You are here:
Health Information
Related Information
- ¿Cómo se pueden prevenir las caídas y evitar posibles fracturas? (Esenciales: hojas informativas de fácil lectura)
- Order a NIAMS Publication to be mailed
Osteoporosis and Fracture
Reviewed August 2008
Preventing Falls and Related Fractures
Falls are serious at any age, and breaking a bone after a fall becomes more likely as a person ages. Many of us know someone who has fallen and broken or fractured a bone. While healing, the fracture limits the person's activities and sometimes requires surgery. Often, the person wears a heavy cast to support the broken bone and needs physical therapy to resume normal activities. People are often unaware that there is frequently a link between a broken bone and osteoporosis. A silent disease involving gradual loss of bone tissue or bone density and resulting in bones so fragile they break under the slightest strain, osteoporosis progresses without symptoms. Consequently, falls are especially dangerous for people who are unaware that their bone density is low. If the patient and the doctor fail to connect the broken bone to osteoporosis, the chance to make a diagnosis with a bone density test and begin a prevention or treatment program is lost. Bone loss continues, and other bones may break.
Even though bones do not break after every fall, the person who has fallen and broken a bone almost always becomes fearful of falling again. As a result, she or he may limit activities for the sake of "safety." Among Americans age 65 and older, fall-related injuries are the leading cause of accidental death.
This publication explores the components of the Fracture Triangle and offers tips for reducing the chances of fall-related fractures that result from low bone mass and osteoporosis. If one of the three factors below is modified, the chances of breaking a bone are greatly reduced:
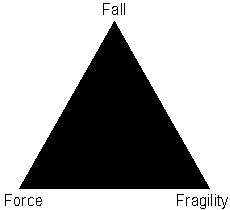
The Fall Itself
The Force and Direction of the Fall
The Fragility of the Bone(s) That Take the Impact
Did You Know?
- More than 90 percent of hip fractures are associated with osteoporosis.
- Nine out of 10 hip fractures in older Americans are the result of a fall.
- Individuals who have a hip fracture are 5 to 20 percent more likely to die in the first year following that injury than others in this age group.
- For those living independently before a hip fracture, 15 to 25 percent will still be in long-term care institutions a year after their fracture.
- Most falls happen to women in their homes in the afternoon.
The Fall Itself
There are several factors that can lead to a fall. Loss of footing or traction is a common cause of falls. Loss of footing occurs when there is less than total contact between the person's foot and the ground or floor. Loss of traction occurs when the ground upon which the person is stepping is wet or slippery, and the person's feet fly out from under her or him. Other examples of loss of traction include tripping, especially over uneven surfaces such as sidewalks, curbs, or floor elevations that result from carpeting, risers, or scatter rugs. Loss of footing also happens from using household items that were intended for other purposes - for example, climbing on kitchen chairs or balancing on boxes or books to increase height.
A fall may occur because a person's reflexes have changed. As people age, reflexes slow down. Reflexes are automatic responses to stimuli in the environment. Examples of reflexes include quickly slamming on the car brakes when a child runs into the street or quickly moving out of the way when something accidentally falls. Aging slows a person's reaction time and makes it harder to regain one's balance following a sudden movement or shift of body weight.
Improving Balance
- Do muscle-strengthening exercises.
- Obtain maximum vision correction.
- Practice using bifocal or trifocal glasses.
- Practice balance exercises daily.
Changes in muscle mass and body fat also can play a role in falls. As people get older, they lose muscle mass because they have become less active over time. Loss of muscle mass, especially in the legs, reduces a person's strength to the point where she or he is often unable to get up from a chair without assistance. In addition, as people age, they lose body fat that has cushioned and protected bony areas, such as the hips. This loss of cushioning also affects the soles of the feet, which upsets the person's ability to balance. The gradual loss of muscle strength, which is common in older people but not inevitable, also plays a role in falling. Muscle strengthening exercises, however, can help people regain their balance, level of activity, and alertness no matter what their age.
Changes in vision also increase the risk of falling. Diminished vision can be corrected with glasses. However, often these glasses are bifocal or trifocal so that when the person looks down through the lower half of her/his glasses, depth perception is altered. This makes it easy to lose one's balance and fall. To prevent this from happening, people who wear bifocals or trifocals must practice looking straight ahead and lowering their head. For many other older people, vision changes cannot be corrected completely, making even the home environment hazardous.
Medications That May Increase the Risk of Falling:
- Blood pressure pills
- Heart medicines
- Diuretics or water pills
- Muscle relaxers or tranquilizers
As people get older, they also are more likely to suffer from a variety of chronic medical conditions that often require taking several medications. People with chronic illnesses that affect their circulation, sensation, mobility, or mental alertness and those taking some types of medications (see chart) are more likely to fall as a result of drug-related side effects such as dizziness, confusion, disorientation, or slowed reflexes.
