular concern for vulnerable populations (e.g., people who are living alone, the poor or working poor, and the elderly [particularly those who are homebound], homeless, recent immigrants, disabled, institutionalized, or incarcerated). More than 31 million individuals in the United States live alone (27 percent of all households) and one-third of these individuals are aged 65 years or older. According to the Harvard School of Public Health public opinion poll, 45 percent of respondents living in one-adult households report they would not have anyone to take care of them in the event of a pandemic.90 More than four in ten respondents living in one-adult households (45 percent) and about one-third of low-income (36 percent), African-American (34 percent), disabled (33 percent), or chronically ill (32 percent) adults said they would not have anyone to take care of them if they were ill and had to remain at home. Similarly among people age 65 or over, those who live in one-adult households were far more likely (41 percent vs 15 percent) than those who lived in two-adult households with another person age 65 or over to say they would have no one to take care of them.
Additionally, the millions of frail elderly individuals who require life-sustaining supports to remain in the community would need additional consideration. Planning should begin now to include solutions to address the needs of the frail elderly. Of the approximately 45 million seniors (over age 65) currently in the U.S., 5 percent, or 2.25 million are considered frail. Currently the Elderly Nutrition Program provides meals for approximately 3 million elderly participants, including the frail elderly, in congregate settings, or through volunteers who provide homebound seniors with home-delivered meals. Participants receive approximately half of their daily nutritional needs from those meals. In addition, other related community-based services, such as transportation and healthcare, are critical for seniors, particularly the frail elderly, who receive this assistance in order to maintain their independence.94, 95 Communities will need to plan for how these vital supports can continue for this population as well as for other groups with unique physical and mental challenges in light of efforts to protect lives and limit the spread of disease.
Strategies to Minimize Impact of Workplace Absenteeism
Solutions or strategies for minimizing the impact of dismissal of students from school and closure of childcare programs and workplace absenteeism may include the following: 1) employing child-minding strategies to permit continued employment; 2) employing flexible work arrangements to allow persons who are minding children or in quarantine to continue to work; 3) minimizing the impact on household income through income replacement; and 4) ensuring job security.
In contrast to the unpredictable nature of workplace absenteeism related to illness (unpredictability of who will be affected and who will be absent from work), it may be easier to forecast who is likely to be impacted by the dismissal of students from school and/or the closure of childcare. Impacted families and individuals can be identified well in advance of an event. Accordingly, early planning and preparedness by employers, communities, individuals, and families is critical to minimizing the impact of this intervention on families and businesses.
In a severe pandemic, parents would be advised to protect their children by reducing out-of-school social contacts and mixing with other children.96 The safest arrangement would be to limit contact to immediate family members and for those family members to care for children in the home. However, if this is not feasible, families may be able to develop support systems with co-workers, friends, families, or neighbors, to meet ongoing childcare needs. For example, they could prepare a plan in which two to three families work together to supervise and provide care for a small group of infants and young children.
As was noted in the Harvard School of Public Health public opinion poll, parents reported that they would primarily depend upon family members to assist with child minding (self/family member in the home, 82 percent; children caring for themselves, 6 percent; family member outside the home, 5 percent; and combination, 5 percent). One of four households with children under age 5 in childcare or children 5-17 years of age estimated that they would be able to work from home and care for their children. Students returning home from colleges and universities may also be available to assist with child minding.90
More than half (57 percent) of private-sector employees have access to paid sick leave.97 More than three-fourths (77 percent) have paid vacation leave, and 37 percent have paid personal leave. Currently, leave policies would likely not cover the extended time associated with child minding. Expanded leave policies and use of workplace flexibilities, including staggered shifts and telework, would help employees balance their work and family responsibilities during a severe pandemic. Additional options to offset the income loss for some employees meeting specific requirements include provisions for Unemployment Insurance. In addition, following a “major disaster” declaration under the Stafford Act, additional individual assistance, including Disaster Unemployment Assistance, may become available to eligible persons. The Family and Medical Leave Act may also offer protections in terms of job security for up to 12 weeks for covered and eligible employees who have a serious health condition or who are caring for a family member with a serious health condition.
In addition to employers expanding leave policies and adopting workplace flexibilities, Federal, State, local, tribal, and territorial officials should review laws, regulations, and policies to identify ways to help mitigate the economic impact of a severe pandemic and implementation of the pandemic mitigation measures on employers, individuals, and families, especially vulnerable populations. Clarity on such policies from employers and the government will help workers plan and prepare for the potential threat of a severe pandemic and to plan and comply with the pandemic mitigation strategies. Many of these programs and policies would also be applicable if no pandemic mitigation strategies were in place and absences were due to personal illness or the need to care for an ill family member.
Interruption of School Meal Programs
An additional concern related to dismissal of students is the interruption of services provided by schools, including nutritional assistance through the school meal programs. This would alter the nature of services schools provide and require that essential support services, including nutritional assistance to vulnerable children, be sustained though alternative arrangements.
The National School Lunch Program operates in more than 100,000 public and non-profit private schools and residential childcare institutions 98, and the School Breakfast Program operates in approximately 80,000 schools 99. School lunch and breakfast are free for students at or below 130 percent of the poverty level and are available at reduced price for students between 130 percent and 185 percent poverty level. Half of the thirty million students that participate in the School Lunch Program received free meals in 2006. During the summer, a Summer Food Service Program operates at more than 30,000 sites, providing breakfast, lunch and snacks to children living in low-income areas; the program served approximately 1.9 million total students in 2005.100
According to the Harvard School of Public Health public opinion poll, 13 percent of households with children receiving free school meals reported that they would have a major problem if schools were closed and meals discontinued.90 Approximately 15 million children currently receive free school meals; thus, it is anticipated that about 2 million would have a major problem associated with the interruption of school meals.
Many of these households also depend upon other Federal nutrition programs, including the Food Stamp Program, the Special Supplemental Nutrition Program for Women, Infants, and Children, and the Child and Adult Care Food Program, and community food pantries.
Strategies to Minimize the Impact of Interrupting School Meals
During a severe pandemic, it will be important for individuals and families to plan to have extra supplies on hand, as people may not be able to get to a store, stores may be out of supplies, and other services (e.g., community soup kitchens and food pantries) may be disrupted. Communities and families with school-age children who rely on school meal programs should anticipate and plan as best they can for a disruption of these services and school meal programs for up to 12 weeks.
This may be particularly challenging for families with children who already depend on a number of these programs. The Federal Government is working together with State and local emergency response planners to find creative solutions to meet nutrition assistance needs for vulnerable populations. Local government and faith-based and community leaders are being encouraged to work closely with nutrition program administrators at the local, State, and Federal level to:
- Develop plans to address community nutrition assistance needs during a pandemic
- Identify nutrition program adaptations needed to respond to social distancing, voluntary quarantines, and possible disruption of the normal food supply
- Address challenges related to the supply and delivery of food through commercial markets
- Identify current program flexibilities/authorities and determine if others are needed
School Resources Available for Community Service
If students are dismissed from school but schools remain open, school- and education-related assets, including school buildings, school kitchens, school buses, and staff, may continue to remain operational and potentially be of value to the community in many other ways. In addition, faculty and staff may be able to continue to provide lessons and other services to students by television, radio, mail, Internet, telephone, or other media. Continued instruction is not only important for maintaining learning but also serves as a strategy to engage students in a constructive activity during the time that they are being asked to remain at home.
Impact on Americans Living Abroad
Although this document primarily considers a domestic influenza pandemic, it provides guidance that is relevant to American organizations and individuals based abroad. There are approximately 7 million American citizens living overseas. About 3 million of these are working abroad on behalf of more than 50 Federal agencies, although the vast majority are employees of the U.S. Department of Defense and their dependents.101, 102 In addition, there are 194 American Overseas Schools that have students in all grades, the vast majority of whom are children of U.S. citizens working in government or for private companies and contractors. Excluding the military, approximately one-third of American households overseas have children under 18 years of age, and approximately half are households in which both parents work.103 (“American households” in this context is defined as households in which the head of household is a U.S. citizen without dual citizenship.) The impact of pandemic mitigation measures on Americans overseas would be similar to that in the United States, except that there are very few extended family members overseas to assist in childcare should schools be closed. As a result, a decision to dismiss students from school and close childcare could result in increased workplace absenteeism. This might be partially offset by the fact that single-parent households with children are less common among Americans abroad than in the United States.
During a pandemic, security for Americans abroad could become an increased concern, particularly in those countries that are unstable or lack the capability to prevent lawlessness. In such instances, the desire to close institutions, such as schools or embassies, must be balanced against the greater protection that can be provided to American citizens who are gathered in one place, rather than distributed in their homes. Additionally, an estimated one-third (80 of 250) of U.S. diplomatic posts abroad have undependable infrastructure for water, electricity, and food availability, which may impair the ability of people to adhere to NPIs.103
In consideration of these factors, many Americans may wish to repatriate to the United States at the outset of a pandemic, and this should be considered in decisions to implement closure of institutions and other NPIs in the international setting.
Strategy to Reduce Impact on Americans Living Abroad
Americans abroad should review pandemic preparedness recommendations issued by the U.S. Department of State and the U.S. Department of Health and Human Services. Updated regional and country-specific information is provided on www.pandemicflu.gov, the CDC travel website (www.cdc.gov/travel/), and the U.S. Department of State’s travel site (www.travel.State.gov). In addition, two million of the estimated 4.5 million non-military affiliated Americans abroad are registered with U.S. Embassies and Consulates, and are thus able to receive warnings and announcements from these diplomatic posts. Those preparing to travel overseas can register for country-specific announcements online at https://travelregistration.State.gov/ibrs/.
Americans should not assume that international transportation would be available during a pandemic. As a result, Americans abroad should identify local sources of healthcare and prepare to “shelter-in-place” if necessary. In those areas with potentially limited water and food availability, Americans living abroad are encouraged to maintain supplies of food and water to last at least two and as long as 12 weeks. Additional recommendations for preparing for a pandemic while abroad are available in the State Department fact sheet How to Prepare for “Sheltering-In-Place,” which is available at travel.state.gov/travel/tips/health/health_3096.html.
XI. Testing and Exercising Community Mitigation Interventions
Because pandemics occur rarely, drills and exercises are required to test plans and to maintain response proficiency. Such real-world operational experience could yield invaluable empirical evidence regarding how readily particular pandemic mitigation measures might be implemented and how well they might work if applied on a larger scale and/or for longer duration. Drills and exercises permit individuals and organizations to carry out their normal duties and relate to each other under unusual circumstances in simulated environments that are far less costly and threatening than real events.
Discussion-based exercises (e.g., tabletop exercises) are a first step to help identify “gaps” in the plan, policies, protocols, processes, and procedures, included in planning for pandemic mitigation interventions. Such gaps should be filled before expensive, resource-intense, operations-based drills and exercises are conducted. For example, developing community communications plans to notify the public about the status of a pandemic, what protective actions should be taken, and where to seek medical advice during a pandemic, as well as planning for distribution of antiviral medications, determining the process for dismissal of students from schools and closure of childcare facilities, and planning for possible closure of mass gatherings should be decided before conducting a full-scale exercise.
As responders practice the plan through exercising, they learn which aspects of response do not go “as planned.” After the exercise, responders debrief (“hot wash”) and create an after-action-report to describe corrective actions to fix response problems, including who is responsible for fixing what by when (a “corrective action plan”). Proposed solutions should be re-tested to ensure that they adequately correct the response problem.
In July 2006, CDC’s Coordinating Office of Terrorism Preparedness and Emergency Response provided supplemental guidance for recipients of Federal funding through the Public Health Preparedness and Response Cooperative Agreement (Cooperative Agreement AA154) for the purpose of pandemic influenza preparedness activities specifically intended to foster developing and exercising pandemic influenza plans. Specific performance measures for testing and exercising plans are listed in that guidance, which can be accessed at www.bt.cdc.gov/planning/coopagreement/pdf/phase2-panflu-guidance.pdf.
XII. Research Needs
A comprehensive research agenda for pandemic influenza is needed to improve the evidence base of the proposed NPIs described in this interim guidance. This agenda should include conducting studies to gain more knowledge of the epidemiology of influenza, the effectiveness of community-based interventions, the use of medical countermeasures that complement community strategies, the modification of existing mathematical modeling to include adverse societal consequences, and the development of new modeling frameworks to assess the effectiveness of interventions.6, 13, 14, 19, 20, 104-108 Research to clarify or expand upon these issues may be necessary during a pandemic outbreak. Thus, planning for accelerated Institutional Review Board approval in the setting of a pandemic may facilitate important research conducted in hospitals, public health departments, and universities.
Key areas for further research include the following:
- Enhancing epidemiologic and laboratory surveillance systems for influenza: Existing influenza surveillance systems have gaps in timeliness and completeness that will hamper adequate functioning during a pandemic. A high priority must be given to the development of more timely surveillance for laboratory-confirmed cases of human infections with novel influenza A viruses, methods to rapidly estimate the excess mortality rate during a pandemic, better use of existing electronic data sources, and the development of platforms that can be used to assess the effectiveness of pandemic interventions, including vaccines, antiviral medications, and NPIs.
- Development of rapid diagnostics: The development of sensitive and specific point-of-care rapid tests for influenza A subtypes with pandemic potential may play an important role in pandemic preparedness. Laboratory diagnosis of influenza is critical for treatment, prophylaxis, surveillance, vaccine development and efficacy, and the timing of the initiation of pandemic mitigation strategies. The development of sensitive and specific point-of-care rapid tests for influenza A subtypes with pandemic potential may play an important role in pandemic preparedness
- Measurement of effectiveness of personal protective equipment (PPE; e.g., surgical masks and respirators) in community settings: Quantification of the effectiveness of PPE for infection prevention, the ability of community members to correctly use PPE, the relative benefit of fit-testing for respirator-use in community settings, the utility of PPE for children and the elderly for whom PPE is not currently designed, and the relative contribution of PPE to safety in the context of other NPIs should be undertaken
- Determination of the trigger points for implementation of NPIs: Infection with influenza results in annual community-based epidemics. While the historic data from 1918 on use of NPIs indicate an ecological relationship between timing and effectiveness, additional prospective data on timing of each of these measures will usefully complement the value of historic evidence. Studies of some of the NPIs can be conducted during sporadic outbreaks of seasonal influenza.
- Determination of markers to signal that it might be appropriate to end or lift pandemic mitigation interventions: Pandemic mitigation measures may be employed in communities until sufficient vaccine is available to that population or until other parameters are reached. Retrospective and other studies could provide detailed information regarding these predictive factors
- Advancing the knowledge base on pharmaceutical interventions: Antiviral medications and vaccines are integral components of pandemic mitigation strategies. Availability and use of medications can complement the effectiveness of voluntary isolation and quarantine and enhance compliance within communities. Therefore, the capacity to rapidly obtain data on antiviral and vaccine effectiveness, the development of resistance, and the assessment of distribution dynamics is important to successful implementation of pandemic mitigation strategies.
- Determination, through prospective field studies, of the effectiveness of interventions required to achieve reduced transmission: The evidence base for most of the interventions currently suggested for use is based on historic reviews, common sense, and biological plausibility. Evidence should be obtained through prospective trials or observational studies conducted during seasonal influenza outbreaks. Given the socioeconomic ramifications of pandemic mitigation interventions, such as social distancing measures for children and adults, adherence with prolonged use of interventions is likely to be limited. Therefore, in addition to the assessment of effectiveness, studies should also be done to assess factors that promote compliance and the optimal duration of interventions.
