Office of Medicare Hearings and Appeals (OMHA) Level 3 Appeals: Working with OMHAIf you disagree with the outcome of your Level 2 appeal (called a reconsideration in Parts A, B, and D, and a reconsidered determination in Part C), you or your representative can request a hearing before an OMHA Administrative Law Judge (ALJ). This is Level 3 of the claims appeal process. A hearing before an OMHA ALJ gives you the opportunity to present your appeal to a new person who will independently review the facts of your appeal and listen to your testimony before making a new and impartial decision in accordance with the applicable law.
The OMHA Appeals Process Steps in the Level 3 Appeals Process
Requirements for Making a Level 3 Appeal
How and Where to Request an Appeal
Before, During, and After the Hearing Process
When the ALJ Issues a Decision Favorable to You
Where and When the Hearing is Held
How and When You Will be Notified of Your Hearing Decision
Appealing the ALJ Decision
Preparing for your hearing Appointing a Representative
Video-teleconferencing (VTC)
Tips for Timely Review
The OMHA Appeals Process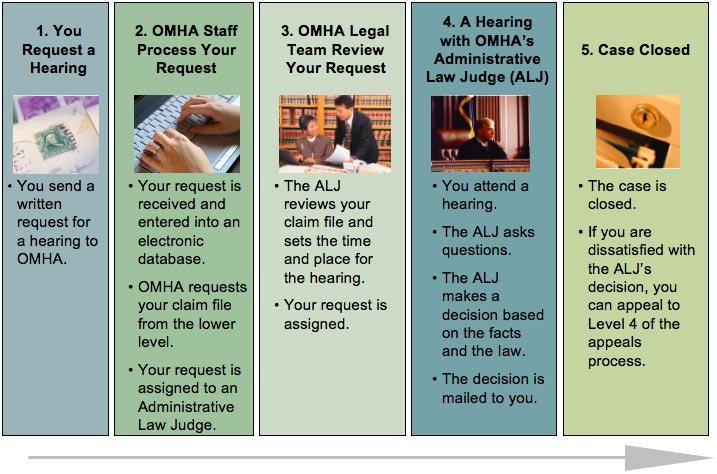 Graphic showing workflow of your hearing request at the third level of appeals. Back to top
In order to appeal your Level 2 appeal decision, you need to make sure you have done the following: - You must file a written request for a hearing within 60 days of receiving the level two appeals decision. If you miss the 60-day deadline, you must explain why your request is late and ask the ALJ to extend the deadline. If the ALJ finds good cause for missing the deadline, the time period for filing the hearing request will be extended.
- The claim(s) you are appealing must be valued at more than $120 (for 2008). This is called the "amount in controversy".
For further assistance, contact the OMHA field office that provides coverage in your state.
Back to top
Your request for an ALJ hearing must be in writing and contain the following information: - The beneficiary’s name, address and Medicare health insurance claim number;
- The name and address of the appellant, when the appellant is not the beneficiary;
- The name and address of the authorized representative if any;
- The document control number assigned by the QIC;
- The dates of service being appealed;
- The reasons you disagree with the QIC’s reconsideration or other determination being appealed, and
- A statement of any additional evidence to be submitted and the date it will be submitted. Note, if you are the provider/supplier, the authorized representative of the provider/supplier or the provider/supplier appealing on behalf of the beneficiary, your statement must also include an explanation why the evidence was not previously submitted to the QIC or a prior decision-maker.
Make sure that any evidence you want considered is submitted either with the Request for the ALJ hearing, or within 10 days of receiving the Notice of the ALJ hearing by either you or your representative. The ALJ will examine any new evidence submitted with the request for hearing (or within 10 days of receiving the notice of hearing) to determine whether the party had good cause for submitting the evidence for the first time at the ALJ level.
If any of the information described above is missing from your request for an ALJ hearing, it can cause delays in the processing of your appeal. At your option, the following forms may be used to file your written request for an ALJ hearing: - If you are appealing a Qualified Independent Contractor (QIC) decision: CMS-20034A/B; or
- If you are appealing a decision not made by a QIC: CMS-5011A/B.
