|
 |
- HealthCare Wide Hazards Module -
Tuberculosis
Nearly one-third of the world's population is infected with Tuberculosis (TB),
and it kills almost 3 million people
per year. However, in the United States, through a broad range of Federal and community initiatives including
the Centers for Disease Control and Prevention (CDC) 1994 publication, Guidelines
for Preventing the Transmission of Mycobacterium Tuberculosis in Health Care
Facilities, national TB rates have declined steadily
over the past decade. The number of reported TB cases and the national TB case
rate are now at their lowest levels since
TB reporting began in 1953. *Note The OSHA proposed
standard for Tuberculosis,
has been withdrawn. Respiratory protection from tuberculosis is
now covered under OSHA's Respiratory Standard
1910.134.
Click on the area for more specific information.
|
Common safety and health topics:
TB disease in persons over the age of 65 constitutes a large proportion of TB cases in the United States. Many of these individuals
have latent TB infection; however, with aging these individuals' immune function starts to decline, placing them at increased risk of
developing active TB disease, and employees in long-term care facilities at
risk of occupational exposure to TB.
|
Potential Hazard
Exposure to Mycobacterium tuberculosis and Multidrug-resistant (MDR) TB:
Mycobacterium tuberculosis: TB is caused by the bacteria Mycobacterium tuberculosis
and is spread by airborne droplets generated when a person with TB disease coughs, speaks, sings, sneezes, etc. Infection occurs when a
susceptible person inhales droplet nuclei containing the bacteria, which then become established in the body.
Additional hazard is now present because of
multidrug-resistant
(MDR) TB. MDR organisms are resistant to the drugs that are normally used to treat TB, such as
Isoniazid and Rifampin. The course
of treatment when treating MDR TB increases from 6 months to 18-24 months, and the cure rate decreases from nearly 100% to less than
60%. Mortality among patients with MDR-TB can be high.
Possible Solutions
Implement an effective control program which minimizes exposures to TB.
*NOTE: Not all controls discussed in this
eTool are required by OSHA, however, employers with employee exposure to
TB must comply with certain requirements including:
1910.134
- Respiratory Protection,
1910.145 - Accident Prevention Signs and Tags,
1904 - Recordkeeping, and Section
5(a)(1) - General Duty Clause.
Enforcement Procedures
OSHA's enforcement procedures are addressed in:
-
Tuberculosis
and Respiratory Protection. Interpretation letter, (2004, July 30), 2 pages. This
memorandum defines the new enforcement policy for tuberculosis under
1910.134. Effective July 2, 2004. Covered establishments must comply
with 1910.134 when using respirators for protection from tuberculosis
(TB).
- Comparison of Respiratory Protection (29 CFR
1910.139) with (29 CFR 1910.134). 132 KB PDF,
29 pages. Most of the requirements in 1910.134 and the former
1910.139 are basically the same, however five areas now have more
detailed requirements; Medical Evaluations -
(e), Fit-testing
-
(f),
Written Program - (c), Training
-
(k), and Recordkeeping
-
(m).
-
OSHA
Directive CPL 2.106, Enforcement Procedures and Scheduling for
Occupational Exposure to Tuberculosis (1996, February 9), 105 pages.
- Except for specific standards (e.g., 1910.134,
1904.11,
1910.145) enforcement for TB is based on
the OSHA General Duty Clause Section
5(a)(1)
which provides: "Each employer shall furnish to each of his employees employment and a place of employment which are free from
recognized hazards that are causing or are likely to cause death or serious physical harm to his employees."
|
The CDC guidelines outline an effective TB infection control program including:
- Early identification, isolation, and treatment of persons with TB, (e.g., provide and practice early patient screening in the
Emergency Department,
to identify potentially infectious patients, and prevent employee exposures.
- The use of engineering and administrative procedures to reduce the risk of exposure.
- The use of respiratory protection.
Directive
CPL
2.106 using the Appendix A, CDC Guidelines, PDF,
addresses protection from the following types of TB exposures:
- Exposure to the exhaled air of an individual with suspected or confirmed pulmonary TB disease.
- A suspected case is one in which the facility has identified an individual as having symptoms consistent with TB. The CDC has
identified the symptoms to be: productive cough, coughing up blood, weight loss, loss of appetite, lethargy/weakness, night sweats, or
fever.
- Employee exposure without appropriate protection to a high hazard procedure performed on an individual with suspected or confirmed
infectious TB disease and which has the potential to generate infectious airborne droplet nuclei.
- Examples of high hazard procedures include aerosolized medication treatment, bronchoscopy, sputum induction, endotracheal intubation
and suctioning procedures, emergency dental, endoscopic procedures, and autopsies conducted in hospitals.
The following are examples of feasible and useful
abatement methods, which are addressed by Directive
CPL 2.106, and OSHA standards (e.g.,
1910.134, and
1910.145):
|
|
Screening, Medical Surveillance, Case Management
|
Potential Hazard
Exposure to TB because of ineffective:
Possible Solutions
The protocol for early identification of individuals
with active TB starts with the following elements:
Screening of Residents:
Prompt implementation of early screening procedures, and staff training to
help them identify potentially infectious individuals, will allow
for early identification of patients with infectious TB and the
initiations of appropriate controls before
occupational exposure occurs to staff and other patients.