- Improved understanding of fundamental questions of influenza transmission and epidemiology: Prospective epidemiological studies to address gaps in understanding of influenza epidemiology and transmission and the natural history of disease may guide the application of NPIs in the community.
- Improved understanding of environmental factors that may influence influenza survival and transmissibility: Studies to elucidate the impact of temperature, humidity, radiation, seasonality, and other factors and their relation to influenza transmission in communities are needed to identify complementary mitigation interventions.
- Improved measures of uncertainty with regard to parameter and model estimates for mathematical modeling of NPIs: Development of improved metrics of uncertainty around interpretation of modeling outputs may more appropriately guide the incorporation of modeling results into development of policy for community use of these measures.
- Characterize and determine the potential psychosocial sequelae of voluntary home quarantine and social distancing strategies: Investigation of the use of home quarantine and social distancing strategies in simulations and in severe seasonal influenza outbreaks could determine key issues that might arise during a severe pandemic requiring long-term social distancing strategies and might suggest possible strategies to reduce untoward effects. Studies that focus on incidences of school closure that might be used for other disease outbreaks might help to better understand facilitators and barriers to adherence with public health recommendations.
- Expanded parameter inputs for modeling the potential effectiveness of school and workplace interventions in mitigating an influenza pandemic: The current mathematical models have been prepared with a single option for each of the interventions. For example, the recommendation for dismissing students from schools is absolute and does not include options to partially implement this intervention. Given the societal consequences of this protective intervention, as well as other measures, it is recommended that models be further developed to study a broader range of options for each intervention.
- Appropriate modeling of effect of interventions to limit the impact of cascading second- and third-order consequences of the use of NPIs: The implementation challenges and cascading consequences of both the pandemic and of the interventions should be considered in the mathematical models. For example, broader outcome measures beyond influenza-related public health outcomes might include costs and benefits of intervention strategies.
- Development of process indicators: Given the need to assess community-level response capacity in any Incident of National Significance, a research agenda related to pandemic mitigation of pandemic influenza should include development of tools to assess ongoing response capacity. These tools may include ways to assess compliance with interventions and to determine factors that influence compliance fatigue. Such tools would be most useful for the implementing jurisdictions in development of preparedness plan and for evaluating the implementation dynamics during a pandemic.
XIII. Conclusions
The goals of planning for an influenza pandemic are to save lives and to reduce adverse personal, social, and economic consequences of a pandemic; however, it is recognized that even the best plans may not completely protect everyone. Such planning must be done at the individual, local, tribal, State, Federal, and international levels, as well as by businesses and employers and other organizations, in a coordinated manner. Interventions intended for mitigating a pandemic pose challenges for individuals and families, employers (both public and private), schools, childcare programs, colleges and universities, and local communities. Pre-pandemic, scenario-based planning offers an opportunity to better understand and weigh the benefits of possible interventions as well as identify strategies to maximize the number of people protected while reducing, to the greatest extent possible, the adverse social, logistical, and economic effects of proposed interventions.
The early use of combinations of NPIs that are strategically targeted, layered, and implemented in a coordinated manner across neighboring jurisdictions and tailored to the severity of the pandemic is a critical component of a comprehensive strategy to reduce community disease transmission and mitigate illness and death. This guidance introduces, for the first time, a Pandemic Severity Index in which case fatality ratio serves as the critical driver for categorizing the severity of a pandemic. The severity index is designed to enable better forecasting of the impact of a pandemic and allows for fine-tuning the selection of the most appropriate tools and interventions, balancing the potential benefits against the expected costs and risks. Decision-makers may find the Pandemic Severity Index useful in a wide range of pandemic planning scenarios beyond pandemic mitigation, including, for example, in plans for assessing the role for pre-pandemic vaccine or estimating medical ventilator supply and other healthcare surge requirements.
This planning guidance should be viewed as the first iteration of a dynamic process that will be revisited and refined on a regular basis and informed by new knowledge gained from research, exercises, and practical experience. The array of public health measures available for pandemic mitigation is also evolving, and future versions of this document will need to incorporate the changing landscape. Some critical priority issues for inclusion in subsequent drafts are highlighted in actions being pursued under the National Implementation Plan Action Items. These include the role and further development of point-of-care rapid influenza diagnostics, antiviral medications, pre-pandemic vaccines, face mask and respirator use in community settings, and home-care infection control management strategies. The development of sensitive and specific diagnostic tests for pandemic strains not only enables a more efficient use of antiviral medication for treatment and prophylaxis but also helps minimize the need for isolation and quarantine for persons with nonspecific respiratory infections. The increasing availability of antiviral medications will prompt new discussions about the role of antiviral prophylaxis for households and workers in critical infrastructure to further reduce transmission potential and to provide incentives to comply with voluntary home quarantine recommendations and for healthcare and other workers to report to work. Changes in the technology and availability of personal protective equipment will influence guidance on community use of face masks and respirators. Guidance for safe management of ill family members in the household should serve to decrease the risk of household transmission of influenza, once again aligning incentives for compliance and increasing the effectiveness of pandemic mitigation interventions.
Planning and preparedness for implementing pandemic mitigation strategies is complex and requires participation by all levels of government and all segments of society. Pandemic mitigation strategies call for specific actions by individuals, families, businesses and employers, and organizations. Building a foundation of community and individual and family preparedness and developing and delivering effective risk communication for the public in advance of a pandemic is critical. If embraced earnestly, these efforts will result in enhanced ability to respond not only to pandemic influenza but also to multiple hazards and threats. While the challenge is formidable, the consequences of facing a severe pandemic unprepared will be intolerable. This interim pre-pandemic planning guidance is put forth as a step in our commitment to address the challenge of mitigating a pandemic by building and enhancing community resiliency.
XIV. References
1. Institute of Medicine; Committee on Modeling Community Containment for Pandemic Influenza. Modeling Community Containment for Pandemic Influenza. A Letter Report. Washington D.C.: The NationalAcademies Press; 2006. p.1.
2. U.S. Homeland Security Council. National Strategy for Pandemic Influenza Implementation Plan. 2006 [cited 2007 January 23]; Available from: www.whitehouse.gov/homeland/nspi_implementation.pdf
3. Gostin L. Public health strategies for pandemic influenza: ethics and the law. JAMA. 2006 Apr 12;295(14):1700-4.
4. Institute of Medicine. The Threat of Pandemic Influenza: Are We Ready? Washington, D.C.: The National Academies Press; 2004.
5. Gerberding JL. Pandemic Preparedness: Pigs, Poultry, and People versus Plans, Products, and Practice. J Infect Dis. 2006 Nov 1;194 Suppl 2:S77-81.
6. Fauci AS. Seasonal and pandemic influenza preparedness: science and countermeasures. J Infect Dis. 2006 Nov 1;194 Suppl 2:S73-6.
7. Monto AS. The threat of an avian influenza pandemic. N Engl J Med. 2005 Jan 27;352(4):323-5.
8. Monto AS. The threat of an avian influenza pandemic. N Engl J Med. 2005 Mar 10;352(10):1056.
9. U.S. Department of Health and Human Services. HHS Pandemic Influenza Plan. 2005 [cited 2007 January 23]; Available from: www.hhs.gov/pandemicflu/plan/
10. Meltzer MI, Cox NJ, Fukuda K. The economic impact of pandemic influenza in the United States: priorities for intervention. Emerg Infect Dis. 1999 Sep-Oct;5(5):659-71.
11. U.S. Congress. Congressional Budget Office. A potential influenza pandemic: possible macroeconomic effects and policy issues. 2005. p.10 [cited 2007 January 23]; Available from: www.cbo.gov/ftpdocs/69xx/doc6946/12-08-BirdFlu.pdf
12. Toner E, Waldhorn R, Maldin B, Borio L, Nuzzo JB, Lam C, et al. Hospital preparedness for pandemic influenza. Biosecur Bioterror. 2006;4(2):207-17.
13. Inglesby TV, Nuzzo JB, O'Toole T, et al. Disease mitigation measures in the control of pandemic influenza. Biosecur Bioterror. 2006;4:1-10.
14. Fauci AS. Pandemic influenza threat and preparedness. Emerg Infect Dis. 2006 Jan;12(1):73-7.
15. Enserink M. Avian influenza. 'Pandemic vaccine' appears to protect only at high doses. Science. 2005 Aug 12;309(5737):996.
16. Fedson DS. Preparing for pandemic vaccination: an international policy agenda for vaccine development. J Public Health Policy. 2005 Apr;26(1):4-29.
17. Fauci AS. Race against time. Nature. 2005 May 26;435(7041):423-4.
18. Kilbourne ED, Smith C, Brett I, Pokorny BA, Johansson B, Cox N. The total influenza vaccine failure of 1947 revisited: major intrasubtypic antigenic change can explain failure of vaccine in a post-World War II epidemic. Proc Natl Acad Sci U S A. 2002 Aug 6;99(16):10748-52.
19. Osterholm MT. Preparing for the next pandemic. N Engl J Med. 2005 May 5;352(18):1839-42.
20. Institute of Medicine; Committee on Modeling Community Containment for Pandemic Influenza. Modeling Community Containment for Pandemic Influenza. A Letter Report. Washington D.C.: The NationalAcademies Press; 2006.
21. Crosby AW. America's Forgotten Pandemic: The Influenza of 1918. Second ed. Cambridge: Cambridge University Press; 2003.
22. Kilbourne ED. Influenza pandemics of the 20th century. Emerg Infect Dis. 2006 Jan;12(1):9-14.
23. Barry JM. The Great Influenza: The Epic Story of the Deadliest Plague in History. New York: Viking; 2004.
24. Taubenberger JK, Morens DM. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. 2006 Jan;12(1):15-22.
25. Cox NJ, Subbarao K. Global epidemiology of influenza: past and present. Annu Rev Med. 2000;51:407-21.
26. Frost WH. The epidemiology of influenza. 1919. Public Health Rep. 2006;121 Suppl 1:149-59; discussion 8.
27. Chin TD, Foley JF, Doto IL, Gravelle CR, Weston J. Morbidity and mortality characteristics of Asian strain influenza. Public Health Rep. 1960 Feb;75:148-58.
28. Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature. 2006 Jul 27;442(7101):448-52.
29. Germann TC, Kadau K, Longini IM, Jr., Macken CA. Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci U S A. 2006 Apr 11;103(15):5935-40.
30. Glass RJ. Targeted social distancing design for pandemic influenza. Emerg Infect Dis. 2006;12:1671-81.
31. Longini IM, Jr., Nizam A, Xu S, Ungchusak K, Hanshaoworakul W, Cummings DA, et al. Containing pandemic influenza at the source. Science. 2005 Aug 12;309(5737):1083-7.
32. Longini IM, Jr., Halloran ME, Nizam A, Yang Y. Containing pandemic influenza with antiviral agents. Am J Epidemiol. 2004 Apr 1;159(7):623-33.
33. Bell DM. Non-pharmaceutical interventions for pandemic influenza, national and community measures. Emerg Infect Dis. 2006 Jan;12(1):88-94.
34. U.S. Congress. Congressional Budget Office. A potential influenza pandemic: possible macroeconomic effects and policy issues. 2005 [cited 2007 January 23]; Available from: www.cbo.gov/ftpdocs/69xx/doc6946/12-08-BirdFlu.pdf
35. World Health Organization. WHO global influenza preparedness plan. The role of WHO and recommendations for national measures before and during pandemics. 2005 [cited 2007 January 23]; Available from: www.who.int/csr/resources/publications/influenza/WHO_CDS_CSR_GIP_2005_5.pdf
36. Ball F, Britton T, Lyne O. Stochastic multitype epidemics in a community of households: estimation of threshold parameter R-* and secure vaccination coverage. Biometrika. 2004;91:345-62.
37. Heesterbeek JA. A brief history of R0 and a recipe for its calculation. Acta Biotheor. 2002;50(3):189-204.
38. Sanchez MA, Blower SM. Uncertainty and sensitivity analysis of the basic reproductive rate. Tuberculosis as an example. Am J Epidemiol. 1997 Jun 15;145(12):1127-37.
39. Lewis B. Simulated Pandemic Influenza Outbreaks in Chicago. Technical Report: Virginia Bioinformatics Institute at Virginia Tech; 2006. Report No.: NDSSL-TR-06-023.
40. Eubank S. Network based models of infectious disease spread. Jpn J Infect Dis. 2005 Dec;58(6):S9-13.
41. Cox NJ, Subbarao K. Influenza. Lancet. 1999 Oct 9;354(9186):1277-82.
42. Yuen KY, Chan PK, Peiris M, Tsang DN, Que TL, Shortridge KF, et al. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet. 1998 Feb 14;351(9101):467-71.
43. Welliver R, Monto AS, Carewicz O, Schatteman E, Hassman M, Hedrick J, et al. Effectiveness of oseltamivir in preventing influenza in household contacts: a randomized controlled trial. JAMA. 2001 Feb 14;285(6):748-54.
44. Halloran ME, Hayden FG, Yang Y, Longini IM, Jr., Monto AS. Antiviral Effects on Influenza Viral Transmission and Pathogenicity: Observations from Household-based Trials. Am J Epidemiol. 2007 Jan 15;165(2):212-21.
45. Hayden FG, Belshe R, Villanueva C, Lanno R, Hughes C, Small I, et al. Management of influenza in households: a prospective, randomized comparison of oseltamivir treatment with or without postexposure prophylaxis. J Infect Dis. 2004 Feb 1;189(3):440-9.
46. Hayden FG, Gubareva LV, Monto AS, Klein TC, Elliot MJ, Hammond JM, et al. Inhaled zanamivir for the prevention of influenza in families. Zanamivir Family Study Group. N Engl J Med. 2000 Nov 2;343(18):1282-9.
47. Monto AS, Pichichero ME, Blanckenberg SJ, Ruuskanen O, Cooper C, Fleming DM, et al. Zanamivir prophylaxis: an effective strategy for the prevention of influenza types A and B within households. J Infect Dis. 2002 Dec 1;186(11):1582-8.
48. Hayden FG, Pavia AT. Antiviral management of seasonal and pandemic influenza. J Infect Dis. 2006 Nov 1;194 Suppl 2:S119-26.
49. Balicer RD, Huerta M, Davidovitch N, Grotto I. Cost-benefit of stockpiling drugs for influenza pandemic. Emerg Infect Dis. 2005 Aug;11(8):1280-2.
50. Longini IM, Jr., Koopman JS, Haber M, Cotsonis GA. Statistical inference for infectious diseases. Risk-specific household and community transmission parameters. Am J Epidemiol. 1988 Oct;128(4):845-59.
51. Institute of Medicine; Committee on Modeling Community Containment for Pandemic Influenza. Modeling Community Containment for Pandemic Influenza. A Letter Report. Washington D.C.: The NationalAcademies Press; 2006. p.25.
52. Lipsitch M, Cohen T, Murray M, et al. Antiviral resistance and the control of pandemic influenza. PLoS Medicine. 2007;4:e15.
53. Olsen SJ, Ungchusak K, Sovann L, Uyeki TM, Dowell SF, Cox NJ, et al. Family clustering of avian influenza A (H5N1). Emerg Infect Dis. 2005 Nov;11(11):1799-801.
54. Watts DJ, Strogatz SH. Collective dynamics of 'small-world' networks. Nature. 1998 Jun 4;393(6684):440-2.
55. Newman ME, Park J. Why social networks are different from other types of networks. Phys Rev E Stat Nonlin Soft Matter Phys. 2003 Sep;68(3 Pt 2):036122.
56. Heymann A, Chodick G, Reichman B, Kokia E, Laufer J. Influence of school closure on the incidence of viral respiratory diseases among children and on health care utilization. Pediatr Infect Dis J. 2004 Jul;23(7):675-7.
