
|
 |
Hospital eTool
Surgical Suite Module
Click on the area for more specific information.

|
Common safety and health topics:
The anesthetic gas and vapors that leak out and into the surrounding room during medical
procedures are considered waste anesthetic gases, including nitrous oxide and halogenated agents (vapors) such as
halothane, enflurane, methoxyfluorane,
trichloroethylene, and chloroform. Exposure to waste gases usually results from
poor work practices during the anesthetization of patients, leaking or poor gas-line connections, improper or
inadequate maintenance of the machine, and/or patient exhalation after the surgical procedure, while in recovery.
|
Potential Hazard

|
Exposure of employees to waste anesthetic gases during surgical procedures in the
operating room and also in the recovery room or Post Anesthesia Care Unit (PACU), during off-gassing of surgery patients.
Some potential health effects of exposure to waste anesthetic gases include nausea, dizziness, headaches, fatigue, irritability,
drowsiness, problems with coordination and judgment, as well as sterility, miscarriages, birth defects, cancer, and liver and kidney
disease.
|
Possible Solutions
-
Anesthetic Gases: Guidelines for Workplace Exposures. OSHA advisory guidelines (2000, May 18), suggests the following:
- Use appropriate anesthetic gas scavenging systems in Operating Rooms. Appropriate waste gas evacuation
involves collecting and removing waste gases, detecting and correcting leaks, considering work practices, and effectively ventilating
the room (Dorsch and Dorsch 1994).
- To minimize waste anesthetic gas concentrations in the operating room the recommended air exchange rate (room dilution ventilation)
is a minimum total of 15 air changes per hour with a minimum of 3 air changes of outdoor air (fresh air) per hour (American Institute of
Architects 1996-1997). Do not recirculate operating room air containing waste anesthetic gases to the operating room or
other hospital locations.
- A properly designed and operating dilution ventilation system should be relied upon to minimize waste anesthetic
gas concentrations in recovery room areas.
- This system should provide a recommended minimum total of 6 air changes per hour with a minimum of 2 air changes of outdoor air per
hour to adequately dilute waste anesthetic gases (American Institute of Architects 1996-1997). Do not recirculate room
exhaust containing waste anesthetic gases to other areas of the hospital.
- Periodic exposure monitoring with particular emphasis on peak gas levels in the breathing zone of nursing personnel working in the
immediate vicinity of the patient's head. Methods using random room sampling to assess ambient concentrations of waste anesthetic gases
in the recovery room are not an accurate indicator of the level of exposure experienced by nurses providing bedside care. Because of
the closeness of the recovery room nurse to the patient, such methods would consistently underestimate the level of waste anesthetic
gases in the breathing zone of the bedside nurse.
- Apply a routine ventilation system maintenance program to keep waste gas exposure levels to a minimum.
- OSHA Tech Manual Section VI,
Chapter 1 - Health Hazards recommends:
- Turn off vaporizers of anesthesia machines when not in use. Also, proper face masks, sufficiently inflated endotracheal tubes, and
prevention of anesthetic spills will decrease the amount of waste anesthetic gases in the operating room.
- Inspect and maintain the anesthesia machine at least every four months. This should be done by factory service representatives or
other qualified personnel. Leakage of gas should be less than 100 ml/min during normal operation.
- Good work practice recommends complete check of all anesthesia equipment prior to each day's use (connectors, tubing, etc.) spills
of liquid anesthetic agents cleaned up promptly.
- Implement information and training program for all employers exposed to waste anesthetic gases, complying with OSHA's Hazard
Communication Standard. See HealthCare Wide Hazards -
Hazardous Chemicals.
Additional Information:
- Waste Anesthetic Gases,
Safety and Health Topics Page.
- Anesthetic Gases:
Guidelines for Workplace Exposures. OSHA Directorate of Technical Support, and the Office of Science and Technical Assessment
(2000, May 18). This document provides guidelines and controls to help reduce occupational exposure to waste anesthetic gases.
- Waste Anesthetic Gases.
OSHA Fact Sheet 91-38, (1991), 2 pages. Basic overview of waste anesthetic gases, including exposure limits and work
practice controls.
-
Controlling Exposures to Nitrous Oxide During Anesthetic Administration. NIOSH Alert: (1994), 8 pages. Department of Health and
Human Services (DHHS) and the National Institute for Occupational Safety and Health (NIOSH) Publication No. 94-100. This
alert presents control measures for preventing or greatly reducing exposure to nitrous oxide (N2O) during the administration
of anesthetic gas.
|
|
|
Potential Hazard
Exposure to blood and OPIM and life threatening BBPs such as Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), and Human
Immunodeficiency Virus (HIV).