Drinking alcoholic beverages also increases the risk of falling. Alcohol slows reflexes and response time; causes dizziness, sleepiness, or lightheadedness; alters balance; and encourages risky behaviors that can lead to falls.
The Force and Direction of a Fall
The force of a fall (how hard a person lands) plays a major role in determining whether a person will fracture or not. For example, the greater the distance of the hip bone to the floor, the greater the risk of fracturing a hip, so tall people appear to have an increased risk of fractures when they fall. The angle at which a person falls also is important. For example, falling sideways or straight down is more risky than falling backward.
Did you know?
- Being tall appears to increase your risk of a hip fracture.
- How you land increases fracture risk.
- Catching yourself so you land on your hands or grabbing onto an object as you fall can prevent a hip fracture.
Protective responses, such as reflexes and changes in posture that break the fall, can reduce the risk of fracturing a bone. Individuals who land on their hands or grab an object on their descent are less likely to fracture their hip, but they may fracture their wrist or arm. While these fractures are painful and interfere with daily activities, they do not carry the high risks that a hip fracture does.
The type of surface on which one lands can also affect whether or not a bone breaks. Landing on a soft surface is less likely to cause a broken bone than landing on a hard surface.
Preliminary research has suggested that by wearing trochanteric (hip) padding, people can decrease the chances of fracturing a hip after a fall. The energy created by the fall is distributed throughout the pad, lessening the impact to the hip. Further research is needed to fully evaluate the role of these devices in decreasing the risk of a hip fracture following a fall.
Bone Fragility
While most serious falls happen when people are older, steps to prevent and/or treat bone loss and falls can never begin too early. Many people begin adulthood with less than optimal bone mass, so the fact that bone mass or density is lost slowly over time puts them at increased risk for fractures.
Bones that once were strong become so fragile and thin that they break easily. Activities that once were done without a second thought are now avoided for fear that they will lead to breaking another bone.
Steps to Prevent Fragile Bones:
- Consume adequate amounts of calcium and vitamin D (see chart).
- Exercise several times a week.
- Ask your doctor about a BMD (bone mineral density) test.
- Ask about medications to slow bone loss and reduce fracture risk.
Prevention of Falls and Fractures
Safety first to prevent falls: At any age, people can change their environments to reduce their risk of falling and breaking a bone.
-
Outdoor safety tips:
- In nasty weather, use a walker or cane for added stability.
- Wear warm boots with rubber soles for added traction.
- Look carefully at floor surfaces in public buildings. Many floors are made of highly polished marble or tile that can be very slippery. If floors have plastic or carpet runners in place, stay on them whenever possible.
- Identify community services that can provide assistance, such as 24-hour pharmacies and grocery stores that take orders over the phone and deliver. It is especially important to use these services in bad weather.
- Use a shoulder bag, fanny pack, or backpack to leave hands free.
- Stop at curbs and check their height before stepping up or down. Be cautious at curbs that have been cut away to allow access for bikes or wheelchairs. The incline up or down may lead to a fall.
Indoor safety tips:
- Keep all rooms free from clutter, especially the floors.
- Keep floor surfaces smooth but not slippery. When entering rooms, be aware of differences in floor levels and thresholds.
- Wear supportive, low-heeled shoes, even at home. Avoid walking around in socks, stockings, or floppy, backless slippers.
- Check that all carpets and area rugs have skid-proof backing or are tacked to the floor, including carpeting on stairs.
- Keep electrical cords and telephone lines out of walkways.
- Be sure that all stairwells are adequately lit and that stairs have handrails on both sides. Consider placing fluorescent tape on the edges of the top and bottom steps.
- For optimal safety, install grab bars on bathroom walls beside tubs, showers, and toilets. If you are unstable on your feet, consider using a plastic chair with a back and nonskid leg tips in the shower.
- Use a rubber bath mat in the shower or tub.
- Keep a flashlight with fresh batteries beside your bed.
- Add ceiling fixtures to rooms lit by lamps only, or install lamps that can be turned on by a switch near the entry point into the room. Another option is to install voice- or sound-activated lamps.
- Use bright bulbs in your home.
- If you must use a step-stool for hard-to-reach areas, use a sturdy one with a handrail and wide steps. A better option is to reorganize work and storage areas to minimize the need for stooping or excessive reaching.
- Consider purchasing a portable phone that you can take with you from room to room. It provides security, because not only can you answer the phone without rushing for it, but you can also call for help should an accident occur.
- Don't let prescriptions run low. Always keep at least one week's worth of medications on hand at home.
- Check prescriptions with your doctor and pharmacist to see if they may be increasing your risk of falling. If you take multiple medications, check with your doctor and pharmacist about possible interactions between the different medications.
- Arrange with a family member or friend for daily contact. Try to have at least one person who knows where you are.
- If you live alone, you may wish to contract with a monitoring company that will respond to your call 24 hours a day.