57. Markel H. When Germs Travel: Six Epidemics That Invaded America Since 1900 and the Fears They Unleashed. New York: Pantheon/Random House; 2004.
58. Palla G, Derenyi I, Farkas I, Vicsek T. Uncovering the overlapping community structure of complex networks in nature and society. Nature. 2005 Jun 9;435(7043):814-8.
59. Lloyd-Smith JO, Galvani AP, Getz WM. Curtailing transmission of severe acute respiratory syndrome within a community and its hospital. Proc Royal Soc Biol Sci. 2003 Oct 7;270(1528):1979-89.
60. US General Services Administration. Childcare Center Design Guide, PBS-100. 2003 [cited 2007 January 23]; Available from: www.gsa.gov/gsa/cm_attachments/GSA_DOCUMENT/Design%20Guide_R2FD38_0Z5RDZ-i34K-pR.pdf
61. U.S. Department of Health and Human Services; Administration for Children and Families. Head Start Design Guide. Chapter 5: Planning Space and Location. 2005 [cited; 2nd:[Available from: www.headstartinfo.org/publications/hs_design_guide/chapter5.htm
62. Tanner CK. Minimum Classroom Size and Number of Students Per Classroom. 2000 [cited 2007 January 23]; Available from: www.coe.uga.edu/sdpl/research/territoriality.html
63. U.S. Department of Energy. Lawrence Berkeley National Laboratory, Commercial Heating and Cooling Loads Component Analysis, June 1998, Table 14. p.35. 2006 [cited 2007 January 23]; Available from: buildingsdatabook.eren.doe.gov/docs/7.4.5.pdf
64. U.S. Department of Energy. Lawrence Berkeley National Laboratory, Commercial Heating and Cooling Loads Component Analysis, June 1998, Table 10. p.31. 2006 [cited 2007 January 23]; Available from: buildingsdatabook.eren.doe.gov/docs/7.4.2.pdf
65. U.S. Department of Energy. Lawrence Berkeley National Laboratory, Commercial Heating and Cooling Loads Component Analysis, June 1998, Table 11. p.32. 2006 [cited 2007 January 23]; Available from: buildingsdatabook.eren.doe.gov/docs/7.4.4.pdf
66. U.S. Department of Commerce; Census Bureau; Housing and Household Economic Statistics Division. American Housing Survey for the United States, 2003. 2005 [cited 2007 January 23]; Available from: www.census.gov/hhes/www/housing/ahs/ahs03/tab23.htm
67. American Public Transportation Association. National Service and Operating Data. 2006. p.13 [cited 2007 January 23]; Available from: www.apta.com/research/stats/factbook/documents/section_06_passengers_pages_11_to_14.pdf
68. American Public Transportation Association. National Service and Operating Data. 2006. p.11 [cited 2007 January 23]; Available from: www.apta.com/research/stats/factbook/documents/section_06_passengers_pages_11_to_14.pdf
69. School Transportation News. K-12 Enrollment/Transportation Data, 2004-05 School Year. 2005 [cited 2007 January 23]; Available from: www.stnonline.com/stn/data_statistics/2004-05_schoolyear.htm
70. Principi N, Esposito S, Marchisio P, Gasparini R, Crovari P. Socioeconomic impact of influenza on healthy children and their families. Pediatr Infect Dis J. 2003 Oct;22(10 Suppl):S207-10.
71. Viboud C, Boelle PY, Cauchemez S, Lavenu A, Valleron AJ, Flahault A, et al. Risk factors of influenza transmission in households. Br J Gen Pract. 2004 Sep;54(506):684-9.
72. Brownstein JS, Kleinman KP, Mandl KD. Identifying pediatric age groups for influenza vaccination using a real-time regional surveillance system. Am J Epidemiol. 2005 Oct 1;162(7):686-93.
73. Becker NG, Dietz K. The effect of household distribution on transmission and control of highly infectious diseases. Math Biosci. 1995 Jun;127(2):207-19.
74. Becker NG, Hall R. Immunization levels for preventing epidemics in a community of households made up of individuals of various types. . Math Biosci. 1996;132(2):205-16.
75. Davis LE, Caldwell GG, Lynch RE, Bailey RE, Chin TD. Hong Kong influenza: the epidemiologic features of a high school family study analyzed and compared with a similar study during the 1957 Asian influenza epidemic. Am J Epidemiol. 1970 Oct;92(4):240-7.
76. Longini IM, Jr., Koopman JS, Monto AS, Fox JP. Estimating household and community transmission parameters for influenza. Am J Epidemiol. 1982 May;115(5):736-51.
77. King JC, Jr., Stoddard JJ, Gaglani MJ, Moore KA, Magder L, McClure E, et al. Effectiveness of school-based influenza vaccination. N Engl J Med. 2006 Dec 14;355(24):2523-32.
78. Paladini M. Do school holidays influence influenza related visits to the emergency department? (personal communication). 2007.
79. Kahn LH. Pandemic influenza school closure policies [letter]. Emerg Infect Dis. 2007;13(2):344.
80. Institute of Medicine; Committee on Modeling Community Containment for Pandemic Influenza. Modeling Community Containment for Pandemic Influenza. A Letter Report. Washington D.C.: The NationalAcademies Press; 2006. p.16.
81. Markel H, Lippman H. (personal communication). 2007.
82. Thompson WW, Comanor L, Shay DK. Epidemiology of seasonal influenza: use of surveillance data and statistical models to estimate the burden of disease. J Infect Dis. 2006 Nov 1;194 Suppl 2:S82-91.
83. Markel H. QUARANTINE! East European Jewish Immigrants and the New York City Epidemic of 1892. Baltimore: Johns Hopkins University Press; 1997.
84. Cetron M, Landwirth J. Public health and ethical considerations in planning for quarantine. Yale J Biol Med. 2005 Oct;78(5):329-34.
85. Bradley RH. Child care and common communicable illnesses in children aged 37 to 54 months. Arch Pediatr Adolesc Med. 2003 Feb;157(2):196-200.
86. U.S. Department of Commerce; U.S. Census Bureau. School Enrollment – Social and Economic Characteristics of Students: October 2003. Available at: www.census.gov/prod/2005pubs/p20-554.pdf
87. U.S. Department of Education; National Center for Education Statistics. Student Financing of Undergraduate Education: 2003-04. 2006 [cited 2007 January 23]; Available from: nces.ed.gov/pubs2006/2006186.pdf
88. Centers for Disease Control and Prevention. 121 Cities Mortality Reporting System. 2006 [cited 2007 January 23]; Available from: www.cdc.gov/ncphi/disss/nndss/phs.htm#121
89. Harvard School of Public Health. Pandemic Influenza and the Public; Survey Findings (press release). 2006 [cited 2007 January 23]; Available from: www.hsph.harvard.edu/press/releases/press10262006.html
90. Blendon RJ, Benson JM, Weldon KJ, et al. Pandemic Influenza and the Public; Survey Findings. 2006 [cited 2007 January 23]; Available from: www.hsph.harvard.edu/panflu/IOM_Avian_flu.ppt
91. The Public Engagement Project on Community Control Measures for Pandemic Influenza. 2006 [cited 2007 January 23]; Available from: www.keystone.org/Public_Policy/pandemic_control.html
92. U.S. Department of Labor; Office of the Assistant Secretary for Policy. Calculations from Current Population Survey (microdata). Washington, D.C.: U.S. Department of Labor; 2006.
93. U.S. Department of Commerce; U.S.Census Bureau. Who's Minding the Kids? Child Care Arrangements: Winter 2002. P70-101. 2005 [cited 2007 January 23]; Available from: www.census.gov/prod/2005pubs/p70-101.pdf
94. Helpguide. Aging Issues. 2004 [cited 2007 January 23]; Available from: www.helpguide.org/elder_care.htm
95. U.S. Department of Health and Human Services; Administration on Aging. Elderly Nutrition Program. 2003 [cited 2007 January 23]; Available from: www.aoa.gov/press/fact/pdf/fs_nutrition.pdf
96. Johnson A. 2007 (personal communication).
97. U.S. Department of Labor; Bureau of Labor Statistics. National Compensation Survey: Employee Benefits in the United States, March 2006. 2006 [cited 2007 January 23]; Available from: www.bls.gov/ncs/
98. U.S. Department of Agriculture; Food and Nutrition Service. National School Lunch Program. 2006 [cited 2007 January 23]; Available from: www.fns.usda.gov/cnd/lunch/aboutlunch/NSLPFactSheet.pdf
99. U.S. Department of Agriculture; Food and Nutrition Service. The School Breakfast Program. 2006 [cited 2007 January 23]; Available from: www.fns.usda.gov/cnd/lunch/aboutlunch/NSLPFactSheet.pdf
100. U.S. Department of Agriculture; Food and Nutrition Service. Child Nutrition Tables. National Summer Food Service Program. 2006 [cited 2007 January 23]; Available from: www.fns.usda.gov/pd/sfsummar.htm
101. Bernier-Toth M. U.S. Department of State (personal communication) 2007.
102. LTC Hachey W. U.S. Department of Defense (personal communication). 2007.
103. Triplett J. U.S. Department of State (personal communication). 2007.
104. Stohr K. Avian influenza and pandemics--research needs and opportunities. N Engl J Med. 2005 Jan 27;352(4):405-7.
105. Glezen WP. Emerging infections: pandemic influenza. Epidemiol Rev. 1996;18(1):64-76.
106. Hufnagel L, Brockmann D, Geisel T. Forecast and control of epidemics in a globalized world. Proc Natl Acad Sci U S A. 2004 Oct 19;101(42):15124-9.
107. Kilbourne ED. Influenza pandemics: can we prepare for the unpredictable? Viral Immunol. 2004;17(3):350-7.
108. Petric M, Comanor L, Petti CA. Role of the Laboratory in Diagnosis of Influenza during Seasonal Epidemics and Potential Pandemics. J Infect Dis. 2006 Nov 1;194 Suppl 2:S98-S110.
XV. Figures
Figure 1. Goals of Community Mitigation
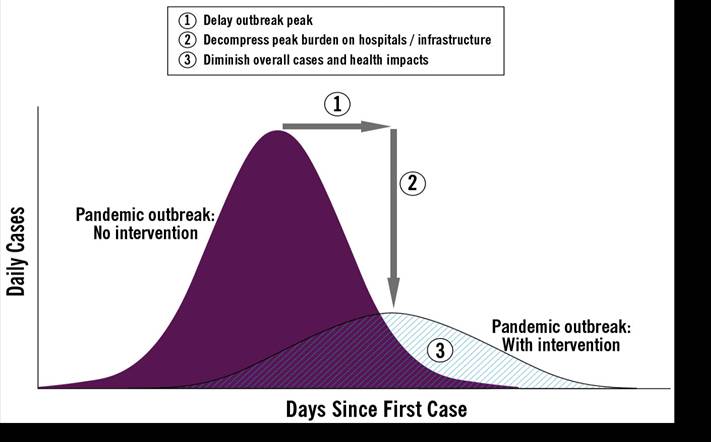
Figure 2. Effect of R0 on Hypothetical Epidemic Curves
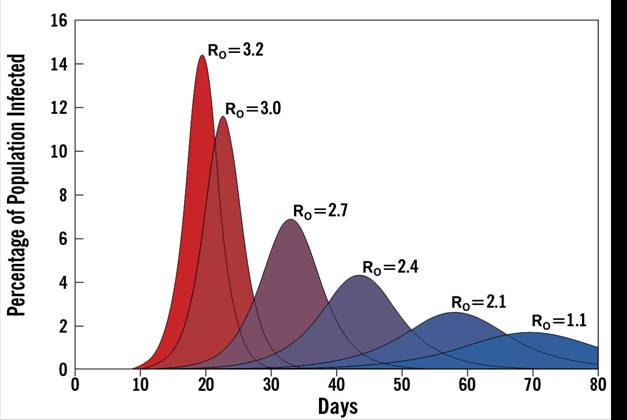
Source: Lewis (2006)
Figure 3a. Projected Mortality* of a Modern Influenza Pandemic Compared with That of 20th Century Pandemics (1918, 1957, 1968)
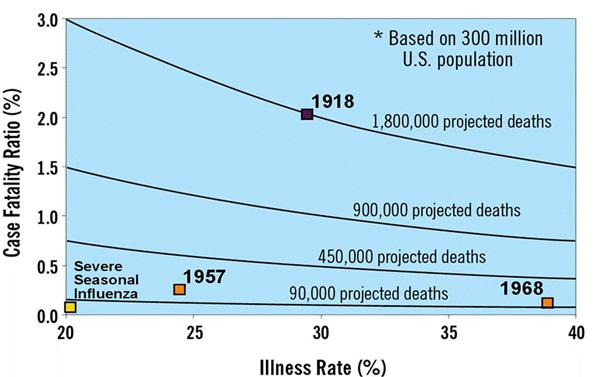
Figure 3b. Pandemic Severity Categories As Determined by Differences in Case Fatality Ratio
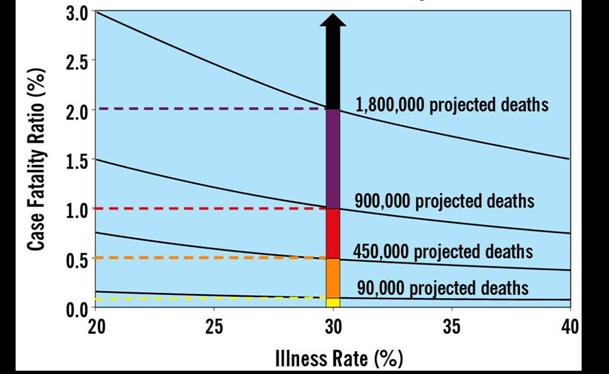
Figure 4. Pandemic Severity Index
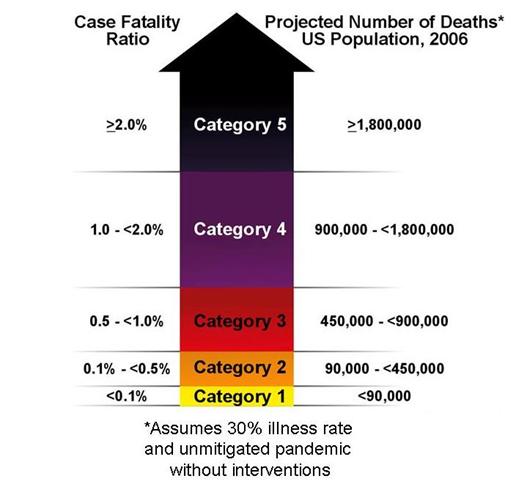
XVI. Tables
Table 1. Pandemic Severity Index by Epidemiologic Characteristics
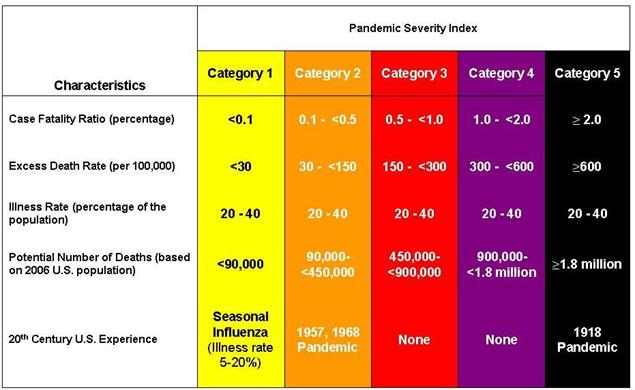
Table 2. Summary of the Community Mitigation Strategy by Pandemic Severity
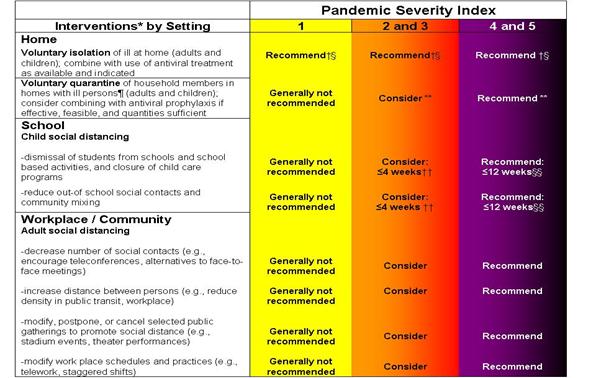
Generally Not Recommended = Unless there is a compelling rationale for specific populations or jurisdictions, measures are generally not recommended for entire populations as the consequences may outweigh the benefits.
