|
 |
 |
 |
      |
 |
What
is anthrax?
Anthrax is an acute infectious
disease caused by a spore-forming bacterium called Bacillus
anthracis. It is generally acquired following
contact with anthrax-infected animals or anthrax-contaminated
animal products. Anthrax has received heightened
attention recently because of its use as a biological
warfare agent.
|
|
 |
| What
is Bacillus anthracis? |
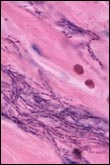
- Bacillus anthracis,
the etiologic agent of anthrax, is a
large, gram-positive, non-motile, spore-forming
bacterial rod. The three virulence factors
of Bacillus anthracis are
edema toxin, lethal toxin, and a capsular
antigen. Human anthrax has three major
clinical forms: cutaneous, inhalation,
and gastrointestinal.
- Bacillus anthracis spores
do not have a characteristic appearance
such as color, smell, or taste. Spores
themselves are too small to be seen by
the naked eye, but have been mixed with
powder to transport them.
|
|
 |
|
| How
can I be exposed to Bacillus
anthracis? |
- Anthrax infection can occur in three
forms:
- Cutaneous (skin)
- Inhalation
- Gastrointestinal
- Bacillus anthracis spores
can live in soil for many years. Humans
can become infected with anthrax by handling
products from infected animals or by
inhaling anthrax spores from contaminated
animal products.
|
|
 |
- Anthrax can also be spread by eating undercooked
meat from infected animals. It is rare to find
infected animals in the United States.
- Direct person-to-person spread of anthrax
is extremely unlikely to occur. Communicability
is not a concern in managing or visiting with
patients with inhalational anthrax.
|
| What
are the symptoms of anthrax? |
Symptoms of disease vary
depending on how the disease was contracted,
but symptoms usually occur within 7 days.
- Cutaneous: Most
(about 95 percent) anthrax infections occur
when the bacterium enters a cut or abrasion
on the skin, such as when handling contaminated
wool, hides, leather, or hair products (especially
goat hair) of infected animals. Skin infection
begins as a raised itchy bump that resembles
an insect bite but within 1-2 days develops
into a vesicle and then a painless ulcer, usually
1-3 centimeters in diameter, with a characteristic
black necrotic (dying) area in the center.
Lymph glands in the adjacent area may swell.
About 20 percent of untreated cases of cutaneous
anthrax will result in death. Deaths are rare
with appropriate antimicrobial therapy.
- Inhalation: Initial
symptoms may resemble a common cold. After
several days, the symptoms may progress to
severe breathing problems and shock. Inhalation
anthrax is often fatal.
- Intestinal: The
intestinal disease form of anthrax may follow
the consumption of contaminated meat and is
characterized by an acute inflammation of the
intestinal tract. Initial signs of nausea,
loss of appetite, vomiting, and fever are followed
by abdominal pain, vomiting of blood, and severe
diarrhea. Intestinal anthrax results in death
in 25 percent to 60 percent of cases. [Source: CDC
Anthrax FAQ]
|
| What
are the incidence rates
of anthrax? |
As of December 5, 2001,
a total of 22 cases of anthrax have been identified
in the United States -- 11 were confirmed as
inhalational anthrax and 11 (seven confirmed
and four suspected) were cutaneous. Of the 11
cases of inhalational anthrax, direct exposure
to Bacillus anthracis-containing
envelopes was confirmed or likely in the first
nine cases.
Before 2001, the incidence rates of anthrax were:
- From January 1955 to December 1999, there
were 236 reported cases of anthrax, most of
them cutaneous, in 30 states and the District
of Columbia.
- The last case of inhalational anthrax in
the United States, before 2001, was in 1976
in California. A home craftsman died of the
disease. He was exposed through his work with
yarn; Bacillus anthracis was
isolated from some of the imported yarns used
by the patient.
- The last case of cutaneous anthrax, before
2001, occurred in North Dakota, in 2000. It
was the only case since 1992.
The case fatality rates
for the various forms of anthrax are:
- Cutaneous: Early
treatment of cutaneous anthrax is usually curative,
and early treatment of all forms is important
for recovery. Patients with cutaneous anthrax
have reported case fatality rates of 20 percent
without antibiotic treatment and less than
1 percent with it.
- Inhalational: Although
case-fatality estimates for inhalational anthrax
are based on incomplete information, the rate
is extremely high, approximately 75 percent,
even with all possible supportive care including
appropriate antibiotics. Estimates of the impact
of the delay in post-exposure prophylaxis or
treatment on survival are not known.
- Gastrointestinal: For
gastrointestinal anthrax, the case-fatality
rate is estimated to be 25 percent to 60 percent.
The effect of early antibiotic treatment on
the case-fatality rate is not defined.
|
| How
is anthrax diagnosed and
treated? |
Diagnosis: Anthrax
is diagnosed by isolating Bacillus
anthracis from the blood, skin lesions,
or respiratory secretions or by measuring
specific antibodies in the blood of persons
with suspected cases.
Treatment: Doctors can prescribe effective
antibiotics. Bacillus
anthracis usually responds effectively
to several antibiotics including penicillin,
doxycycline, and fluoroquinolones (such as
ciprofloxacin). To be effective, treatment
should be initiated early. If left untreated,
the disease can be fatal. |
|
 |
Further information on antimicrobial
treatment of anthrax can be found on the following
websites:
|
| How
can I prevent infection? |
In countries
where anthrax is common and vaccination
levels of animal herds are low, humans
should avoid contact with livestock and
animal products and avoid eating meat that
has not been properly slaughtered and cooked.
Also, an anthrax vaccine has been licensed
for use in humans. The vaccine is reported
to be 93 percent effective in protecting
against anthrax.
The anthrax vaccine is a cell-free filtrate
vaccine, which means it contains no dead
or live bacteria in the preparation. The
final product contains no more than 2.4 milligrams
of aluminum hydroxide as an additive. Anthrax
vaccines intended for animals should not
be used in humans. |
|
 |
The Advisory
Committee on Immunization Practices has recommend
anthrax vaccination for the following groups:
- People who work directly with the organism
in the laboratory,
- People who work with imported animal hides
or furs in areas where standards are insufficient
to prevent exposure to anthrax spores,
- People who handle potentially infected animal
products in high-incidence areas (Incidence
is low in the United States, but veterinarians
who travel to work in other countries where
incidence is higher should consider being vaccinated.),
and
- Military personnel deployed to areas with
high risk for exposure to the organism (as
when it is used as a biological warfare weapon).
- First responders and workers involved in
anthrax decontamination.
Pregnant women should be
vaccinated only if absolutely necessary.
Further information on anthrax vaccination can
be found on the following websites:
|
| Links to
additional information on Bacillus
anthracis and anthrax |
|
|
|
|
| |
|
| | | | |
| | |
|
 |
 |
 |
|