|
Exposure Control Plan (Non-mandatory): Control of exposure to
TB can be readily addressed in a facility's Exposure Control Plan (ECP).
An ECP helps employers prevent exposure to TB in their facilities.
Risk Assessment:
Nursing homes or long-term care facilities for the elderly have been identified as having a
high-risk situation for the transmission of TB. The degree of risk of occupational exposure of a worker to TB will vary based on a number of factors discussed in
detail by the CDC and (Directive CPL
2.106 Appendix A, PDF
141 pages, pg. 4-5).
- To assist employers in establishing a baseline risk assessment for TB in a particular facility the
CDC offers:
|
Medical Surveillance of employees according to
Directive CPL 2.106 includes:
- Medical surveillance at no cost to the employees,
- Medical surveillance for all current potentially exposed employees and for all new employees prior to exposure.
- Medical surveillance consists of: employee medical evaluation and management, post-exposure follow-up and administering periodic
and baseline TB skin testing. Only skin testing is addressed here. See
OSHA Directive CPL 2.106
for further information.
-
TB
Skin Testing:
- Mantoux tuberculin skin test detects TB infection and helps monitor, identify and address conversion rates:
- Baseline TB testing a two-step test method is required on initial skin test, provided they have not had a negative skin test with
in the last year.
- Frequency of skin testing is determined by the risk assessment of your particular facility.
- Retesting required every three months, for high risk facilities.
- Six months for workers in intermediate facilities.
- Yearly testing for low risk personnel.
- See the CDC
guidelines, OSHA Directive CPL 2.106 Appendix A, PDF,
pages 8-17, for definitions of risk categories.
Case Management of Infected Employees
Exposure to the adverse affects of TB infection can occur due to inadequate case management.
According to Directive CPL 2.106
effective case management of infected employees includes:
- Protocol for New Converters
[Directive CPL 2.106
Appendix A].
- An employee's conversion to a positive TB skin test is followed as soon as possible by appropriate; physical, laboratory, and
radiographic evaluations to determine whether the employee has infections TB disease.
[Appendix A, PDF,
page 40 sec 4] . TB
test skin conversions protocol.
- Work Restrictions for Infectious Employees
[Directive CPL 2.106
Appendix A - PDF,
page 41].
|
|
Training and Education
|
Potential Hazard
Exposure to TB due to lack of training or education (employees are not aware of the tasks or procedures that
may involve risks of exposure to TB).
Possible Solutions
OSHA's Respiratory Protection Standard 1910.134(c)(1)(viii),
Requires training of employees in the respiratory hazards to which they
are potentially exposed during routine and emergency situations.
OSHA Directive CPL 2.106,
L.4., Training and education of employees about TB hazards includes:
- Mode of TB transmission, its signs and symptoms, medical surveillance and therapy, and site specific protocols including the purpose
and proper use of controls [Appendix A, - PDF,
pages 36-37].
- Employee education about recognizing and reporting to a designated person, any patients or clients with symptoms suggestive of
infectious TB, as well as post exposure protocols to be followed in the event of an exposure incident [Appendix A,
PDF,
page 23].
OSHA's Respiratory Protection Standard 1910.134(c)(4)
also requires employers to provide
respirator training,
medical
evaluations,
fit-testing,
written program, and
recordkeeping at no cost to the employee.
Additional Information:
|
|
Isolation
|
Potential Hazard
Exposure to TB because of:
- Failure to promptly isolate and mask those patients with suspected infectious TB.
- Adequate transfer procedures were not provided and/or used.
Possible Solutions
Provide adequate isolation for those patients with TB or suspected TB.
OSHA Directive CPL 2.106,
states individuals with suspected or confirmed infectious TB disease must
be placed in a respiratory acid-fast bacilli (AFB) isolation room. High
hazard procedures on individuals with suspected or confirmed infectious TB
disease must be performed in AFB treatment rooms, AFB isolation rooms,
booths, and/or hoods. (AFB isolation refers to a negative pressure room or
an area that exhausts room air directly outside or through HEPA filters if
recirculation is unavoidable).
Transferring of patients: The CDC recommends
that facilities who have determined a resident has suspected infectious TB, and do not
intend to provide treatment for TB patients:
- May choose to promptly transfer a patient to a facility that provides service to individuals who need isolation.
- It is recommended that the facility's exposure control plan have in place procedures for transferring infectious individuals such
as:
- Masking and segregation of the individual until transfer can be arranged.
- The time to transfer should be as soon as feasible.
- Temporary isolation can be provided by placing a portable stand-alone HEPA filtration unit (vented to the outside) in an unused
exam room, booth tent or other enclosure if the time to get someone transferred may take an extended period.
|
|
Isolation Rooms
|
Potential Hazard
Exposure to TB because of isolation room failure:
- Equipment failure, not working properly.
- Isolation doors left open or excessive traffic in room.
Possible Solutions
Facilities that choose to provide service to residents with confirmed or suspected TB need to provide appropriate
isolation rooms [OSHA Directive
CPL 2.106, L.1.e.5 (1996, February 9)]. Individuals with
suspected or confirmed infectious TB disease must be placed in a
respiratory acid-fast bacilli (AFB) isolation room. AFB isolation refers to a negative pressure
room or an area that exhausts room air directly outside or through HEPA
filters if recirculation is unavoidable.
- Use respiratory acid-fast bacilli (AFB) isolation rooms:

|
- A switch outside the room equipped with an indicator light flipped to the "on" position is one way to indicate the
negative pressure has been activated in the room.
|
|
- Isolation rooms are maintained at negative pressure to prevent the escape of aerosolized M. tuberculosis
from the infected patient's room into outside corridors and unprotected employees and patients.
|
|
|
|
- Keep doors closed except for the purpose of entering or exiting to help maintain negative pressure in room.
|
|
- Limit access to these rooms to specific employees.
|

|
- Combine tasks to prevent excessive traffic in the room. For example:
- Rather than having the dietary aide bring in food, the nurse could combine tasks by bringing in food with medications and bedding
as she performs morning care for the patient.
|

|
- Locate air intake ducts away from doors.
|

|
- Regularly inspect HEPA filters and other devices used in isolation rooms to demonstrate installed effectiveness.
|
|
- To monitor and check for negative room pressure the smoke trail method can be used. Explanation of smoke trail testing procedures
can be found in:
|

|
- Vent isolation room air to the outdoors away from intake vents and employees. If the air from these areas cannot be vented to the
outside, filter air before it can be recirculated back into other areas of the facility through a HEPA filter.
|
Additional Information:
In September of 1999, the Joint
Commission on Accreditation of Healthcare Organizations (JCAHO) Committee on Healthcare Safety recommended that JCAHO update its
Environment of Care Standard for Utility Systems Management, including the Comprehensive Accreditation Manual for Long Term Care to
include and address issues of improperly designed and maintained ventilation systems (including inappropriate pressure relationships,
air exchange rates, and filtration efficiencies).
|
|
|
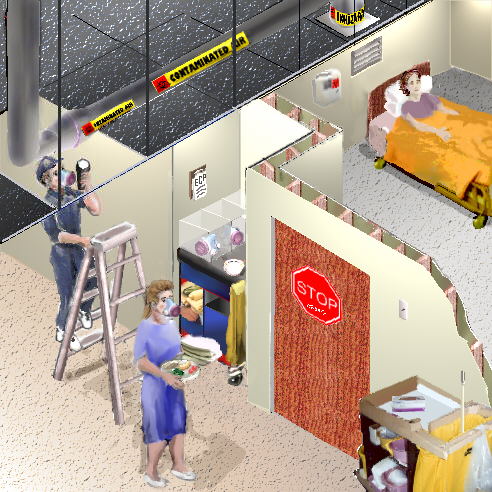
Warning Signs and Tags
|
Potential Hazard
Exposure to TB because of inadequate signs or labels, such as:
- Isolation and treatment rooms not labeled properly.
- Exposure to TB through unlabeled contaminated ducts, fans, filters.
Possible Solutions
Enforcement
Procedures and Scheduling for Occupational Exposure to Tuberculosis [OSHA Directive CPL 2.106, L.4.].
Employees must receive adequate information about the hazards of TB through the use of labels and signs, as indicated in
1910.145 Accident Prevention Signs and
Tags. OSHA requires that signs must be posted at the entrance to:
|
- Rooms or areas used to isolate an individual with suspected or confirmed infectious TB (TB isolation rooms for
example).
|
|
- Rooms or areas where procedures or services are being performed on an individual with suspected/confirmed TB.
|
|
Warning signs shall be posted outside the Respiratory isolation or treatment room. The sign
must include a signal word (e.g. "STOP", HALT", or "NO ADMITTANCE") or biological hazard symbol and a
descriptive message (e.g., "Respiratory Isolation, No Admittance Without Wearing a Type N95 or More Protective Respirator",
or "See nurses' station before entering this room")
[1910.145(f)(4)].
|