Consider = Important to consider these alternatives as part of a prudent planning strategy, considering characteristics of the pandemic, such as age-specific illness rate, geographic distribution, and the magnitude of adverse consequences. These factors may vary globally, nationally, and locally.
Recommended = Generally recommended as an important component of the planning strategy.
*All these interventions should be used in combination with other infection control measures, including hand hygiene, cough etiquette, and personal protective equipment such as face masks. Additional information on infection control measures is available at www.pandemicflu.gov.
†This intervention may be combined with the treatment of sick individuals using antiviral medications and with vaccine campaigns, if supplies are available
§Many sick individuals who are not critically ill may be managed safely at home
¶The contribution made by contact with asymptomatically infected individuals to disease transmission is unclear. Household members in homes with ill persons may be at increased risk of contracting pandemic disease from an ill household member. These household members may have asymptomatic illness and may be able to shed influenza virus that promotes community disease transmission. Therefore, household members of homes with sick individuals would be advised to stay home.
**To facilitate compliance and decrease risk of household transmission, this intervention may be combined with provision of antiviral medications to household contacts, depending on drug availability, feasibility of distribution, and effectiveness; policy recommendations for antiviral prophylaxis are addressed in a separate guidance document.
††Consider short-term implementation of this measure—that is, less than 4 weeks.
§§Plan for prolonged implementation of this measure—that is, 1 to 3 months; actual duration may vary depending on transmission in the community as the pandemic wave is expected to last 6-8 weeks.
Table 3. Triggers for Implementation of Mitigation Strategies by Pandemic Severity Index and U.S. Government Stages
Alert: Notification of critical systems and personnel of their impending activation.
Standby: Initiate decision-making processes for imminent activation, including mobilization of resources and personnel.
Activate: Implementation of the community mitigation strategy.
*Widespread human outbreaks in multiple locations overseas.
†First human case in North America.
§Spread throughout the United States.
¶Recommendations for regional planning acknowledge the tight linkages that may exist between cities and metropolitan areas that are not encompassed within state boundaries.
**Standby applies. However, Alert actions for Category 4 and 5 should occur during WHO Phase 5, which corresponds to U.S. Government Stage 2.
††Standby/Activate Standby applies unless the laboratory-confirmed case cluster and community transmission occurs within a given jurisdiction, in which case that jurisdiction should proceed directly to Activate community interventions defined in Table 2.
XVII. Appendices
Appendix 1 - Glossary of Terms
Absenteeism rate: Proportion of employed persons absent from work at a given point in time or over a defined period of time.
Antiviral medications: Medications presumed to be effective against potential pandemic influenza virus strains and which may prove useful for treatment of influenza-infected persons or for prophylactic treatment of persons exposed to influenza to prevent them from becoming ill. These antiviral medications include the neuraminidase inhibitors oseltamivir (Tamiflu®) and zanamivir (Relenza®).
Case fatality ratio: Proportion of deaths among clinically ill persons.
Childcare: Childcare programs discussed in this guidance include 1) centers or facilities that provide care to any number of children in a nonresidential setting, 2) large family childcare homes that provide care and education for seven or more children in the home of the provider, and 3) small family childcare homes that provide care to six or fewer children in the home of the provider.
Children: In this document children are defined as 17 years of age or younger unless an age is specified or 12 years of age or younger if teenagers are specified.
Clinically ill: Those persons who are infected with pandemic influenza and show signs and symptoms of illness.
Colleges: Post-high school educational institutions (i.e., beyond 12th grade).
Community mitigation strategy: A strategy for the implementation at the community level of interventions designed to slow or limit the transmission of a pandemic virus.
Cough etiquette: Covering the mouth and nose while coughing or sneezing; using tissues and disposing in no-touch receptacles; and washing of hands often to avoid spreading an infection to others.
Countermeasures: Refers to pre-pandemic and pandemic influenza vaccine and antiviral medications.
Critical infrastructure: Systems and assets, whether physical or virtual, so vital to the United States that the incapacitation or destruction of such systems and assets would have a debilitating impact on national security, economy, or public health and/or safety, either alone or in any combination. Specifically, it refers to the critical infrastructure sectors identified in Homeland Security Presidential Directive 7 (HSPD-7).
Early, targeted, and layered nonpharmaceutical interventions (NPIs) strategy: A strategy for using combinations of selected community-level NPIs implemented early and consistently to slow or limit community transmission of a pandemic virus.
Excess rate: Rate of an outcome (e.g., deaths, hospitalizations) during a pandemic above the rate that occurs normally in the absence of a pandemic. It may be calculated as a ratio over baseline or by subtracting the baseline rate from the total rate.
Face mask: Disposable surgical or procedure mask covering the nose and mouth of the wearer and designed to prevent the transmission of large respiratory droplets that may contain infectious material.
Faith-based organization: Any organization that has a faith-inspired interest.
Generation time: Average number of days taken for an ill person to transmit the infection to another person.
Hand hygiene: Hand washing with either plain soap or antimicrobial soap and water or use of alcohol-based products (gels, rinses, foams containing an emollient) that do not require the use of water.
Illness rate or clinical attack rate: Proportion of people in a community who develop illness (symptomatic cases ÷ population size).
Incident of National Significance: Designation is based on criteria established in Homeland Security Presidential Directive 5 and include events with actual or potential high-impact that requires a coordinated and effective response by Federal, State, local, tribal, nongovernmental, and/or private sector entities in order to save lives, minimize damage, and provide the basis for long-term community recovery and mitigation activities.
Incubation period: The interval (in hours, days, or weeks) between the initial, effective exposure to an infectious organism and the first appearance of symptoms of the infection.
Infection control: Hygiene and protective measures to reduce the risk of transmission of an infectious agent from an infected person to uninfected persons (e.g., hand hygiene, cough etiquette, use of personal protective equipment, such as face masks and respirators, and disinfection).
Influenza pandemic:A worldwide epidemic caused by the emergence of a new or novel influenza strain to which humans have little or no immunity and which develops the ability to infect and be transmitted efficiently and between humans for a sustained period of time in the community.
Isolation of ill people: Separation or restriction of movement of persons ill with an infectious disease in order to prevent transmission to others.
Mortality rate: Number of deaths in a community divided by population size of community over a specific period of time (e.g., 20 deaths per 100,000 persons per week).
Nonpharmaceutical intervention (NPI): Mitigation measure implemented to reduce the spread of an infectious disease (e.g., pandemic influenza) but one that does not include pharmaceutical products, such as vaccines and medicines. Examples include social distancing and infection control measures.
Pandemic vaccine: Vaccine for a specific influenza virus strain that has evolved the capacity for sustained and efficient human-to-human transmission. This vaccine can only be developed once the pandemic strain emerges.
Personal protective equipment (PPE): PPE is any type of clothing, equipment, or respiratory protection device (respirators) used to protect workers against hazards they encounter while doing their jobs. PPE can include protection for eyes, face, head, torso, and extremities. Gowns, face shields, gloves, face masks, and respirators are examples of PPE commonly used within healthcare facilities. When PPE is used in a workplace setting to protect workers against workplace hazards, its use must be consistent with regulations issued by the Occupational Safety and Health Administration (www.osha.gov/index.html).
Post-exposure prophylaxis: The use of antiviral medications in individuals exposed to others with influenza to prevent disease transmission.
Pre-pandemic vaccine: Vaccine against strains of influenza virus in animals that have caused isolated infections in humans and which may have pandemic potential. This vaccine is prepared prior to the emergence of a pandemic strain and may be a good or poor match (and hence of greater or lesser protection) for the pandemic strain that ultimately emerges.
Prophylaxis: Prevention of disease or of a process that can lead to disease. With respect to pandemic influenza, this specifically refers to the administration of antiviral medications to healthy individuals for the prevention of influenza.
Quarantine: A restraint upon the activities or communication (e.g., physical separation or restriction of movement within the community/work setting) of an individual(s) who has been exposed to an infection but is not yet ill to prevent the spread of disease; quarantine may be applied voluntarily (preferred) or on compulsory basis dependent on legal authority.
Rapid diagnostic test: Medical test for rapidly confirming the presence of infection with a specific influenza strain.
Recrudescence: Reappearance of a disease after it has diminished or disappeared.
R0 (“reproductive number”): Average number of infections resulting from a single case in a fully susceptible population without interventions.
Schools: Refers to public and private elementary, middle, secondary, and post-secondary schools (colleges and universities).
Schools (K-12): Refers to schools, both public and private, spanning the grades kindergarten through 12th grade (elementary through high school).
Seasonal influenza: Influenza virus infections in familiar annual patterns.
Second- and third-order effects: Chains of effects that may arise as a consequence of intervention and which may require additional planning and intervention to mitigate. These terms generally refer to foreseeable unintended consequences of intervention. For example, dismissal of students from school classrooms may lead to workplace absenteeism for child minding. Subsequent workplace closings due to high absenteeism may lead to loss of income for employees, a third-order effect that could be detrimental to families living at or near subsistence levels.
Sector: A subdivision (sociological, economic, or political) of society.
Social distancing: Measures to increase the space between people and decrease the frequency of contact among people.
Surge capacity: Refers to the ability to expand provision of services beyond normal capacity to meet transient increases in demand. Surge capacity within a medical context includes the ability of healthcare or laboratory facilities to provide care or services above their usual capacity and to expand manufacturing capacity of essential medical materiel (e.g., vaccine) to meet increased demand.
Surgical mask: Disposable face mask that covers the mouth and nose and comes in two basic types. The first type is affixed to the head with two ties and typically has a flexible adjustment for the nose bridge. This type of surgical mask may be flat/pleated or duck-billed in shape. The second type of surgical mask is pre-molded, or cup shaped, and adheres to the head with a single elastic strap and usually has a flexible adjustment for the nose bridge. Surgical masks are used to prevent the transmission of large particles.
Telework:Refers to activity of working away from the usual workplace (often at home) through telecommunication or other remote access means (e.g., computer, telephone, cellular phone, fax machine).
Universities: Educational institutions beyond 12th grade (post high school).
Viral shedding: Discharge of virus from an infected person.
Virulence: The ability of the pathogen to produce disease; or the factors associated with the pathogen to affect the severity of diseases in the host.
Voluntary: Acting or done of one’s own free will without legal compulsion (e.g., voluntary household quarantine).
Appendix 2 – Interim Guidance Development Process
This guidance document was developed through a collaborative process that gathered input from a variety of sources, including subject-matter experts, peer-reviewed scientific literature, current research, and stakeholders (i.e., federal agencies, public health officials, and the public). A working group composed of Federal, State, and local public health officials and representatives from the Association of State and Territorial Health Officials (ASTHO), the Council of State and Territorial Epidemiologists (CSTE), the National Association of County and City Health Officials (NACCHO), the Infectious Disease Society of America (IDSA), and the National Association of Local Boards of Health (NALBOH) met periodically to review and evaluate evidence derived from the following sources:
- Preliminary statistical analyses of historical data on the implementation of selected NPIs in U.S. cities during the 1918 pandemic.
- Stakeholder input from interagency outreach meetings with public health, private sector, labor unions, and community partners.
- Proceedings of community public engagement meetings conducted in five U.S. cities (Atlanta, GA; Lincoln, NE; Seattle, WA; Syracuse, NY; Washington, DC) in October-November 2006.
- Public opinion poll results conducted by the Harvard School of Public Health in September-October 2006 surveying 1,697 adults in the United States regarding their willingness to follow public health officials’ recommendations for selected pandemic mitigation interventions.
- Peer-reviewed mathematical modeling to assess potential pandemic mitigation interventions during an influenza pandemic.
- Expert opinion of public health officials, including published findings and recommendations of the Committee on Modeling Community Containment for Pandemic Influenza (Institute of Medicine, 2006).
- Preliminary results from a November 2006 Epi-Aid investigation of a seasonal influenza outbreak with associated school closure.
- Preliminary results from review of legal authorities/policies of school closure in each state conducted by the Center for Law and the Public’s Health.
In addition, stakeholders from government, academia, private industry, educational organizations, and faith-based and community organizations reviewed and evaluated these data during public stakeholder meetings in June and December 2006. The opinions from individuals in the working group and stakeholders were considered during the writing of this guidance.
Pandemic planning with respect to the implementation of these pandemic mitigation interventions must be citizen-centric and support the needs of people across society in as equitable a manner as possible. Accordingly, the process for developing this interim pre-pandemic guidance sought input from key stakeholders, including the public. While all views and perspectives were respected, a hierarchy of values did in fact emerge over the course of the deliberations. In all cases, the question was whether the cost of the interventions was commensurate with the benefits they could potentially provide. Thus, there was more agreement on what should be done when facing a severe pandemic with a high case fatality ratio (e.g., a 1918-like pandemic) than on what should be done when facing a pandemic with a lower case fatality ratio (e.g., a 1968-like pandemic); even with the inherent uncertainties involved, the cost-benefit ratio of the interventions clearly becomes more favorable as the severity increases and the number of lives potentially saved increases. Many stakeholders, for example, expressed concern about the effectiveness of the proposed interventions, which cannot be demonstrated a priori and for which the evidence base is limited and of variable quality. However, where high rates of mortality could be anticipated in the absence of intervention, a significant majority of stakeholders expressed their willingness to “risk” undertaking interventions of uncertain effectiveness in mitigating disease and death. Where scenarios that would result in 1918-like mortality rates were concerned, most stakeholders reported that aggressive measures would be warranted and that the value of the lives potentially saved assumed precedence over other considerations. However, the feasibility of these approaches has not been assessed at the community level. Local, State, regional, and Federal exercises will need to be conducted to obtain more information about the feasibility and acceptance of these measures. In addition, ongoing engagement with the public, especially vulnerable populations, is essential.
