 |
 |
 |
 |




|
Summary of Strategic Framework (TAB)Topics on this page
Making our vision of the future of healthcare a reality is a large undertaking. Our plan of action consists of four sequential main goals: informing clinicians, interconnecting them, personalizing care, and thus improving population health. Each goal is supported by three major strategies to help us achieve it.
Summary of Strategic Framework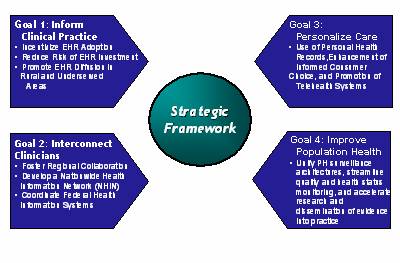
Goal 1 - Informing CliniciansUse of electronic health records (EHRs) can result in workflow efficiencies in clinicians' offices and higher quality of care for patients. Yet, only a fraction of all clinicians in the U.S use electronic health records today. Those who are using EHRs are considered pioneers among their peers. While EHR use has been slowly but steadily gaining acceptance among clinicians, many smaller practices maintain a strictly paper office. Introducing EHRs and other health information technology into a largely paper office changes current office workflows. Much of it is change for the better, but the transition requires substantial training for clinicians and their office employees as well as careful attention to explaining the rationale behind changes to physicians' practices.An increasing number of studies have found that EHRs can result in positive patient-care outcomes, but many physicians remain reluctant to embrace them. Accelerating the use of EHRs among clinicians requires that they are better informed about the benefits of incorporating greater technology into their practice and how it can benefit their patients. Before this can happen, several issues must be resolved. For many clinicians incorporating an EHR into their practice represents the unknown, signifies a costly alternative to present-day business practice, and signals a disruption of current workflow. Concerns over the cost of EHRs to clinicians remain a persistent and legitimate concern and thus a barrier to widespread adoption. In order to overcome this barrier, three things must happen. First, the investment in EHRs must be a shared one. Purchasing and deploying an EHR is a costly investment for a clinician's office, particularly a smaller practice. Therefore the cost must become an investment shared between clinicians and others in the health care system. This will allow many to not only play a role in making the transition possible but to profit as well, reducing the possibility that only certain players benefit from their purchase and use. We are exploring both financial and non-financial incentives for investors. Second, EHR certification is necessary. Using EHRs can result in reengineered business practices and workflow, but selecting the appropriate EHR can be challenging for clinicians. Certification of products from software vendors based on a minimum set of functions or capabilities will provide an initial level of assurance for physicians undertaking a production selection process. A private sector certification commission has been formed to address this. Technical assistance and support can further assist clinicians with EHR adoption to reduce risk of failure. Third, access to EHRs in rural and underserved areas must be increased. This could be even more challenging than achieving wider adoption among clinicians in populated areas or in larger practices. We are exploring options for greater penetration in these geographic areas. The best methods for data transportation and sharing by the Department of Veterans Affairs and Department of Defense are being reviewed to determine how these practices can be more widely adopted by clinicians in rural and underserved areas.
Goal 2 - Interconnecting CliniciansPatients' information should be portable and move with them from one point of care to another. The current practice of using separate paper files for one patient in multiple clinical settings is limiting and can compromise the quality of healthcare received. Conversion to an EHR system is necessary but not sufficient to solve the portability problem. That's because each clinician or medical practice may purchase an EHR system from different vendors, which may not be compatible with one another. Unless EHR systems can communicate, they are simply islands of data where patient information does not flow seamlessly from one clinical setting to the next. Without clinicians' ability to exchange information with one another electronically, whether it is across town or across the country, patients' information may not be readily available when and where it is needed. To remedy this, an interoperable system based upon a common architecture must be developed. Patient records would then be available electronically virtually anywhere in the country. We have outlined three strategies to achieve this.Our first step is to foster regional collaborations among health care entities so that a patient's information can be securely stored in the local community but is electronically accessible to those involved with providing their care in that community. A limited number of regional initiatives exist today, but they vary in the ways they approach data sharing and cannot communicate patient information outside their own system. As momentum builds and more regional collaboratives-coined "Regional Health Information Organizations" or RHIOs-are formed, a common approach for their development is needed to support the overall goal of health care data exchange among them. It is expected that the government could have a role in the formation of RHIOs. Second, these local RHIOs must be able to use a common set of standards so they can communicate with one another. Interconnecting each RHIO will require an infrastructure, known as a National Health Information Network (NHIN), to facilitate interoperability among RHIOs. This will allow medical information to travel anywhere with patients, thus revolutionizing the industry by making information more consumer-centric. HHS has proposed convening a private sector consortium to plan, develop, and operate the NHIN and has published a request for information (RFI) calling for outside input into the design and operation of the NHIN. Third, the government has made a commitment to using common standards and architecture to achieve a result similar to what is being planned for the private sector. The result will be a more cost-effective and efficient healthcare system.