|
- Employers must use biological hazard tags on air transport components (e.g., fans, ducts,
filters), that may reasonably contain air infected with M. tuberculosis to warn employees, temporary employees, or contractors of
possible hazards of contamination
[OSHA Directive CPL 2.106,
L.4. (1996)].
|

|
- Example wording for warning label: "Contaminated Air--Respiratory Protection Required."
|
|
|
Respiratory Protection
|
Potential Hazard
Exposure to TB due to:
- Improper use or fit of respirator, or improper reuse of damaged or soiled respirators.
- Ineffective respiratory protection program.
Possible Solutions
OSHA's Respiratory Protection standard
1910.134
states that the employer is responsible to establish and maintain a
complete respiratory protection program that assures respirators are
properly selected, fitted, used, and maintained regularly.
-
Respiratory Protection Program Guidelines. OSHA CPL 2-254A (2000,
July 14), 18 pages. This instruction sets forth guidelines for
establishing and implementing an OSHA respirator program to ensure that
all OSHA employees are protected from exposure to respiratory hazards.
Employer must
also provide a medical evaluation to determine the employee's ability to
use a respirator [1910.134(e)].
-
1910.134 App C, OSHA Respirator Medical Evaluation Questionnaire
(Mandatory).

|
|

|
- The directive CPL 2.016, L.2.a. specifies the CDC guidelines for standard performance criteria for respirators for exposure to TB.
These criteria include: wearing NIOSH-approved high-efficiency particulate air (HEPA) filtered respirator, or Class N95 or more
protective respirator whenever the employee:
- Enters rooms housing individuals with suspected or confirmed infectious TB.
- Is present during the performance of high hazard procedures or services for an individual with suspected or confirmed infectious
TB.
- Transports an individual with suspected or confirmed TB in a closed vehicle.
|
|
- Requirements for a minimal acceptable program are found in 1910.134(b), and include among
other things:
|
|
- Employee instruction on correct fit and use of respirators
[1910.134(k)].
Every respirator wearer shall receive fitting instructions including demonstrations and practice in how the respirator should be worn,
how to adjust it, and how to determine if it fits properly.
- Fit Testing is covered in the OSHA Technical Manual
and OSHA CPL
2-2.29 (1980, October 27).
Employees must be fit tested before using their respirators and annually or whenever a change occurs (i.e., different size, model, or respirator
design or facial shape) [1910.134(f), 1910.134(e)(5)].
- Providing respiratory protection for persons who wear glasses may be a
problem; a proper seal must be maintained [1910.134(g)(1)(ii)].
- Respirators cannot be worn with facial hair that interrupts the face-to facepiece seal or valve function [1910.134(g)(1)(i)].
|
|
- Standard operating procedures for storing, reusing, and disposing of
respirators [1910.134(h) CPL 2.106, L.2.a.3].
|