Possible Solutions
Follow the requirements of the
Bloodborne Pathogens Standard such as:
- Wear appropriate PPE as required by the Bloodborne Pathogens Standard
1910.1030(d)(3)(ix)]
if blood or Other Potentially Infectious Materials (OPIM) exposure is anticipated. The type and amount of PPE
depends on the anticipated exposure including:
- Gloves must be worn when hand contact with blood, mucous membranes, OPIM, or non-intact skin is anticipated, or when handling
contaminated items or surfaces
[1910.1030(d)(3)(ix)].
- Provide effective engineering and work practice controls to help remove or isolate exposures to blood
and bloodborne pathogens
[1910.1030(c)(1)(iv)(B),
1910.1030(d)(2)(i), and
OSHA Directive CPL 2-2.69.
- Minimize the hazards of exposure to BBPs in the surgery area by promoting the use of:
- Safer needle/other sharps device
- Blunt suture needles
- Needleless IV connectors
- Proper containerization of sharps
- "No Pass Zone" for surgical instruments
- A Hands-free technique for passing instruments The hands-free technique is a work practice whereby a tray or other means are used to
eliminate simultaneous handling of sharp instruments during surgery.
The Effectiveness of the Hands-Free Technique in Reducing Operating Room Injuries. NIOSH (2001, November), 62KB PDF.
- Method for passing equipment safely between surgeon and assistants
The Bloodborne Pathogens Standard also requires:
- Discarding of contaminated needles and other sharp instruments immediately or as soon as feasible after
use into appropriate containers
[1910.1030(d)(4)(iii)(A)(1)].
- Sharps containers need to be available, and in close proximity to areas where sharps may be found...
[1910.1030(d)(4)(iii)(A)(2)].
- Contaminated needles and other contaminated sharps shall not be bent, recapped, or removed except as noted in paragraphs (d)(2)(vii)(A)
and (d)(2)(vii)(B).
- Employers must provide readily accessible hand washing facilities,
[1910.1030(d)(2)(iii)]
and ensure that employees wash their hands immediately or as soon as feasible after removal of gloves
[1910.1030(d)(2)(v)].
 For additional information, see HealthCare Wide Hazards -
Bloodborne Pathogens, and
Needlesticks.
For additional information, see HealthCare Wide Hazards -
Bloodborne Pathogens, and
Needlesticks.
|
|
|
Potential Hazard
Developing latex allergy from exposure to latex from using products that contain latex such as, gloves, catheters, tubing.
Possible Solutions
OSHA requires:
- Employers to provide appropriate gloves for employees to wear, including "hypoallergenic gloves, glove liners, powderless
gloves or other similar alternatives" to employees who are allergic to the gloves normally provided
1910.1030(d)(3)(iii).
Please note that hypoallergenic gloves are not to be assumed to be non-latex or latex-free.
Good work practice includes:
- Provide a latex-free work environment
- Use non-latex gloves and other latex-free products.
- If latex must be used, choose a low protein, powder-free glove. (Powder-free gloves seem to reduce systemic allergic responses.)
 For additional information, see HealthCare Wide Hazards -
Latex Allergy.
For additional information, see HealthCare Wide Hazards -
Latex Allergy.
|
|
|
Potential Hazard
 Fire, explosion, and toxicity of compressed gases. These effects arise from the compression of the gas and the health effects of
the chemical itself. Compressed gases within a healthcare facility are usually either fixed piped gas systems or individual
cylinders of gases.
Fire, explosion, and toxicity of compressed gases. These effects arise from the compression of the gas and the health effects of
the chemical itself. Compressed gases within a healthcare facility are usually either fixed piped gas systems or individual
cylinders of gases.
Possible Solutions
Handle compressed gases in accordance with Compressed Gas Association Pamphlet P-1-1965 which is incorporated by reference as
specified in 29 CFR 1910.6. Other guidance regarding safe handling of medical gases is included in NFPA 99 Standard for Health
Care Facilities, Chapter 4 Gas and Vacuum Systems.
 Keep cylinders of compressed gases secured. They should never be dropped or allowed to strike each other with force. Keep cylinders of compressed gases secured. They should never be dropped or allowed to strike each other with force.
Additional Information:
|
|
Static or Awkward Postures
|
Potential Hazard
Exposure of staff to:
- Static postures from continuously standing in one position during lengthy surgical
procedures, causing muscle fatigue and pooling of blood in the lower extremities. Standing on hard work surfaces such as
concrete creates trauma and pain to feet.