Information on requesting an ALJ hearing is also included in your reconsideration notice. Send your written request to the OMHA Field Office listed in your reconsideration notice or reconsidered determination notice. If you send the request anywhere else, it can delay processing your request.
Back to top
When your request for an ALJ hearing is received by the OMHA field office, the staff establishes an electronic file to keep track of your case. The staff also sends a request to the QIC or other lower level decision-maker for them to forward your claim file to OMHA. An accurately completed request for ALJ hearing minimizes delays in obtaining your claim file. Before the hearing: - The ALJ reviews your claim file and sets the time and place for the hearing.
- You will receive a Notice of Hearing, at least 20 days before the scheduled hearing, notifying you of the time and place for the hearing and what issues will be decided.
- Once you receive the Notice of Hearing, complete the Response to Notice of Hearing Form and return it to the ALJ listed on the Notice of Hearing within 5 days of receipt of the Notice of Hearing.
- You and your representative may look at the evidence in your file. You do this by submitting a written request using the following forms:
- If you are requesting your own record: form HHS-719
- If you are a representative requesting the record with the beneficiary's permission: form HHS-720 (To give permission, submit form HHS-721)
- Under certain circumstances, you may be able to submit new evidence. It is very important that you submit any new evidence within 10 days of receiving the Notice of Hearing. To submit new evidence, you or your representative should fill out form HHS-728. The ALJ will examine any new evidence submitted with the request for hearing (or within 10 days of receiving the Notice of Hearing) to determine whether the party had good cause for submitting the evidence for the first time at the ALJ level.
At the hearing: - The ALJ will explain the issues in your case and may question you and any witnesses you bring to the hearing.
- The ALJ may ask other witness(es), such as a physician or other experts, to attend the hearing and provide testimony; you will have an opportunity to question any witness offering testimony at your hearing.
- You and the witness(es) will answer questions under oath.
- The ALJ makes an audio recording of the hearing.
After the hearing: - The ALJ issues a written decision after considering all the evidence and applicable law.
- The ALJ will mail to you and your representative, if you have one, a copy of the decision.
Back to top
If the ALJ finds in your favor and that your claim should be paid by Medicare, your case is forwarded to the CMS Medicare contractor for effectuation. This means it is the Medicare contractor and not the ALJ who is responsible to pay the claim according to the ALJ decision and applicable Medicare payment policies. Therefore, any questions you may have regarding Medicare payment following a favorable ALJ decision should be directed to the Medicare contractor and not OMHA. Back to top
The date, time, and location for your hearing will be sent to you at least twenty days before the hearing in the Notice of Hearing. A hearing will generally be held by video-teleconference. However, an in-person hearing may be held if the ALJ determines the circumstances of the appeal warrant an in-person hearing. Telephone hearings may also be arranged in certain circumstances. There are four field offices nationwide and hundreds of video-teleconference (VTC) sites where hearings may be held. This extensive network assists OMHA in providing you with ready access to hearings, even in remote locations. It also reduces the distance that you may need to travel for your hearing. If you are requesting an in-person hearing, your request must be in writing and also contain an explanation why the hearing needs to be conducted in-person rather than by video-teleconference or by telephone. The ALJ will consider your request and with the concurrence of the Managing ALJ, may grant it provided good cause is shown. If you cannot attend the hearing, notify the Administrative Law Judge (ALJ) assigned to your appeal as soon as possible. The ALJ will reschedule the hearing if you have good cause for not attending. Your request for a hearing can be dismissed if you fail to appear at the hearing and the ALJ determines that you did not have good cause. Most hearings are scheduled a few weeks ahead of time. Your hearing may take longer to schedule if the ALJ needs to schedule a medical or non-medical expert to testify.