|
- For example, a disposal container could be provided on the cart outside the room to store soiled
reusable respirators until they can be cleaned for reuse.
|
|
- Respirators shall be regularly cleaned and disinfected. Those used by
more than one worker shall be thoroughly cleaned and disinfected after
each use [1910.134(h)(1)(i)-(iv)].
1910.134 App B-2, Respiratory Cleaning Procedures (Mandatory).
- Disposable respirators can be reused (by the same HCW), as long as the functional and structural integrity of the respirator is
maintained. The outside of the filter material should be inspected before each use:
- If the filter material is physically damaged or soiled, the filter should be changed or discarded.
- Health care facilities' policies specify whether cleaning or sterilizing an item is necessary
[CDC
Guidelines- Appendix
A].
|
Additional Information:
- Enforcement
Procedures and Scheduling for Occupational Exposure to Tuberculosis [OSHA Directive CPL 2.106 (1996, February 9)].
-
Respiratory Protection Program Guidelines. OSHA CPL 2-254A (2000, July
14), 18 pages. This instruction sets forth guidelines for establishing and
implementing an OSHA respirator program to ensure that all OSHA employees
are protected from exposure to respiratory hazards.
-
Inspection procedures for the Respiratory Protection Standard. OSHA
CPL 2-0.120 (1998, September 25), 10 pages. This instruction establishes
agency interpretations and enforcement policies, and provides instructions
to ensure uniform enforcement of the Respiratory Protection Standard, 29
CFR 1910.134.
- TB
Respiratory Protection Program in Health Care Facilities Administrator's Guide. Step 7: Inspect, Clean, Maintain, and Store
Respirators.
- OSHA Respiratory Protection Advisor.
- Respiratory Protection
Safety and Health Topics Page.
|
|
|
Housekeeping/Cleaning
|
Potential Hazard

|
Exposure to TB through improper housekeeping or venting procedures when cleaning TB contaminated rooms.
|
Possible Solutions
[OSHA Directive CPL 2.106
Appendix A, CDC, Supplement
5-Decontamination-Cleaning, Disinfecting, and Sterilizing (1994)] addresses cleaning practices when cleaning the room of a person
who has infectious TB.
- Normal cleaning procedures can be used, (i.e., an EPA approved germicide/disinfectant. It does not need to be tuberculocidal for
routine cleaning of a TB isolation room).
- Products are available if Tuberculocidal cleaning is desired for certain processes. The United States Environmental Protection
Agency (EPA) Office of Pesticides Program. provides lists of registered anti-microbial products at
Antimicrobial
Chemical/Registration Number Indexes.
- Personnel should follow isolation practices and wear a Class N95 or more protective respirator, while cleaning rooms of an
infectious patient.
- After the room is vacated by an infectious patient, the
precaution sign must remain posted at the
entrance to the room, and respirators must be used if entering the room, until the area is ventilated for the time necessary, using
the CDC's
recommendations, for removal efficiency of 99.9%.
- For final cleaning of the isolation room after a patient has been discharged, PPE is not necessary if the room has been ventilated
for the appropriate amount of time.
|
|
Recordkeeping
|
Potential Hazard
Exposure to TB because exposure conversion trends are not being monitored.
Possible Solutions
OSHA Recordkeeping Standards:
- If any employee has been occupationally exposed to anyone with a known case of active tuberculosis and subsequently develops a
tuberculosis infection as evidenced by a positive skin test or diagnosis by a doctor you must record the case on the
OSHA 300 log.
- Under the following circumstances the employer can line out or erase the log if evidence is obtained that the employee's TB case
was not caused by an occupational exposure:
- The worker is living in a household with a person who has been diagnosed with active TB.
- The Public Health Department has identified the worker as a contact of an individual with a case of active TB unrelated to the
workplace; or
- A medical investigation shows that the employee's infection was caused by exposure to TB away from work, or proves that the case
was not related to the workplace TB exposure.
- You do not have to record on the log a positive TB skin test result obtained at a pre-employment physical
as this exposure did not occur at your worksite.
Additional Information:
- Recordkeeping. OSHA Publication 3169.
- Recordkeeping
forms:
The OSHA Form 300, Log of Work-Related Injuries and
Illnesses has
been revised. The forms, which are required for employers to use in recording injuries and
illnesses, have changed in several important ways for 2004. The
new forms must be in use by January 1, 2004.
- New Recordkeeping
Rule Factsheet. Highlights of the OSHA Recordkeeping Rule.
- 1910.1020, Access to Employee
Exposure and medical records, (prior designation 1910.20).
|
|