- Watch yourself in a mirror. Does your body lean or sway back and forth or side to side? People with decreased ability to balance often have a high degree of body sway and are more likely to fall.
Practice Balance Exercises Every Day:
While holding the back of a chair, sink, or countertop, practice standing on one leg at a time for a minute. Gradually increase the time. Try balancing with your eyes closed. Try balancing without holding on.
While holding the back of a chair, sink, or countertop, practice standing on your toes, then rock back to balance on your heels. Hold each position for a count of 10.
While holding the back of chair, sink, or countertop with both hands, make a big circle to the left with hips, repeat to the right. Do not move your shoulders or feet. Repeat 5 times.
Reducing the Force of a Fall
Take steps to lessen your chances of breaking a bone in the event that you do fall:
- Remember that falling sideways or straight down is more likely to result in a hip fracture than falling in other directions. If possible, try to fall forward or to land on your buttocks.
- If possible, land on your hands or use objects around you to break a fall.
- Walk carefully, especially on hard surfaces.
- When possible, wear protective clothing for padding.
- Talk to your doctor about whether you may be a candidate for hip padding.
Decreasing Bone Fragility
Individuals can protect bone health by following osteoporosis prevention and treatment strategies:
- Consume a calcium-rich diet that provides 1,200 mg (milligrams) of calcium from a combination of foods and supplements.
- Obtain between 200 to 600 IU (International Units) of vitamin D each day, depending on age.
- Participate in weight-bearing and resistance-training exercises most days, preferably daily.
- Talk with your doctor about having a bone mineral density (BMD) test. The most widely recognized bone mineral density test is called a dual-energy x-ray absorptiometry or DXA test. It is painless: a bit like having an x ray, but with much less exposure to radiation. It can measure bone density at your hip and spine.
- Talk with your doctor about possibly beginning a Food and Drug Administration-approved medication for osteoporosis to stop bone loss, improve bone density, and reduce fracture risk.
People need to know whether they are at risk for developing osteoporosis or whether they have lost so much bone that they already have osteoporosis. While risk factors can alert a person to the possibility of low bone density, only a BMD test can measure current bone density, diagnose osteoporosis, and determine fracture risk. There are many different techniques that measure bone mineral density painlessly and safely. Most of them involve machines that use extremely low levels of radiation to complete their readings. Sometimes, ultrasound machines, which rely on sound waves, are used instead.
Individuals may wish to have a bone mineral density test to determine current bone health. Today, Medicare and many private insurance carriers cover bone density tests to detect osteoporosis for individuals who meet certain criteria. Talk with your doctor about whether or not this test would be appropriate for you. Falls are serious, but there are simple, inexpensive steps that can be taken to reduce your risk for falling and reduce your risk of breaking a bone if you do fall.
Resources
-
For additional information on osteoporosis, visit the National Institutes of Health Osteoporosis and Related Bone Diseases ~ National Resource Center Web site at www.niams.nih.gov/Health_Info/Bone/default.asp or call 1-800-624-2663.
For additional information on fall prevention, visit the National Institute on Aging Web site at www.niapublications.org/engagepages/falls.asp or call 1-800-222-2225.
For Your Information
For updates and for any questions about any medications you are taking, please contact the U.S. Food and Drug Administration at:
-
U.S. Food and Drug Administration
Toll Free: 888-INFO-FDA (888-463-6332)
Website: http://www.fda.gov/
The National Resource Center acknowledges the assistance of the National Osteoporosis Foundation in the preparation of this publication.
NIH Osteoporosis and Related Bone Diseases ~ National Resource Center
2 AMS Circle
Bethesda, MD 20892-3676
Phone: 202–223–0344
Toll Free: 800–624–BONE
TTY: 202-466-4315
Fax: 202-293-2356
Email: NIAMSBoneInfo@mail.nih.gov
Website: http://www.niams.nih.gov/Health_Info/bone/default.asp
The NIH Osteoporosis and Related Bone Diseases ~ National Resource Center provides patients, health professionals, and the public with an important link to resources and information on metabolic bone diseases. The mission of NIH ORBD~NRC is to expand awareness and enhance knowledge and understanding of the prevention, early detection, and treatment of these diseases as well as strategies for coping with them.
The NIH Osteoporosis and Related Bone Diseases ~ National Resource Center is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases with contributions from:
- National Institute on Aging
- Eunice Kennedy Shriver National Institute of Child Health and Human Development
- National Institute of Dental and Craniofacial Research
- National Institute of Diabetes and Digestive and Kidney Diseases
- NIH Office of Research on Women's Health
- DHHS Office on Women's Health.
The National Institutes of Health (NIH) is a component of the U.S. Department of Health and Human Services (DHHS).
Most of our bone publications are available online only. Some are available in print. Would you like to order publications on bone disorders to be mailed to you? Visit our online order form.