Goal 3 - Personalizing HealthClinicians are not the only individuals who need greater access to patient information. Well-informed patients are better equipped to actively participate in their own care and decision-making. The Internet has proved invaluable in broadening access to information for consumers and patients, but general information from Websites goes only so far to educate people on wellness and illness. Innovations in technology are emerging to give patients electronic access to their health record and the ability to gather specific information tailored to their illnesses, chronic conditions and health characteristics. Widespread adoption of these innovations, via a concept known as a Personal Health Record (PHR), will revolutionize consumer health care decision-making. We are pursuing three strategies for personalizing health: encouraging the use of PHRs, enhancing informed consumer choice, and promoting the use of telehealth systems.The PHR is an electronic application through which individuals can maintain and manage their health information (and that of others for whom they are authorized) in a private, secure, and confidential environment. The PHR concept is gaining popularity but is hampered by the lack of a consistent framework for presenting information and by uncertainty as to how it should link up with the electronic health records of healthcare provider organizations, among other issues. More certain is the promise that a well-educated patient will emerge. For example, a PHR can be used to effectively synthesize an abundance of health information and tailor it to a patient's specific needs. The combination of selected data from their own medical records and additional patient-specific information will undoubtedly allow patients to make more informed healthcare choices. A nation of patients playing a more active role in their healthcare involves supplying them with information they find useful so they can make improved decisions. Those patient decisions should include not only what actions to take in their behalf but also whom they select to treat them and where they seek treatment. Consumers should be informed about the performance of clinicians and health care institutions based on unbiased measures of medical value and other considerations, including the quality of care delivered by a provider based on historical performance. Efforts to provide reliable and fair reports on performance have been limited by the scarcity of substantial and illuminating clinical information. Thus clinical performance is difficult to compare with any certainty, and the areas that happen to be measurable often are not very important in consumer choice. We support and will help facilitate efforts in the federal government and elsewhere to develop useful clinical performance measures in hospitals, nursing homes, home health agencies and other settings of care. Patients in rural and underserved areas confront many of the same barriers as providers when it comes to accessing health care information. Telehealth systems involve remote communication technology so that patients can receive care even when the clinician is not present. Telehealth has been proven both cost-effective and medically beneficial, but payment for services remains limited. More consideration should be given to providing sufficient provider reimbursement to encourage greater use. Telehealth systems could help treat patients who are not receiving the care they need due to distances involved in seeking treatment.
Goal 4 - Population HealthOur fourth and final goal is the most challenging and far-reaching but also the most important-improving the health of the entire nation. This task cannot be contemplated without timely and accurate information. But with a concerted and unified effort at all levels of government and private endeavor, a strong foundation for population health can be attained. To accomplish this ultimate goal, the federal government has proposed three primary strategies: unifying public health surveillance systems; streamlining quality and health status monitoring; and accelerating the pace at which scientific discoveries in medicine are disseminated into medical practice.Surveillance systems reduce the risk to public health from dangers such as communicable diseases, hazardous or unsafe foods, terrorism and other catastrophes. In such emergencies it is absolutely necessary to alert both clinicians and consumers quickly. By knitting together a unified network of surveillance systems from hospital organizations, physician practices, public health agencies and other sources of incoming data on medical threats, public health professionals will have the relevant information they need to react early or issue preventive measures. The only way to create such a network is to make all the data-collection systems interoperable. The healthcare field is at work creating standards for quality of patient care, but the efforts are not coordinated effectively. Many different organizations collect subsets of data for varying purposes and use them in different ways. Performance measures can focus either on the quality of care in a clinical setting-hospitals, nursing homes, home visits, etc.-or the many categories of disease conditions, such as heart problems, treatment of pneumonia, anti-infection measures and skill in maternal labor and delivery. Efforts are underway to develop standards that dictate how and under what conditions data should be collected. Streamlining and standardizing such quality-monitoring data will allow information on quality to be more completely aggregated and analyzed, providing a comprehensive picture of quality both at the point of care and for research purposes. Software applications to facilitate electronic tracking of quality indicators will help minimize burdens and intrusions on health professionals who are trying to focus on treating patients. Lastly, the government is working to accelerate the diffusion of clinical research information into the hands of sponsors, researchers and the Food and Drug Administration as well as the medical community at large. Research findings without adoption accomplish no public good; the discoveries must be translated into useful products and applications for physicians. Information technology is a vital component in delivering knowledge about new therapeutic agents and associated drugs and medical devices. IT systems also can speed up the submission of higher-quality research data to the FDA during clinical trials. Eventually an interoperable network of electronic health records would be able to accelerate translation of research into practice by tapping into national databases of clinical decision support and delivering the latest clinical knowledge to clinicians at the point of care. Complete Report – The Health IT Strategic FrameworkStrategic Framework: The Decade of Health Information Technology: Delivering Consumer-centric and Information-rich Health Care , 2004 [Download PDF Version - 10M]
List of Attachments |
Medical Identity Theft Town Hall Plans Underway; To learn more, visit ONC Commissioned Medical Identity Theft Assessment. The ONC-Coordinated Upcoming Events HL7 22nd Plenary and Working Group Meeting Personal Experiences "We have hospitals in Afghanistan and Iraq, and many of the soldiers would arrive without records in Germany, with no record of the CAT scans or what happened in surgery in Afghanistan or Iraq. The clinicians in Germany would have to re-operate on the patient, would have to redo all their x-ray evaluations, CAT scans, etc...." ~ Colonel John Holcomb Stay Informed Stay Informed! Join our Listserv for automatic updates |