CDC Community Mitigation Strategy Team acknowledges the following for their contributions to the development of this document:
Department of Health and Human Services National Association of Local Health Boards
Department of Commerce MIDAS Modelers
Department of Defense University of Michigan
Department of Education
Department of Homeland Security
Department of the Interior
Department of Justice
Department of Labor
Department of State
Department of Transportation
Department of the Treasury
U.S. Department of Agriculture
U.S. Environmental Protection Agency
U.S. Office of Personnel Management
Department of Veterans Affairs
White House Homeland Security Council
Association of State and Territorial Health Officials
Council of State and Territorial Epidemiologists
Harvard School of Public Health
Infectious Disease Society of America
Institute of Medicine
National Association of County and City Health Officials
Appendix 3 - WHO Phases of a Pandemic/U.S. Government Stages of a Pandemic
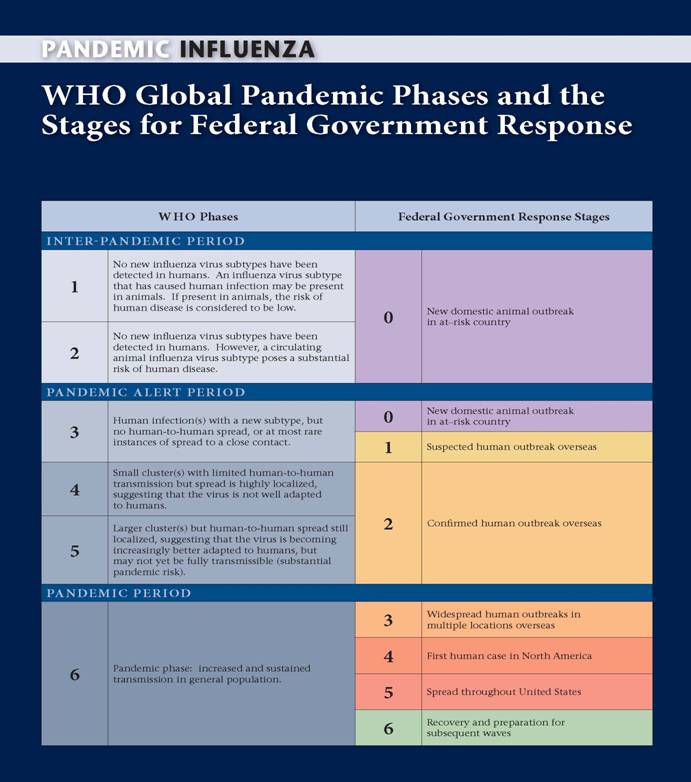
Appendix 4 - Pandemic Influenza Community Mitigation Interim Planning Guide for Businesses and Other Employers
Purpose
This Interim Planning Guide for Businesses and Other Employers is provided as a supplement to the Interim Pre-Pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States—Early, Targeted, Layered Use of Nonpharmaceutical Interventions. This guide is intended to assist in pre-pandemic planning. Individuals and families, employers, schools, and other organizations will be asked to take certain steps (described below) to help limit the spread of a pandemic, mitigate disease and death, lessen the impact on the economy, and maintain societal functioning. This guidance is based upon the best available current data and will be updated as new information becomes available. During the planning process, Federal, State, local, tribal, and territorial officials should review the laws, regulations, and policies that relate to these recommendations, and they should include stakeholders in the planning process and resolution of issues.
Businesses and other employers (including local, State, and Federal agencies and other organizations) will be essential partners in protecting the public’s health and safety when a pandemic occurs. This Pandemic Influenza Community Mitigation Interim Planning Guide for Businesses and Other Employers provides guidance to these groups by describing how they might prepare for, respond to, and recover from an influenza pandemic. When an influenza pandemic starts, public health officials will determine the severity of the pandemic and recommend actions to protect the community’s health. People who become severely ill may need to be cared for in a hospital. However, most people with influenza will be safely cared for at home.
Community mitigation recommendations will be based on the severity of the pandemic and may include the following:
- Asking ill people to voluntarily remain at home and not go to work or out in the community for about 7-10 days or until they are well and can no longer spread the infection to others (ill individuals may be treated with influenza antiviral medications, as appropriate, if these medications are effective and available).
- Asking members of households with a person who is ill to voluntarily remain at home for about 7 days (household members may be provided with antiviral medications, if these medications are effective and sufficient in quantity and feasible mechanisms for their distribution have been developed).
- Dismissing students from schools (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs for up to 12 weeks, coupled with protecting children and teenagers through social distancing in the community, to include reductions of out-of-school social contacts and community mixing. Childcare programs discussed in this guidance include centers or facilities that provide care to any number of children in a nonresidential setting, large family childcare homes that provide care for seven or more children in the home of the provider, and small family childcare homes that provide care to six or fewer children in the home of the provider.1
- Recommending social distancing of adults in the community, which may include cancellation of large public gatherings; changing workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services; ensuring work-leave policies to align incentives and facilitate adherence with the measures outlined above.
Planning now for a severe pandemic (and adjusting your continuity plan accordingly) will help assure that your business is prepared to implement these community recommendations. Businesses and other employers should be prepared to continue the provision of essential services during a pandemic even in the face of significant and sustained absenteeism. Pandemic preparation should include coordinated planning with employees and employee representatives and critical suppliers. Businesses should also integrate their planning into their communities' planning. These preparedness efforts will be beneficial to your organization, staff, and the community, regardless of the severity of the pandemic. The following provide information to guide business planning for a pandemic: Business Pandemic Influenza Planning Checklist (www.pandemicflu.gov/plan/business/businesschecklist.html), the Pandemic Preparedness Planning for U.S. Businesses with Overseas Operations Checklist, (www.pandemicflu.gov/plan/business/businessesoverseaspdf.pdf), and the Pandemic Influenza Preparedness, Response and Recovery Guide for Critical Infrastructure and Key Resources (www.pandemicflu.gov/plan/pdf/cikrpandemicinfluenzaguide.pdf). In addition, recommendations for implementation of pandemic mitigation strategies are available at www.pandemicflu.gov. Reliable, accurate, and timely information on the status and severity of the pandemic also will be posted on www.pandemicflu.gov. Additional information is available from the Centers for Disease Control and Prevention (CDC) Hotline: 1-800-CDC-INFO (1-800-232-4636). This line is available in English and Spanish, 24 hours a day, 7 days a week. TTY: 1-888-232-6348. Questions can be e-mailed to cdcinfo@cdc.gov.
Recommendations for Planning
1. Plan for ill individuals to remain at home
- Plan for staff absences during a pandemic due to personal illness.
- Encourage ill persons to stay home during a pandemic and establish return-to-work policies after illness.
- Identify critical job functions and plan for their continuity and how to temporarily suspend non-critical activities, cross-train employees to cover critical functions, and cover the most critical functions with fewer staff.
- Identify employees who might need extra assistance to stay home when they are ill because, for example, they live alone or have a disability.
- Review Federal and State employment laws that identify your employer obligations and options for employees.
- Establish and clearly communicate policies on sick (and other) leave and employee compensation.
- Develop a workplace culture that recognizes and encourages behaviors such as voluntarily staying home when ill in order to recover and to avoid spreading infection to others.
- Develop policies on what to do when a person becomes ill at the workplace.
- Provide employees with information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov.
2. Plan for all household members of a person who is ill to voluntarily remain at home
- Plan for staff absences related to family member illness.
- Identify critical job functions and plan for their continuity and how to temporarily suspend non-critical activities, cross-train employees to cover critical functions, and cover the most critical functions with fewer staff.
- Establish policies for an alternate or flexible worksite (e.g., work via the internet, e-mailed or mailed work assignments) and flexible work hours, where feasible.
- Develop guidelines to address business continuity requirements created by jobs that will not allow teleworking (e.g., production or assembly line workers).
- Establish and clearly communicate policies on family leave and employee compensation, especially Federal laws and laws in your State regarding leave of workers who need to care for an ill family member or voluntarily remain home.
- Provide employees with information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov.
3. Plan for dismissal of students and childcare closure
- Identify employees who may need to stay home if schools dismiss students and childcare programs close during a severe pandemic.
- Advise employees not to bring their children to the workplace if childcare cannot be arranged.
- Plan for alternative staffing or staffing schedules on the basis of your identification of employees who may need to stay home.
- Identify critical job functions and plan now for cross-training employees to cover those functions in case of prolonged absenteeism during a pandemic.
- Establish policies for employees with children to work from home, if possible, and consider flexible work hours and schedules (e.g., staggered shifts).
- Encourage employees who have children in their household to make plans to care for their children if officials recommend dismissal of students from schools, colleges, universities, and childcare programs. Advise employees to plan for an extended period (up to 12 weeks) in case the pandemic is severe.
- In a severe pandemic, parents would be advised to protect their children by reducing out-of-school social contacts and mixing with other children. Although limiting all outside contact may not be feasible, parents may be able to develop support systems with co-workers, friends, families, or neighbors if they continue to need childcare. For example, they could prepare a plan in which two to three families work together to supervise and provide care for a small group of infants and young children while their parents are at work (studies suggest that childcare group size of less than six children may be associated with fewer respiratory infections).2
- Talk with your employees about any benefits, programs, or other assistance they may be eligible for if they have to stay home to mind children for a prolonged period during a pandemic.
- Coordinate with State and local government and faith-based and community-based organizations to assist workers who cannot report to work for a prolonged period.
4. Plan for workplace and community social distancing measures
- Become familiar with social distancing methods that may be used during a pandemic to modify the frequency and type of person-to-person contact (e.g., reducing hand-shaking, limiting face-to-face meetings and shared workstations, promoting teleworking, offering liberal/unscheduled leave policies, staggered shifts).
- Plan to operate businesses and other workplaces using social distancing and other measures to minimize close contact between and among employees and customers. Determine how the work environment may be reconfigured to allow for more distance between employees and between employees and customers during a pandemic. If social distancing is not feasible in some work settings, employ other protective measures (guidance available at www.pandemicflu.gov).
- Review and implement guidance from the Occupational Safety and Health Administration (OSHA) to adopt appropriate work practices and precautions to protect employees from occupational exposure to influenza virus during a pandemic. Risk of occupational exposure to influenza virus depends in part on whether or not jobs require close proximity to people potentially infected with the pandemic influenza virus or whether employees are required to have either repeated or extended contact with the public. OSHA will post and periodically update such guidance on www.pandemicflu.gov.
- Encourage good hygiene at the workplace. Provide employees and staff with information about the importance of hand hygiene (information can be found at www.cdc.gov/cleanhands/) as well as convenient access to soap and water and/or alcohol-based hand gel in your facility. Educate employees about covering their cough to prevent the spread of germs (www.cdc.gov/flu/protect/covercough.htm).
5. Communicate with your employees and staff
- Disseminate your company’s pandemic plan to all employees and stakeholders in advance of a pandemic; include roles/actions expected of employees and other stakeholders during implementation of the plan.
- Provide information to encourage employees (and their families) to prepare for a pandemic by providing preparedness information. Resources are available at www.pandemicflu.gov/plan/individual/checklist.html.
6. Help your community
- Coordinate your business’ pandemic plans and actions with local health and community planning.
- Find volunteers in your business who want to help people in need, such as elderly neighbors, single parents of small children, or people without the resources to get the medical or other help they will need.
- Think of ways your business can reach out to other businesses and others in your community to help them plan for a pandemic.
- Participate in community-wide exercises to enhance pandemic preparedness.
7. Recovery
- Assess criteria that need to be met to resume normal operations and provide notification to employees of activation of the business resumption plan.
- Assess the availability of medical, mental health, and social services for employees after the pandemic.
References:
1 American Academy of Pediatrics. Children in Out-of-Home Child Care: Classification of Care Service. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003:124.
2 Bradley RH. Child care and common communicable illnesses in children aged 37 to 54 months. Arch Pediatr Adolesc Med. 2003 Feb;157(2):196-200
Appendix 5 - Pandemic Influenza Community Mitigation Interim Planning Guide for Childcare Programs
Purpose
This Interim Planning Guide for Childcare Programs is provided as a supplement to the Interim Pre-Pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States—Early, Targeted, Layered Use of Nonpharmaceutical Interventions. The guide is intended to assist in pre-pandemic planning. Individuals and families, employers, schools, and other organizations will be asked to take certain steps (described below) to help limit the spread of a pandemic, mitigate disease and death, lessen the impact on the economy, and maintain societal functioning. This guidance is based upon the best available current data and will be updated as new information becomes available. During the planning process, Federal, State, local, tribal, and territorial officials should review the laws, regulations, and policies that relate to these recommendations, and they should include stakeholders in the planning process and resolution of issues.
Childcare programs will be essential partners in protecting the public’s health and safety when an influenza pandemic occurs. Childcare programs discussed in this guidance include centers or facilities that provide care to any number of children in a nonresidential setting, large family childcare homes that provide care for seven or more children in the home of the provider and small family childcare homes that provide care to six or fewer children in the home of the provider.1 This Pandemic Influenza Community Mitigation Interim Planning Guide for Childcare Programs provides guidance describing how such programs might prepare for and respond to an influenza pandemic. When an influenza pandemic starts, public health officials will determine the severity of the pandemic and recommend actions to protect the community’s health. People who become severely ill may need to be cared for in a hospital. However, most people with influenza will be safely cared for at home.
Community mitigation recommendations will be based on the severity of the pandemic and may include the following:
- Asking ill people to voluntarily remain at home and not go to work or out in the community for about 7-10 days or until they are well and can no longer spread the infection to others (ill individuals will be treated with influenza antiviral medications, as appropriate, if these medications are effective and available).
- Asking members of households with a person who is ill to voluntarily remain at home for about 7 days (household members may be provided with antiviral medications, if these medications are effective and sufficient in quantity and feasible mechanisms for their distribution have been developed).
- Dismissing students from schools (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs for up to 12 weeks, coupled with protecting children and teenagers through social distancing in the community to include reductions of out-of-school social contacts and community mixing.
- Recommending social distancing of adults in the community, which may include cancellation of large public gatherings; changing workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services; ensuring work-leave policies to align incentives and facilitate adherence with the measures outlined above.
Recommendations for closing childcare facilities will depend upon the severity of the pandemic. The current three-tiered planning approach includes 1) no closure in a Category 1 pandemic, 2) short-term (up to 4 weeks) closure of childcare facilities in a Category 2 or Category 3 pandemic, and 3) prolonged (up to 12 weeks) closure of childcare facilities in a severe influenza pandemic (Category 4 or Category 5). These actions may only apply to traditional forms of center-based care and large family childcare programs (more than six children). Small family childcare programs (less than seven children) may be able to continue operations.
In the most severe pandemic, the duration of these public health measures would likely be for 12 weeks and will undoubtedly have serious financial implications for childcare workers and their employers as well as for families who depend on their services. In a severe pandemic, parents will be advised to protect their children by reducing out-of-school social contacts and mixing with other children. Although limiting all outside contact may not be feasible, families may be able to develop support systems with co-workers, friends, families, or neighbors if they continue to need childcare. For example, they could prepare a plan in which two or three families work together to supervise and provide care for a small group of infants and young children while their parents are at work (studies suggest that childcare group size of less than six children may be associated with fewer respiratory infections).2
Planning now for a severe pandemic will help assure that your childcare program is prepared to implement these community recommendations. These preparedness efforts will be beneficial to your programs, staff, families, and the community, regardless of the severity of the pandemic. The Pandemic Flu Planning Checklist for Childcare Facilities (www.pandemicflu.gov/plan/school/index.html) provides an approach to planning for a pandemic. Recommendations for implementation of pandemic mitigation strategies are available at www.pandemicflu.gov. Reliable, accurate, and timely information on the status and severity of the pandemic will be posted on www.pandemicflu.gov. Additional information is available from the Centers for Disease Control and Prevention (CDC) Hotline: 1-800-CDC-INFO (1-800-232-4636). This line is available in English and Spanish, 24 hours a day, 7 days a week. TTY: 1-888-232-6348. Questions can be e-mailed to cdcinfo@cdc.gov.
Recommendations for Planning
1. Plan for ill individuals to remain at home
- Develop a plan of childcare operations for implementation during pandemics of all levels of severity.
- Develop a plan for employee absences due to personal illness. Plan for alternative staffing:
- Identify critical job functions and plan for alternate coverage of those functions during a pandemic. Family childcare programs may consider prearranging childcare coverage with other providers in their areas.
- Review and analyze Federal and State employment laws that identify employer obligations and options for personnel.
- Establish and clearly communicate policies on sick leave and employee compensation.
- Encourage ill persons to stay home during a pandemic and establish return-to-work policies after illness.