- Awkward postures from tilting head downwards for long periods of time.
Possible Solutions
| |
- Provide stools where their use is possible.
|
| |
- Use shoes with well cushioned insteps and soles.
|

|
- Provide a foot rest bar or a low stool, so employees can continually alter their posture by raising one foot.
|
| |
- Use height adjustable work surfaces.
|
|
During surgical procedures that use a laser or electro-surgical unit, the thermal destruction of tissue creates a smoke
byproduct. An estimated 500,000 workers are exposed to laser or electro-surgical smoke each year, including surgeons, nurses,
anesthesiologists, and surgical technologists.
|
Potential Hazard
According to NIOSH research studies have confirmed that this smoke plume can contain toxic gases and vapors such as benzene,
hydrogen cyanide, and formaldehyde, bioaerosols, dead and live cellular material (including blood fragments), and viruses.
At high concentrations the smoke causes ocular and upper respiratory tract irritation in health care
personnel, and creates visual problems for the surgeon. The smoke has unpleasant odors and has been shown to have mutagenic
potential. Although there has been no documented transmission of infectious disease through surgical smoke, the
potential for generating infectious viral fragments, particularly following treatment of venereal warts, may exist.
Researchers have suggested that the smoke may act as a vector for cancerous cells which may be inhaled by the surgical team
and other exposed individuals.
Possible Solutions
- Engineering Controls: Use portable smoke evacuators and room suction systems.
- Work practice Controls:
- Keep the smoke evacuator or room suction hose nozzle inlet within 2 inches of the surgical site to effectively capture
airborne contaminants.
- Keep smoke evacuator ON (activated) at all times when airborne particles are produced during all surgical or other
procedures.
- Consider all tubing, filter, and absorbers as infectious waste and dispose of them appropriately.
- Install new filters and tubing before each procedure.
- Inspect smoke evacuator systems regularly to prevent possible leaks.
- Use
Universal Precautions as required by the OSHA Bloodborne Pathogens Standard
[1910.1030(d)(1)].
Additional Information:
|
|
|
Potential Hazard
Exposure of employees to lasers used in the operating rooms during excision and cauterization of tissue. Class 3b and 4
lasers are most often used. Exposure usually occurs from unintentional operation and/or when proper controls are not in
effect. The high electrical energy used to generate the beam is a potential shock hazard. Direct beam exposure can cause
burns to skin and eyes possibly resulting in blindness. Electric shock and fire are also potential hazards when using lasers.
The four classes of laser are:
Class 1
|
The least-hazardous class. Considered incapable of providing damaging levels of laser emissions.
|
Class 2
|
Applies only to visible laser emissions and may be viewed directly for time periods of less than or equal to 0.25 seconds, which
is the aversion response time.
|
Class 3a
|
Dangerous under direct or reflected vision. These lasers are restricted to the visible electromagnetic spectrum.
|
Class 3b
|
May extend across the whole electromagnetic spectrum and are hazardous when viewed intrabeam.
|
Class 4
|
The highest-energy class of lasers, also extending across the electromagnetic spectrum. This class of laser presents significant
fire, skin, and eye hazards.
|
Possible Solutions
The OSHA Tech Manual Section VI, Chapter 1-Health
Hazards recommends:
|
Sample Laser Signs
|
|
|
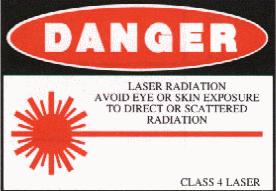
Class 4 - Laser Sign |

Class 2-Laser Sign |
- Maintain and service the entire laser system according to the manufacturer's instructions. Only qualified personnel from the
manufacturer or in-house should maintain the system. Maintenance may only be done according to written standard operating procedures
and must meet the requirements of the Lockout/Tagout Standard
1910.147.
- Adequately cover laser systems, especially ones with high voltage capacitance. Also, attach bleeders and proper grounding to the
system. All operating room doors to rooms that house lasers should contain safety interlocks which shutdown the laser system if anyone
enters the room.
- Cover or black out, all windows in laser surgical areas to protect employees outside the surgical area.
- Lasers are calibrated by the manufacturer, but check the laser system before each procedure and during extended procedures.
Classifications of lasers should coincide with actual measurement of output. Generally, measurements are required when the manufacturer's
information is not available, when the laser system has not been classified, or when alterations have been made to the laser system that
may have changed its classification. Only personnel trained in laser technology should make measurements.