Back to top
You will be notified of your hearing decision by U.S. mail. Generally you will receive the decision within 90 days of your hearing request, but keep in mind that each case is unique. Under certain circumstances the 90 day timeframe to decide your case may be extended. In some instances, if the ALJ does not issue a decision within the 90 day period, you may appeal directly to the Medicare Appeals Council (MAC).
Back to top
If you are not satisfied with the ALJ decision, you may request that the MAC review your case. This is a Level 4 appeal. Your request for the MAC to review your claim must be made within 60 days of the date you receive the OMHA ALJ hearing decision. If you are unable to meet this deadline, explain your reasons for missing it in your request. An appeal to the Medicare Appeals Council is referred to as a “request for review.” Note: A party does not have the right to seek MAC review of an ALJ's remand to a QIC or an ALJ's affirmation of a QIC's dismissal of a request for reconsideration. You should also know that other parties may file a request for review. To learn more about the MAC, see the section on the Level 4 appeals.
Back to top
Preparing for Your HearingAt every level of appeal, you are entitled to have a family member, friend, the provider/supplier or someone else represent you. Generally, in those cases, you and the representative must complete form CMS-1969-Appointment of Representative. However, a court-appointed guardian, an individual who has durable power of attorney, a health care proxy, or a person designated under a health care consent statute can file an appeal without an Appointment of Representative form, if you send to OMHA written proof of the representative's ability to represent you (for example, a valid power of attorney or an appointment order from a court).
Back to top
Office of Medicare Hearings and Appeals (OMHA) hearings often use video-teleconferencing technology or "VTC". The hearing utilizes video cameras and televisions so you and the ALJ can see and hear one another. The technology allows you to have a hearing without having to travel to an OMHA field office. Often a VTC hearing can be scheduled faster than an in-person hearing and that means less waiting time for you. Also, a VTC hearing location may be closer to your home and that might make it easier for you to have witnesses or other people accompany you. The VTC occurs in a private room and is completely confidential. A technician will make sure the equipment is working, but will not be present during the hearing and cannot hear your case. No one except your representative, or someone else you might choose, witnesses at the hearing, or others that the ALJ considers necessary and proper will be allowed to listen in or view the hearing. You will be able to see, hear and talk to the ALJ at the hearing. Transmission of the hearing is secure, and your privacy is protected. While all hearings are recorded, there is only audio recording and no video recording. If we are using VTC equipment in your area, we will contact you to schedule your VTC hearing for a convenient time. We realize that not everyone is familiar with how VTC works. The OMHA field office staff have a list of VTC sites near your home and can assist you in selecting a site. In addition, they can answer any questions you may have concerning VTC hearings. The ALJ will consider any concerns you may have expressed regarding your VTC hearing and the circumstances of the appeal when setting the time and place of your hearing. Once the time and place for your hearing are set, you will have an opportunity to object to either the time or place established for your hearing. Again, if you have any questions or want more information, please contact your OMHA field office.
Back to top
There are a number of things you can do to assist the processing of your request for a hearing. - Make sure your Request for Hearing is complete and accurate in order to minimize delays in obtaining your claim file from the QIC or prior decision-maker.
- If you wish to appoint a representative, do so as early as possible. Your representative will want time to review your file and prepare for the hearing. If you wait until the date of the hearing or shortly before, your hearing may have to be postponed to provide your representative with time to prepare. Rescheduling a hearing adds substantially to the time required to process your hearing request. It may also extend the 90 day adjudication deadline.
- Make sure that any evidence you want considered is submitted either with the Request for the ALJ hearing, or within 10 days of receiving the Notice of the ALJ hearing by either you or your representative. If you are the provider/supplier, the authorized representative of the provider/supplier or are the provider/supplier appealing on behalf of the beneficiary, you must also include an explanation why the evidence was not previously submitted to the QIC or a prior decision-maker. The ALJ will review the evidence and determine whether or not good cause exists for submitting the new evidence for the first time at the ALJ level.
- Notify us of any changes in your address immediately.
- OMHA requests that you do not make automatic, multiple requests for the status of your request for review.
Back to top
|