- Establish policies for sick-leave absences unique to a pandemic (e.g., liberal/unscheduled leave).
- Develop policies on observation for illness and what to do when a child or employee becomes ill at the workplace.
- Advise employees to look for information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov.
2. Plan for all household members of a person who is ill to voluntarily remain at home
- Develop a plan for employee absences related to family member illness. Plan for alternate staffing:
- Identify critical job functions and plan now for coverage of those functions.
- Review Federal and State employment laws that identify your employer obligations and options for employees.
- Establish and clearly communicate policies on family leave and employee compensation.
- Establish policies for sick-leave absences unique to a pandemic (e.g., liberal/unscheduled leave).
- Establish policies for employees who have to stay home because someone in their household is ill with pandemic influenza.
- Be familiar with Federal and State laws regarding leave of workers who need to care for an ill family member or voluntarily remain at home.
- Advise employees to look for information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov.
3. Plan for dismissal of students from school and childcare closure, considering the impact on employees and parents
- Develop a plan for program operations during all levels of pandemic severity.
- Plan for alternate staffing based on your assessment.
- Identify critical job functions and plan now for coverage of those functions in case of prolonged absenteeism during a pandemic.
- Work with State and local government and faith-based and community-based organizations to provide any needed assistance to staff who are not able to work for a prolonged period of time.
4. Plan for workplace and community social distancing measures
- Become familiar with social distancing actions that may be used during a pandemic to modify frequency and type of person-to-person contact (e.g., reducing hand-shaking, limiting face-to-face meetings, promoting teleworking, and offering liberal/unscheduled leave policies and staggered shifts).
- Plan to operate the workplace using social distancing and other measures to minimize close contact between employees.
- Review and implement guidance from the Occupational Safety and Health Administration (OSHA) on appropriate work practices and precautions to protect employees from occupational exposure to influenza virus during a pandemic. Risks of occupational exposure to influenza virus depends in part on whether jobs require close proximity to people who may be infectious with the pandemic influenza virus or whether employees are required to have either repeated or extended contact with the general public. OSHA will post and periodically update such guidance on www.pandemicflu.gov.
- If the childcare program is to remain in operation during a Category 1-3 pandemic, provide staff with information about the measures that the program will institute in order to reduce virus transmission among staff and children. These may include
- Restructuring and keeping groups of staff and children from mixing together to minimize social contacts.
- Asking ill staff to stay home while they are ill.
- Modifying exclusion policies to include ill children and possibly, based on public health recommendations made at the time of the pandemic, those with ill family members.
- Implementing staggered shifts.
- Implementing social distancing practices, including
- Eliminating gatherings of staff and
- Minimizing contact between staff and parents.
- Encourage good hygiene at the workplace. Provide children and staff with information about the importance of hand hygiene (information can be found at www.cdc.gov/cleanhands/) as well as convenient access to soap and water and alcohol-based hand gel in your facility. Educate employees and children about covering their cough to prevent the spread of germs (see www.cdc.gov/flu/protect/covercough.htm).
- Promote social distancing of children outside the childcare setting by advising parents that children reduce their social interaction and contacts to the greatest extent possible.
5. Communicate with staff and parents/families
- Be prepared to provide parents/families with information about
- Why programs will be cancelled and the importance of keeping infants and children from congregating with other children in the community.
- How alternative childcare options may be accessed.
- How students who need free meals may qualify for other types of nutrition assistance in the community.
- Provide information to staff and parents/families on what they can do to prepare their families for a pandemic. Resources are available at www.pandemicflu.gov/plan/individual/checklist.html and www.ready.gov/america/index.html.
- Provide systematic emergency communications to childcare staff and families during the pandemic. Use a telephone calling tree, an e-mail alert, or call-in voice recording to communicate pandemic status in the community and status of childcare program activities. Messages for staff and families should be targeted and provided in the different languages that reflect the languages within the community.
- Recommend that parents/families seek further information about pandemic through other sources including key Federal, State, local, tribal, and territorial public health resources and regularly provided pandemic updates at www.pandemicflu.gov.
6. Help your community
- Coordinate your pandemic plans and actions with local health and community planning.
- Think of ways your childcare program can reach out to other childcare programs and others in your community to help them plan for a pandemic.
- Participate in community-wide exercises to enhance pandemic preparedness.
7. Recovery
- Establish the criteria and procedures for resuming childcare operations and activities.
- Develop communication plans for advising employees, staff, and families of the resumption of programs and activities.
- Develop the procedures, activities, and services needed to restore the childcare environment.
References:
1 American Academy of Pediatrics. Children in Out-of-Home Child Care: Classification of Care Service. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003:124.
2 Bradley RH. Child care and common communicable illnesses in children aged 37 to 54 months. Arch Pediatr Adolesc Med. 2003 Feb;157(2):196-200
Appendix 6 - Pandemic Influenza Community Mitigation Interim Planning Guide for Elementary and Secondary Schools
Purpose
This Interim Planning Guide for Elementary and Secondary Schools is provided as a supplement to the Interim Pre-Pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States—Early, Targeted, Layered Use of Nonpharmaceutical Interventions. The guide is intended to assist in pre-pandemic planning. Individuals and families, employers, schools, and other organizations will be asked to take certain steps (described below) to help limit the spread of a pandemic, mitigate disease and death, lessen the impact on the economy, and maintain societal functioning. This guidance is based upon the best available current data and will be updated as new information becomes available. During the planning process, Federal, State, local, tribal, and territorial officials should review the laws, regulations, and policies that relate to these recommendations, and they should include stakeholders in the planning process and resolution of issues.
Schools will be essential partners in protecting the public’s health and safety when an influenza pandemic occurs. This Pandemic Influenza Community Mitigation Interim Planning Guide for Elementary and Secondary Schools provides guidance to educational institutions, describing how they might prepare for and respond to an influenza pandemic. When an influenza pandemic starts, public health officials will determine the severity of the pandemic and recommend actions to protect the community’s health. People who become severely ill may need to be cared for in a hospital. However, most people with influenza will be safely cared for at home.
Community mitigation recommendations will be based on the severity of the pandemic and may include the following:
- Asking ill people to voluntarily remain at home and not go to work or out in the community for about 7-10 days or until they are well and can no longer spread the infection to others (ill individuals will be treated with influenza antiviral medications, as appropriate, if these medications are effective and available).
- Asking members of households with a person who is ill to voluntarily remain at home for about 7 days (household members may be provided with antiviral medications, if these medications are effective and sufficient in quantity and feasible mechanisms for their distribution have been developed).
- Dismissing students from schools (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs for up to 12 weeks, coupled with protecting children and teenagers through social distancing in the community to include reductions of out-of-school social contacts and community mixing. Childcare programs discussed in this guidance include centers or facilities that provide care to any number of children in a nonresidential setting, large family childcare homes that provide care for seven or more children in the home of the provider and small family childcare homes that provide care to six or fewer children in the home of the provider.1
- Recommending social distancing of adults in the community, which may include cancellation of large public gatherings; changing workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services; ensuring work-leave policies to align incentives and facilitate adherence with the measures outlined above.
Recommendations for dismissing students from classes will depend upon the severity of the pandemic. The current three-tiered planning approach includes 1) no dismissals in a Category 1 pandemic, 2) short-term (up to four weeks) dismissal of students during a Category 2 or Category 3 pandemic, and 3) prolonged (up to 12 weeks) dismissal of students from schools during a severe influenza pandemic (Category 4 or Category 5 pandemic).
In the most severe pandemic, the duration of these public health measures would likely be for 12 weeks, which would have educational implications for students. Planning now for a prolonged period of student dismissal may assist schools to be prepared as much as possible to provide opportunities for continued instruction and other assistance to students and staff. Federal, State, local, tribal, and territorial laws, regulations, and policies regarding student dismissal from schools, school closures, funding mechanisms, and educational requirements should be taken into account in pandemic planning. If students are dismissed from school but schools remain open, school- and education-related assets, including school buildings, school kitchens, school buses, and staff, may continue to remain operational and potentially be of value to the community in many other ways. In addition, faculty and staff may be able to continue to provide lessons and other services to students by television, radio, mail, Internet, telephone, or other media. Continued instruction is not only important for maintaining learning but also serves as a strategy to engage students in a constructive activity during the time that they are being asked to remain at home.
Planning now for a severe pandemic will ensure that schools are prepared to implement the community interventions that may be recommended. Be prepared to activate the school district’s crisis management plan for pandemic influenza that links the district’s incident command system with the local and/or State health department/emergency management system’s incident command system(s).
The Pandemic Flu Planning Checklist for K-12 School Districts describes approaches to school planning for a pandemic and can be found at www.pandemicflu.gov/plan/school/index.html and www.ed.gov/admins/lead/safety/emergencyplan/pandemic/planning-guide/index.html. Recommendations for implementation of pandemic mitigation strategies are available at www.pandemicflu.gov, and reliable, accurate, and timely information on the status and severity of a pandemic will also be posted on the Web site. Additional information is available from the Centers for Disease Control and Prevention (CDC) Hotline: 1-800-CDC-INFO (1-800-232-4636). This line is available in English and Spanish, 24 hours a day, 7 days a week. TTY: 1-888-232-6348. Questions can be e-mailed to cdcinfo@cdc.gov.
Recommendations for Planning
1. Plan for ill individuals to remain at home
- Develop a plan for faculty and staff absences due to personal illness. Plan for alternative staffing:
- Identify critical job functions and plan for alternate coverage of those functions during a pandemic.
- Review and analyze Federal and State employment laws that identify employer obligations and options for personnel.
- Establish and clearly communicate policies on sick leave and employee compensation.
- Encourage ill persons to stay home during a pandemic and establish return-to-work policies after illness.
- Establish policies for sick-leave absences unique to a pandemic (e.g., liberal/unscheduled leave).
- Develop policies on observation for illness and what to do when a student or staff member becomes ill at the workplace.
- Advise employees to look for information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov .
2. Plan for all household members of a person who is ill to voluntarily remain at home
- Develop a plan for faculty and staff absences related to family member illness. Plan for alternate staffing:
- Identify critical job functions and plan now for coverage of those functions.
- Establish policies for alternate or flexible worksite (e.g., videoconferencing and teleworking) and flexible work hours.
- Review Federal and State employment laws that identify your employer obligations and options for employees.
- Establish and clearly communicate policies on family leave and employee compensation.
- Establish policies for sick-leave absences unique to a pandemic (e.g., liberal/unscheduled leave).
- Establish policies for employees who have to stay home because someone in their household is ill with pandemic influenza.
- Be familiar with Federal and State laws regarding leave of workers who need to care for an ill family member or voluntarily remain at home.
- Advise employees to look for information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov.
3. Plan for dismissal of students and childcare closure for employees
- Develop a plan for school operations during all levels of pandemic severity. Even if students are dismissed, schools may remain operational.
- Identify and plan for employees and staff who may have to stay home if schools and childcare programs dismiss students/children during a pandemic.
- Plan for alternate staffing based on your assessment.
- Identify critical job functions and plan now for coverage of those functions in case of prolonged absenteeism during a pandemic.
- Establish policies for employees to possibly work flexible work hours and schedules (e.g., staggered shifts) to accommodate their childcare needs.
- Encourage your employees who have children to make their own plans to care for children if officials recommend dismissal of students from schools and closure of childcare programs. Advise that employees plan for an extended period (up to 12 weeks) in case the pandemic is severe. Instruct employees not to bring their children to the workplace if childcare cannot be arranged.
- In a severe pandemic, parents would be advised to protect their children by reducing out-of-school social contacts and mixing with other children. Although limiting all outside contact may not be feasible, families may be able to develop support systems with co-workers, friends, families, or neighbors if they continue to need childcare. For example, they could prepare a plan in which two to three families work together to supervise and provide care for a small group of infants and young children while their parents are at work (studies suggest that childcare group size of less than six children may be associated with fewer respiratory infections).2
- Determine if schools must, may, or cannot compensate, continue benefits, and extend leave to employees who are not working during the pandemic. Inform employees of the decision.
- Work with your State legislatures if modifications to State laws are needed for flexibilities regarding, for example, requirements for the number of instruction days, amount of instruction time, and length of the school day.
- Work with State and local governments and faith-based and community-based organizations to provide any needed assistance to staff who cannot report to work for a prolonged period.
4. Plan for dismissal of students
- Develop a plan for continuity of instruction
- Inform teachers, students and parents how alternate learning opportunities will be provided.
- This may include assignments by radio, television, regular mail, e-mail, telephone, and teleconferencing or through the media
- Consider potential restructuring of the school calendar
- Provide school nurses, counselors, school psychologists, special-needs teachers, and social workers guidance on maintaining needed health, counseling, and social services for students with physical and mental/emotional healthcare needs.
- Identify and inform parents on how students who need free meals may qualify for other types of nutrition assistance in the community.
- Provide systematic emergency communications to school staff and families during the pandemic, using a telephone calling tree, an e-mail alert, call-in voice recording, or regular mail to communicate.
5. Plan for workplace and community social distancing measures
- Become familiar with social distancing actions that may be used during a pandemic to modify frequency and type of person-to-person contact (e.g., reducing hand-shaking, limiting face-to-face meetings, promoting teleworking, liberal/unscheduled leave policies, and staggered shifts).
- Plan to operate the workplace using social distancing and other measures to minimize close contact between employees.
- Review and implement guidance from the Occupational Safety and Health Administration (OSHA) on appropriate work practices and precautions to protect employees from occupational exposure to influenza virus during a pandemic. Risks of occupational exposure to influenza virus depends in part on whether jobs require close proximity to people who may be infectious with the pandemic influenza virus or whether employees are required to have either repeated or extended contact with the general public. OSHA will post and periodically update such guidance on www.pandemicflu.gov.
- Encourage good hygiene at the workplace. Provide students, faculty, and staff with information about the importance of hand hygiene (information can be found at www.cdc.gov/cleanhands/) as well as convenient access to soap and water and alcohol-based hand gel in your facility. Educate employees and students about covering their cough to prevent the spread of germs (see www.cdc.gov/flu/protect/covercough.htm).
- Promote social distancing of children and teens outside the school setting by advising they reduce their social interaction and contacts to the greatest extent possible. This may include cancelling after-school and extracurricular group activities.
6. Communicate with faculty, staff, students, and parents/families
- Make sure your school’s pandemic plan is explained and understood by faculty, staff, and parents in advance of a pandemic, including expected roles/actions for employees and others during implementation.
- Provide information to school staff and parents/families on what they can do to prepare themselves and their families for the pandemic. Resources are available at www.pandemicflu.gov/plan/individual/checklist.html and www.ready.gov/america/index.html.
- Be prepared to provide parents/families with information discussing student dismissal from school and the importance of keeping students from congregating with other students in out-of-school settings.
- Provide staff with information on the school district’s plan for
- Assuring that essential central office functions, including payroll, and communications with staff, students, and families will continue.
- Adapting school facilities to supplement healthcare delivery if needed by local public health officials.
- Encouraging school nurses, counselors, school psychologists, and social workers to establish supportive long-distance relationships with particularly vulnerable students via the phone, e-mail, or regular mail.
- Coordinate strategies with other districts in your region.
7. Help your community
- Coordinate your pandemic plans and actions with local health and community planning.
- Find volunteers in your school who want to help people in need, such as elderly neighbors, single parents of small children, or people without the resources to get the medical or other help they will need.
- Think of ways your school can help others in your community plan for a pandemic.
- Participate in community-wide exercises to enhance pandemic preparedness.
8. Recovery
- Establish the criteria and procedure with State and local planning teams for resuming school activities.