Guidelines for Laser Safety and Hazard Assessment PUB 8-1.7 General Basic Safety Precautions, provides guidelines including:
- Skin Protection can best be achieved through engineering controls. If the potential exists for damaging skin exposure, particularly
for ultraviolet lasers (200-400 nm), then skin covers and or "sun screen" creams are recommended.
- Hands - Most gloves will provide some protection against laser radiation. Tightly woven fabrics and opaque gloves provide the
best protection.
- Arms - A laboratory jacket or coat can provide protection for the arms. For Class IV lasers, consideration should be given to
flame resistant materials.
- Personnel should use protective clothing when exposed to levels of radiation that exceed the Maximum Permissible Exposure for
the skin.
Additional Information:
- 1926.54, Nonionizing radiation.
- Laser Hazards,
Safety and Health Topics Page.
- Laser Hazards, OSHA Technical Manual, Section III, chapter 6.
-
Guidelines for Laser Safety and Hazard Assessment. OSHA Instruction PUB 8-1.7 (1991, August 5), 70 pages.
- Laser Hazards. OSHA Technical Manual (TED 1-0.15A),
Section III - Chapter 6 (1999, January 20), 51 pages. This chapter contains information that will assist in the recognition and
evaluation of laser hazards.
- The
American National Standards Institute (ANSI) has developed several standards on laser hazards and non-beam hazards. They are
recognized as a minimum standard for laser safety. These are available for purchase.
- ANSI Z136.1-1993: American National Standard for the Safe Use of Lasers.
- ANSI Z136.3-1996: American National Standard for the Safe Use of Lasers in the Health Care Environment.
|
|
|
|
Potential Hazard
Exposure to possible hazardous chemicals found and used in the surgical area, e.g., paracetic acid used in cold sterilant
machines and Methyl Methacrylate (MMA) an acrylic cement-like substance used to secure prostheses to bone during orthopedic
surgery. Exposure usually occurs during mixing, preparation, and in the operating room.
Possible Solutions
- Mix Methyl Methacrylate only in a closed system.
- Employees should carefully read and follow instructions and warnings on labels, (e.g., when using cold sterilant machines for
sterilizating equipment that cannot be autoclaved, use goggles provided and do not open machine until it is in a
safe to open mode).
- Employees should follow all MSDS instructions regarding safe handling, storage, and disposal of hazardous chemicals.
- Employers should consider using disinfectants or other products that are not hazardous.
- According to the
Hazard Communication Standard: Employers must inform employees of chemical hazards and have on hand Material Safety
Data Sheets, (MSDS) for all hazardous chemicals used in their facilities.
 For additional information, see HealthCare Wide Hazards -
Hazardous Chemicals.
For additional information, see HealthCare Wide Hazards -
Hazardous Chemicals.
|
|
|
Potential Hazard
Staff exposure to burns or shocks from poorly maintained equipment or improperly trained staff (e.g., autoclaves, warming
cabinets, defibrillators).
Possible Solutions
A safety and health program that routinely monitors the condition of equipment and addresses work practices of employees:
- Train employees to correctly and safely use equipment.
- Maintain adequate working space and access to equipment.
- Visually inspect cords. Do not use if frayed or damaged. Equipment cords should be grounded.
- Visual inspection of equipment before using.
- If something doesn't look right, don't use the machine, and call for assistance.
- Ensure that all electrical service near sources of water is properly grounded
[1910.304(f)(5)(v)].
- Use appropriate personal protective equipment and safe work practices for assessed hazards (e.g., when handling hot items
use gloves, and don't open autoclaves or sterilizers until items are sufficiently cooled.
 For additional information, see HealthCare Wide Hazard -
Electrical, and
PPE.
For additional information, see HealthCare Wide Hazard -
Electrical, and
PPE.
|
|
|
Potential Hazard
Staff exposure to trips, and falls, e.g., falling over portable equipment that easily blends into the floor or slipping on
debris, (bandages, tubing, blood, IV fluids) that are spilled on the floor. Electrical cords crossing floors may also be a
trip hazard.
Possible Solutions
| |
- Walking/Working Surfaces Standard requires
[1910.22(a)(1)]:
All places of employment shall be kept clean and orderly and in a sanitary condition.
|
| |
- Aisles and passageways shall be kept clear and in good repairs, with no obstruction across or in aisles that could create a
hazard [1910.22(b)(1)].
Provide ceiling or floor plugs for equipment, so power cords need not run across pathways.
|

|
- Mark mobile equipment with a bright color, or a tape "X", to help distinguish it from the floor and make it more
visible to employees.
|
|
|