- Develop communication for advising employees, students, and families of the resumption of school programs and activities.
- Develop the procedures, activities, and services needed to restore the learning environment.
References:
1 American Academy of Pediatrics. Children in Out-of-Home Child Care: Classification of Care Service. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003:124.
2 Bradley RH. Child care and common communicable illnesses in children aged 37 to 54 months. Arch Pediatr Adolesc Med. 2003 Feb;157(2):196-200.
Appendix 7 - Pandemic Influenza Community Mitigation Interim Planning Guide for Colleges and Universities
Purpose
This Interim Planning Guide for Colleges and Universities is provided as a supplement to the Interim Pre-Pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States—Early, Targeted, Layered Use of Nonpharmaceutical Interventions. The guide is intended to assist in pre-pandemic planning. Individuals and families, employers, schools, and other organizations will be asked to take certain steps (described below) to help limit the spread of a pandemic, mitigate disease and death, lessen the impact on the economy, and maintain societal functioning. This guidance is based upon the best available current data and will be updated as new information becomes available. During the planning process, Federal, State, local, tribal, and territorial officials should review the laws, regulations, and policies that relate to these recommendations, and they should include stakeholders in the planning process and resolution of issues.
Colleges and universities will be essential partners in protecting the public’s health and safety when an influenza pandemic occurs. This Pandemic Influenza Community Mitigation Interim Planning Guide for Colleges and Universities provides guidance to post-secondary institutions, describing how they should prepare for an influenza pandemic. At the onset of an influenza pandemic, public health officials will determine the severity of the pandemic and recommend actions to protect the community’s health. People who become severely ill may need to be cared for in a hospital. However, most people with influenza will be safely cared for at home.
Community mitigation recommendations will be based on the severity of the pandemic and may include the following:
- Asking ill people to voluntarily remain at home and not go to work or out in the community for about 7–10 days or until they are well and can no longer spread the infection to others (ill individuals will be treated with influenza antiviral medications, as appropriate, if these medications are effective and available).
- Asking members of households with a person who is ill to voluntarily remain at home for about 7 days (household members may be provided with antiviral medications, if these medications are effective and sufficient in quantity and feasible mechanisms for their distribution have been developed).
- Dismissing students from schools (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs for up to 12 weeks, coupled with protecting children and teenagers through social distancing in the community to include reductions of out-of-school social contacts and community mixing. Childcare programs discussed in this guidance include centers or facilities that provide care to any number of children in a nonresidential setting, large family childcare homes that provide care for seven or more children in the home of the provider and small family childcare homes that provide care to six or fewer children in the home of the provider.1
- Recommending social distancing of adults in the community, which may include cancellation of large public gatherings; changing workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services; and ensuring work-leave policies to align incentives and facilitate adherence with the measures outlined above.
Recommendations for cancelling college and university classes will depend upon the severity of the pandemic. The current three-tiered planning approach includes 1) no dismissals in a Category 1 pandemic, 2) short-term (up to 4 weeks) dismissal from classes in a Category 2 or Category 3 pandemic, and 3) prolonged (up to 12 weeks) dismissal from classes in a severe influenza pandemic (Category 4 or Category 5).
Dismissing students for up to 12 weeks will have educational implications. Planning now for a prolonged period of student dismissal will help colleges and universities to plan for alternate ways to provide continued instruction and services for students and staff. Even if students are dismissed from classes, the college/university facility may remain open during a pandemic and may continue to provide services to students who must remain on campus and provide lessons and other services to off-campus students via Internet or other technologies. Some students, particularly international students, may not be able to rapidly relocate during a pandemic and may need to remain on campus for some period. They would continue to need essential services from the college/university during that time.
Continued instruction is not only important for maintaining learning but also serves as a strategy to reduce boredom and engage students in a constructive activity while group classes are cancelled. Planning now for a severe pandemic will help assure that your college or university is prepared to implement these community recommendations. These preparedness efforts will be beneficial to your school, staff, students, and the community, regardless of the severity of the pandemic. Be prepared to activate the university’s crisis management plan for pandemic influenza, which links the university’s incident command system with the local and/or State health department/emergency management system’s incident command system(s).
The Pandemic Flu Planning Checklist for Colleges and Universities describes approaches to school planning for a pandemic and can be found at www.pandemicflu.gov/plan/school/index.html and www.ed.gov/admins/lead/safety/emergencyplan/pandemic/planning-guide/index.html. Recommendations for implementation of pandemic mitigation strategies are available at www.pandemicflu.gov and reliable, accurate, and timely information on the status and severity of a pandemic will also be posted on this site. Additional information is available from the Centers for Disease Control and Prevention (CDC) Hotline: 1-800-CDC-INFO (1-800-232-4636). This line is available in English and Spanish, 24 hours a day, 7 days a week. TTY: 1-888-232-6348. Questions can be e-mailed to cdcinfo@cdc.gov.
Recommendations for Planning
1. Plan for ill individuals to remain at home
- Develop a plan for faculty and staff absences due to personal illness. Plan for alternative staffing.
- Identify critical job functions and plan for alternate coverage of those functions during a pandemic.
- Review and analyze Federal and State employment laws that identify employer obligations and options for personnel.
- Establish and clearly communicate policies on sick leave and employee compensation.
- Encourage ill persons to stay home during a pandemic and establish return-to-work policies after illness.
- Establish policies for sick-leave absences unique to a pandemic (e.g., liberal/unscheduled leave).
- Develop policies on observation for illness and what to do when a student or staff member becomes ill at the college/university.
- Advise employees to look for information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov.
2. Plan for all household members of a person who is ill to voluntarily remain at home
- Develop a plan for faculty and staff absences related to family member illness. Plan for alternate staffing.
- Identify critical job functions and plan now for coverage of those functions.
- Establish policies for alternate or flexible worksite (e.g., videoconferencing and teleworking) and flexible work hours.
- Review Federal and State employment laws that identify your employer obligations and options for employees.
- Establish and clearly communicate policies on family leave and employee compensation.
- Establish policies for sick-leave absences unique to a pandemic (e.g., liberal/unscheduled leave).
- Establish policies for employees who have to stay home because someone in their household is ill with pandemic influenza.
- Be familiar with Federal and State laws regarding leave of workers who need to care for an ill family member or voluntarily remain at home.
- Advise employees to look for information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov.
3. Plan for dismissal of students and childcare closure for employees
- Identify and plan for employees and staff who may have to stay home if schools and childcare programs dismiss students/children during a severe pandemic.
- Plan for alternate staffing based on your assessment.
- Identify critical job functions and plan for coverage of those functions in case of prolonged absenteeism during a pandemic.
- Establish flexible work policies for employees, such as flexible work hours and schedules (e.g., staggered shifts) to accommodate childcare needs.
- Encourage your employees who have children to make their own plans to care for children if officials recommend dismissal of students from schools and closure of childcare programs. Advise that employees plan for an extended period (up to 12 weeks) in case the pandemic is severe. Instruct employees not to bring their children to the workplace if childcare cannot be arranged.
- In a severe pandemic, parents will be advised to protect their children by reducing out-of-school social contacts and mixing with other children. Although limiting all outside contact may not be feasible, families may be able to develop support systems with co-workers, friends, families, or neighbors, if they continue to need childcare. For example, they could prepare a plan in which two to three families work together to supervise and provide care for a small group of infants and young children while their parents are at work (studies suggest that childcare group size of less than six children may be associated with fewer respiratory infections).2
- Determine if schools must, may, or cannot compensate, continue benefits to and extend leave to employees who are not working during the pandemic. Inform employees of the decision.
- Coordinate with State and local government and faith-based and community-based organizations to provide any needed assistance to staff that are not able to work for a prolonged period (including matching available workers with local businesses, government agencies, or non-profit organizations needing extra workers).
4. Plan for dismissal of students
- Inform students about plans and procedures for providing and completing course work.
- Provide guidance to students and faculty on continuing student instruction. Such guidance may include
- Assessing the possibility of altering course-work requirements.
- Providing ongoing assignments by regular mail, e-mail, Internet links, telephone, teleconferencing, or calling into a recorded message at the university
- Gathering information in advance that would identify students’ mailing addresses, telephone/cell numbers, and e-mail addresses
- Encouraging faculty who teach the same subject to share in the development of distance-learning instructional materials for their students.
- Providing information on accessing university healthcare staff (e.g., nurses, nurse practitioners, physicians, physician assistants, counselors, and psychologists) who could be recommended as consultation resources for students with physical and mental/emotional healthcare needs.
- Develop a plan for accommodating students, especially international students, who remain on campus during an influenza pandemic.
- Review and implement guidance from the Occupational Safety and Health Administration (OSHA) on appropriate work practices and precautions to protect employees from occupational exposure to influenza virus during a pandemic. Risks of occupational exposure to influenza virus depends in part on whether or not jobs require close proximity to people who may be infectious with the pandemic influenza virus or whether employees are required to have either repeated or extended contact with the public. OSHA will post and periodically update such guidance on www.pandemicflu.gov.
5. Plan for workplace and community social distancing measures
- Learn about social distancing methods that may be used during a pandemic to limit person-to-person contact during a pandemic and reduce the spread of disease (e.g., reducing hand-shaking, limiting face-to-face meetings and shared workstations, work from home policies, staggered shifts).
- Use social distancing measures to minimize close contact at your college/university. Determine how your facility could be rearranged to allow more distance between people during a pandemic.
- Develop plans for alternatives to mass gatherings. Examples could range, for example, from video messages on the Internet to e-mailed messages, mailed newsletters, pre-recorded messages on a designated call-in phone number.
- Encourage good hygiene at the workplace. Provide faculty, staff, and students with information about the importance of hand hygiene (information can be found at www.cdc.gov/cleanhands/) as well as convenient access to soap and water and alcohol-based hand gel in your facility. Educate faculty, staff, and students about covering their cough to prevent the spread of germs (see www.cdc.gov/flu/protect/covercough.htm).
6. Communicate with faculty, staff, students, and parents/families
- Provide faculty, staff, and parents with information on the college/university’s pandemic preparedness plan in advance of a pandemic. This communication should include
- Identifying expected roles/actions for faculty, staff, students, and other stakeholders during implementation
- Assuring that essential central office functions, including payroll, and communications with staff, students and families will continue
- Identifying how the college/university’s physical facilities may be used for other purposes during a pandemic
- Develop a plan to inform parents/families that students may be dismissed during a Category 4-5 pandemic.
- Encourage them to plan for that contingency, including plans for relocating students to home or elsewhere
- Inform them of school procedures and policies regarding tuition, fees, and contractual obligations
- Provide systematic emergency communications to faculty, staff, and students (both on and off campus) during the pandemic by using multiple methods (e.g., a telephone calling tree, an e-mail alert, or call-in voice recording) to communicate pandemic status in the community and status of classes and other university activities.
- Be prepared to provide parents/families with information discussing
- How dismissal of students will be announced
- Why students will be dismissed from classes and the importance of keeping students from congregating with others in the community
- How alternate instruction will be provided
- Be prepared to provide students who soon will be leaving for home with information discussing
- Why students are being dismissed from classes and the importance of keeping students from congregating with other students in the community. Students should understand
- Differences between seasonal and pandemic influenza
- How influenza is spread
- What individuals can do help prevent the spread of influenza
- Remind students who live in residence halls to take their books and other personal items with them on the last day of classes, if indicated.
- Provide information to university faculty, staff, and parents/families on what they can do to prepare their families for the pandemic. Resources are available at www.pandemicflu.gov/plan/individual/checklist.html and www.ready.gov/america/index.html.
- Recommend that faculty, staff, students and their families seek further information about the pandemic through resources, including key Federal, State, and local public health that provide regular updates on the status of the pandemic. For reliable, accurate, and timely information about pandemic flu, see www.pandemicflu.gov.
7. Help your community
- Coordinate your pandemic plans and actions with local health planning.
- Find volunteers in your college/university who want to help people in need, such as elderly neighbors, single parents of small children, or people without the resources to get the medical or other help they will need.
- Think of ways your institution can reach out to others in your community to help them plan for a pandemic.
- Participate in community-wide exercises to enhance pandemic preparedness.
8. Recovery
- Establish with State and local planning teams the criteria and procedures for resuming school activities.
- Develop communication for advising employees and students and families of the resumption of school programs and activities.
- Develop the procedures, activities, and services needed to restore the learning environment.
References:
1 American Academy of Pediatrics. Children in Out-of-Home Child Care: Classification of Care Service. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003:124.
2 Bradley RH. Child care and common communicable illnesses in children aged 37 to 54 months. Arch Pediatr Adolesc Med. 2003 Feb;157(2):196-200.
Appendix 8 - Pandemic Influenza Community Mitigation Interim Planning Guide for Faith-Based and Community Organizations
Purpose
This Interim Planning Guide for Faith-based and Community Organizations is provided as a supplement to the Interim Pre-Pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States—Early, Targeted, Layered Use of Nonpharmaceutical Interventions. The guide is intended to assist in pre-pandemic planning. Individuals and families, employers, schools, and faith-based and community organizations will be asked to take certain steps (described below) to help limit the spread of a pandemic, mitigate disease and death, lessen the impact on the economy, and maintain societal functioning. This guidance is based upon the best available current data and will be updated as new information becomes available. During the planning process, Federal, State, local, tribal, and territorial officials should review the laws, regulations, and policies that relate to these recommendations, and they should include stakeholders in the planning process and resolution of issues.
Faith-based and community organizations (FBCOs) will be essential partners in protecting the public’s health and safety when an influenza pandemic occurs. This Pandemic Influenza Community Mitigation Interim Planning Guide for Faith-Based and Community Organizations provides guidance for religious organizations (including, for example, places of worship—churches, synagogues, mosques, and temples—and faith-based social service providers), social service agencies, and community organizations in preparing for and responding to an influenza pandemic. When an influenza pandemic starts, public health officials will determine the severity of the pandemic and recommend actions to protect the community’s health. People who become severely ill may need to be cared for in a hospital. However, most people with influenza will be safely cared for at home.
Community mitigation recommendations will be based on the severity of the pandemic and may include the following:
- Asking ill people to voluntarily remain at home and not go to work or out in the community for about 7-10 days or until they are well and can no longer spread the infection to others (ill individuals will be treated with influenza antiviral medications, as appropriate, if these medications are effective and available).
- Asking members of households with a person who is ill to voluntarily remain at home for about 7 days (household members may be provided with antiviral medications, if these medications are effective and sufficient in quantity and feasible mechanisms for their distribution have been developed).
- Dismissing students from schools (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs for up to 12 weeks, coupled with protecting children and teenagers through social distancing in the community to include reductions of out-of-school social contacts and community mixing. Childcare programs discussed in this guidance include centers or facilities that provide care to any number of children in a nonresidential setting, large family childcare homes that provide care for seven or more children in the home of the provider and small family childcare homes that provide care to six or fewer children in the home of the provider.1
- Recommending social distancing of adults in the community, which may include cancellation of large public gatherings; changing workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services; and ensuring work-leave policies to align incentives and facilitate adherence with the measures outlined above.
Planning now for a severe pandemic will help assure that your organization is prepared to implement these community recommendations. These preparedness efforts will be beneficial to your organization, volunteer and paid staff, and community, regardless of the severity of the pandemic. The Faith-Based & Community Organizations Pandemic Influenza Preparedness Checklist (available at
www.pandemicflu.gov/plan/community/faithcomchecklist.html) provides an approach to pandemic planning by FBCOs. In addition, recommendations for implementation of pandemic mitigation strategies are available at www.pandemicflu.gov. Reliable, accurate, and timely information on the status and severity of the pandemic also will be posted on www.pandemicflu.gov. Additional information is available from the Centers for Disease Control and Prevention (CDC) Hotline: 1-800-CDC-INFO (1-800-232-4636). This line is available in English and Spanish, 24 hours a day, 7 days a week. TTY: 1-888-232-6348. Questions can be e-mailed to cdcinfo@cdc.gov.
Recommendations for Planning
1. Plan for ill individuals to remain at home
- Plan for employee and volunteer staff absences during a pandemic due to personal illness.
- Identify critical job functions and plan how to temporarily suspend non-critical activities, cross-train staff to cover critical functions, and cover the most critical functions with fewer staff.
- Identify employees, volunteers, and members or clients that live alone or might need extra assistance if they need to stay home because they are ill.
- Review Federal and State employment laws that identify your employer obligations and options for employees.
- Establish and clearly communicate policies on sick leave and employee compensation.
- Encourage ill persons to stay home during a pandemic and establish return to work policies after illness.
- Encourage leadership to model staying at home when ill as well as the use of proper cough and sneeze etiquette and hand hygiene.
- Where appropriate, align public health messages and recommendations with your organization’s values and beliefs. For example, develop a culture that recognizes the positive behaviors of voluntarily staying home when ill to get well and avoid spreading infection to others.
- Develop policies on what to do when a person becomes ill at the workplace.
- Advise employees, volunteers, and members or clients to look for information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov.
2. Plan for all household members of a person who is ill to voluntarily remain at home
- Plan for employee and volunteer staff absences during a pandemic related to family member illness.
- Identify critical job functions and plan how to temporarily suspend non-critical activities, cross-train staff to cover critical functions, and cover the most critical functions with fewer staff.
- Establish policies for alternate or flexible worksite (e.g., work via the Internet, e-mail, mailed or phone work assignments) and flexible work hours.
- Establish and clearly communicate policies on family leave and employee compensation, especially Federal laws and laws in your State regarding leave of workers who need to care for an ill family member or voluntarily remain at home.
- Establish and clearly communicate policies for volunteers to ensure that critical functions are covered.
- Advise staff and members to look for information on taking care of ill people at home. Such information will be posted on www.pandemicflu.gov.
3. Plan for dismissal of students and childcare closure
- Find out how many employee and volunteer staff may have to stay at home to care for children if schools and childcare programs dismiss students.
- Identify critical job functions and plan for temporarily suspending non-critical activities and cross-training staff to cover critical functions with fewer staff.
- Establish policies for staff with children to work from home, if possible, and consider flexible work hours and schedules (e.g., staggered shifts).
- Encourage staff with children to make plans for what they will do if officials recommend dismissal of students from schools and closure of childcare programs. Instruct staff and volunteers not to bring their children to the workplace if childcare cannot be arranged.
- In a severe pandemic, parents will be advised to protect their children by reducing out-of-school social contacts and mixing with other children. Although limiting all outside contact may not be feasible, parents may be able to develop support systems with co-workers, friends, families, or neighbors, if they continue to need childcare. For example, they could prepare a plan in which two to three families work together to supervise and provide care for a small group of infants and young children while their parents are at work (studies suggest that childcare group size of less than six children may be associated with fewer respiratory infections).2
- Help your staff explore about benefits they may be eligible for if they have to stay home to mind children for a prolonged period during a pandemic.
4. Prepare your organization
- Consider potential financial deficits due to emergencies when planning budgets. This is useful for pandemic planning and many other unforeseen emergencies, such as fires and natural disasters.
- Many FBCOs rely on community-giving to support their activities. Develop strategies that will allow people to continue to make donations and contributions via the postal service, the Internet, or other means if they are at home for an extended period.
- Develop a way to communicate with your employee and volunteer staff during an emergency to provide information and updates.
- Meet with other FBCOs to develop collaborative efforts to keep your organizations running, such as large organizations collaborating with small ones or several small organizations working together.
5. Plan for workplace and community social distancing measures
- Learn about social distancing methods that may be used during a pandemic to limit person-to-person contact during a pandemic and reduce the spread of disease (e.g., reducing hand-shaking, limiting face-to-face meetings and shared workstations, work from home policies, staggered shifts).
- Use social distancing measures to minimize close contact at your facility. Determine how your facility could be rearranged to allow more distance between people during a pandemic.
- Develop plans for alternatives to mass gatherings. Examples could range from video messages on the Internet to e-mailed messages, mailed newsletters, pre-recorded messages from trusted leaders on a designated call-in phone number, and daily teaching guides from trusted leaders.
- Encourage good hygiene at the workplace. Provide staff, volunteers, and members with information about the importance of hand hygiene (information can be found at www.cdc.gov/cleanhands/) as well as convenient access to soap and water and alcohol-based hand gel in your facility. Educate employees about covering their cough to prevent the spread of germs (see www.cdc.gov/flu/protect/covercough.htm).
- Identify activities, rituals, and traditions, such as hand shaking, hugging, and other close-proximity forms of greeting that may need to be temporarily suspended or modified during a pandemic.
- Review and implement guidance from the Occupational Safety and Health Administration (OSHA) to adopt appropriate work practices and precautions to protect employees from occupational exposure to influenza virus during a pandemic. Risks of occupational exposure to influenza virus depends in part on whether or not jobs require close proximity to people potentially infected with the pandemic influenza virus or whether they are required to have either repeated or extended contact with the general public. OSHA will post and periodically update such guidance on www.pandemicflu.gov.
6. Communicate with your employee and volunteer staff and members
- Share your organization’s pandemic plan, including expected roles/actions for employee and volunteer staff and members during implementation.
- Suggest that all employee, volunteers, and members or clients prepare for a pandemic. Resources are available at www.pandemicflu.gov/plan/individual/checklist.html and www.ready.gov/america/index.html. For example, individuals and families should have a reserve supply of food and water. People with more resources might consider obtaining enough supplies to support 1-2 other families in an emergency.
- Ensure that your organization has up-to-date contact information for employees, volunteers, and members or clients, including names of family members, addresses, home, work, and cell phone numbers, e-mail addresses, and emergency contacts.
7. Help your Community
- Identify people who are vulnerable and may need assistance in your community (i.e., elderly people who live alone, persons with disabilities, people with limited skill in speaking English, low-income families, children, or teens who may lack supervision). Designate people from your organization to be responsible to check on specific vulnerable people or families.
- Determine ways your facility might be used during a pandemic, such as a temporary care facility or a central distribution site for providing meals, supplies, or medicine to those who cannot obtain them.
- Identify and meet with local emergency responders, health departments, and healthcare organizations to learn about their planning and educate them about your organization’s planning.
- Suggest that each household maintain a current list of emergency contacts in your community.
- Meet with other FBCOs to develop collaborative efforts to care for those in need, such as large organizations partnering with small ones or several small organizations working together.
- Identify employee and volunteer staff in advance who would be willing to help others in need during a pandemic and help them to receive training through the local health department, emergency services, or other resources.
- Designate an experienced person who can take calls and organize individuals who call spontaneously to volunteer during an emergency to facilitate the best use of their particular skills and experience.
- Develop or identify an existing mental health or counseling hotline that people in the community can call during a pandemic or other emergency.
- Participate in community-wide exercises to enhance pandemic preparedness.
8. Recovery
- Assess which criteria would need to be met to resume normal operations.
- Plan for the continued need for medical, mental health, and social services after a pandemic.
References:
1 American Academy of Pediatrics. Children in Out-of-Home Child Care: Classification of Care Service. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003:124.
2 Bradley RH. Child care and common communicable illnesses in children aged 37 to 54 months. Arch Pediatr Adolesc Med. 2003 Feb;157(2):196-200.
Appendix 9 - Pandemic Influenza Community Mitigation Interim Planning Guide for Individuals and Families
Purpose
This Interim Planning Guide for Individuals and Families is provided as a supplement to the Interim Pre-Pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States—Early, Targeted, Layered Use of Nonpharmaceutical Interventions. The guide is intended to assist in pre-pandemic planning. Individuals and families, employers, schools, and other organizations will be asked to take certain steps (described below) to help limit the spread of a pandemic, mitigate disease and death, lessen the impact on the economy, and maintain societal functioning. This guidance is based upon the best available current data and will be updated as new information becomes available. During the planning process, Federal, State, local, tribal, and territorial officials should review the laws, regulations, and policies that relate to these recommendations, and they should include stakeholders in the planning process and resolution of issues.
Individuals and families will have an essential role in protecting themselves and the public’s health and safety when an influenza pandemic occurs. This Pandemic Influenza Community Mitigation Interim Planning Guide for Individuals and Families provides guidance describing how individuals and families might prepare for and respond to an influenza pandemic. At the onset of an influenza pandemic, public health officials will determine the severity of the pandemic and recommend actions to protect the community’s health. People who become severely ill may need to be cared for in a hospital. However, most people with influenza will be safely cared for at home.
Community mitigation recommendations will be based on the severity of the pandemic and may include the following:
- Asking ill people to voluntarily remain at home and not go to work or out in the community for about 7-10 days or until they are well and can no longer spread the infection to others (ill individuals will be treated with influenza antiviral medications, as appropriate, if these medications are effective and available).
- Asking members of households with a person who is ill to voluntarily remain at home for about 7 days (household members may be provided with antiviral medications, if these medications are effective and sufficient in quantity and feasible mechanisms for their distribution have been developed).
- Dismissing students from schools (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs for up to 12 weeks, coupled with protecting children and teenagers through social distancing in the community to include reductions of out-of-school social contacts and community mixing. Childcare programs discussed in this guidance include centers or facilities that provide care to any number of children in a nonresidential setting, large family childcare homes that provide care for seven or more children in the home of the provider, and small family childcare homes that provide care to six or fewer children in the home of the provider.1
- Recommending social distancing of adults in the community, which may include cancellation of large public gatherings; changing workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services; and ensuring work-leave policies to align incentives and facilitate adherence with the measures outlined above.
Planning now for a severe pandemic will assist you and your family as you prepare for interventions that might be recommended. Resources are available at www.pandemicflu.gov/plan/individual/checklist.html and www.ready.gov/america/index.html. In addition, reliable, accurate, and timely information on the status and severity of a pandemic and recommendations for implementation of pandemic mitigation strategies is available at www.pandemicflu.gov. Additional information is available from the Centers for Disease Control and Prevention (CDC) Hotline: 1-800-CDC-INFO (1-800-232-4636). This line is available in English and Spanish, 24 hours a day, 7 days a week. TTY: 1-888-232-6348. Questions can be e-mailed to cdcinfo@cdc.gov.
Recommendations for Planning
1. Plan for ill individuals to remain at home
- Be prepared to stay at home if you are ill with pandemic influenza. Information on taking care of ill people at home will be posted on www.pandemicflu.gov.
- It will be important to have extra supplies on hand during a pandemic, as you may not be able to get to a store or stores may be out of supplies. You should have a reserve of at least a two-week supply of water and food; however, if the pandemic is severe, community disruption may last for a longer period. If community water supplies are not suitable for consumption during a pandemic, your local water utility or public health authorities will notify the community.
- Periodically check your regular prescription drugs to ensure a continuous supply in your home.
- Have any nonprescription drugs and other health supplies on hand, including a thermometer, pain relievers, stomach remedies, cough and cold medicines, and other over-the-counter medicines that you and your family use on a regular basis.
- Designate one person in the household who could be the caregiver if anyone in the household becomes ill with pandemic influenza. Develop an alternate plan for someone to be the caregiver if that person becomes sick.
- Talk with neighbors, friends, and family about your plans for staying at home if you or someone in your household is ill. Share ideas.
- Ensure that each household has a current list of emergency contacts in your community, including mental health and counseling resources.
2. Plan for all household members of a person who is ill to voluntarily remain at home
- Be prepared to stay at home if someone in your household is ill. Information on taking care of ill people at home will be posted on www.pandemicflu.gov.
- Have any nonprescription drugs and other health supplies on hand, including a thermometer, pain relievers, stomach remedies, cough and cold medicines, and other over-the-counter medicines that you and your family use on a regular basis.
- Talk with family members and members of your household about how they would be cared for if they become ill and about what will be needed to care for them in your or their home.
- Designate one person in the household who could be the caregiver if anyone in the household becomes ill with pandemic flu. Make plans for a backup if that person gets ill.
- Consider how to care for people in your household with special needs in case the services they rely on are not available.
- Talk with neighbors, friends, and family about your plans for staying at home if someone in your household is ill. Share ideas.
- Ensure that each household has a current list of emergency contacts in your community, including mental health and counseling resources.
3. Plan for dismissal of students and childcare closure
- If you have children in your household, make plans for their care if officials recommend dismissal of students from schools and closure of childcare programs.
- Plan and arrange now for who will care for children if schools and childcare programs dismiss students and children during a pandemic. Plan for an extended period (up to 12 weeks) in case the pandemic is severe.
- Do not plan to bring children to the workplace if childcare cannot be arranged.
- If you have children in a college or university, have a plan for the student to relocate or return home, if desired, or if the college/university dismisses students, at the onset of a Category 4-5 pandemic.
- Plan home-learning activities and exercises. Have materials, such as books, on hand.
- Public health officials will likely recommend that children and teenagers do not gather in groups in the community during a pandemic. Plan recreational activities that your children can do at home.
- Find out now about the plans at your child’s school or childcare facility during a pandemic.
- In a severe pandemic, parents will be advised to protect their children by reducing out-of-school social contacts and mixing with other children. Although limiting all outside contact may not be feasible, parents may be able to develop support systems with co-workers, friends, families, or neighbors, if they continue to need childcare. For example, they could prepare a plan in which two to three families work together to supervise and provide care for a small group of infants and young children while their parents are at work (studies suggest that childcare group size of less than six children may be associated with fewer respiratory infections).2
4. Plan for workplace and community social distancing measures
- Become familiar with social distancing actions that may be used during a pandemic to modify frequency and type of person-to-person contact (e.g., reducing hand-shaking, limiting face-to-face meetings, promoting teleworking, liberal/unscheduled leave policies, and staggered shifts).
- Talk to your employer
- Talk to your employer about the pandemic influenza plan for your workplace to include issues about benefits, leave, telework, and other possible policies to go into effect during a pandemic.
- Ask your employer about how your employer will continue during a pandemic if key staff cannot come to work.
- Plan for the possible reduction or loss of income if you are unable to work or your place of employment is closed. Consider maintaining a cash reserve.
- Check with your employer or union about leave policies for workers who are ill, live in a household with someone ill with pandemic influenza, or have to take off work to take care of children.
- Find out if you can work from home.
- Discuss alternative ways of holding meetings at work, including, for example, teleconferences, during a pandemic.
- Find out how you will receive information from your employer during a pandemic.
- Prepare backup plans in case public gatherings, such as community events and meetings and worship services, are cancelled.
- Talk with others in your community about other ways of communicating during a pandemic if public gatherings are cancelled.
- Plan for recreational activities that you and your household members can do at home if community gatherings are cancelled during a pandemic.
- Discuss with your faith-based organization or place of worship their plans for communicating with members during a pandemic.
5. Help others
- Prepare backup plans for taking care of loved ones who are far away.
- Find volunteers who want to help people in need, such as elderly neighbors, single parents of small children, or people without the resources to get the medical help they will need.
- Think of ways you can reach out to others in your neighborhood or community to help them plan for and respond to a pandemic.
References:
1 American Academy of Pediatrics. Children in Out-of-Home Child Care: Classification of Care Service. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003:124.
2 Bradley RH. Child care and common communicable illnesses in children aged 37 to 54 months. Arch Pediatr Adolesc Med. 2003 Feb;157(2):196-200.