You are here:
Health Information
Related Information
- What Are Growth Plate Injuries? (fast facts, easy-to-read)
- ¿Qué son las lesiones en las placas de crecimiento? (Esenciales: hojas informativas de fácil lectura)
- Order a NIAMS Publication to be mailed
Growth Plate Injuries
PDF Version of this Document Order this publication
Publication Date: October 2001
Revised August 2007
Questions and Answers About Growth Plate Injuries
This booklet contains general information about growth plate injuries. It describes what the growth plate is, how injuries occur, and how they are treated. At the end is a list of additional resources. If you have further questions after reading this booklet, you may wish to discuss them with your doctor.
- What Is the Growth Plate?
- Who Gets Growth Plate Injuries?
- What Causes Growth Plate Injuries?
- How Are Growth Plate Fractures Diagnosed?
- What Are the Different Types of Growth Plate Injuries?
- What Kind of Doctor Treats Growth Plate Injuries?
- How Are Growth Plate Injuries Treated?
- Will the Affected Limb of a Child With a Growth Plate Injury Still Grow?
- What Are Researchers Trying To Learn About Growth Plate Injuries?
- Where Can People Find More Information About Growth Plate Injuries?
- Key Words
Information Boxes
What Is the Growth Plate?
The growth plate, also known as the epiphyseal plate or physis, is the area of growing tissue near the ends of the long bones in children and adolescents. Each long bone has at least two growth plates: one at each end. The growth plate determines the future length and shape of the mature bone. When growth is complete - sometime during adolescence - the growth plates close and are replaced by solid bone.
Because the growth plates are the weakest areas of the growing skeleton - even weaker than the nearby ligaments and tendons that connect bones to other bones and muscles - they are vulnerable to injury. Injuries to the growth plate are called fractures.
Who Gets Growth Plate Injuries?
Growth plate injuries can occur in growing children and adolescents. In a child, a serious injury to a joint is more likely to damage a growth plate than the ligaments that stabilize the joint. Trauma that would cause a sprain in an adult might cause a growth plate fracture in a child.
Growth plate fractures occur twice as often in boys as in girls, because girls’ bodies mature at an earlier age than boys. As a result, their bones finish growing sooner, and their growth plates are replaced by stronger, solid bone.
One-third of all growth plate injuries occur in competitive sports such as football, basketball, or gymnastics, while about 20 percent of growth plate fractures occur as a result of recreational activities such as biking, sledding, skiing, or skateboarding.
Fractures can result from a single traumatic event, such as a fall or automobile accident, or from chronic stress and overuse. Most growth plate fractures occur in the long bones of the fingers (phalanges) and the outer bone of the forearm (radius). They are also common in the lower bones of the leg (the tibia and fibula).
What Causes Growth Plate Injuries?
Growth plate injuries can be caused by an event such as a fall or blow to the limb, or they can result from overuse. For example, a gymnast who practices for hours on the uneven bars, a long-distance runner, and a baseball pitcher perfecting his curve ball can all have growth plate injuries.
Although many growth plate injuries are caused by accidents that occur during play or athletic activity, growth plates are also susceptible to other disorders, such as bone infection, that can alter their normal growth and development. Other possible causes of growth plate injuries include the following:
Child abuse - More than 1 million children each year are the victims of substantiated child abuse or neglect. The second most common injury among abused children is a fracture, and growth plate injuries are prevalent because the growth plate is the weakest part of the bone.
Injury from extreme cold (for example, frostbite) - Exposure to extreme cold can damage the growth plate in children and result in short, stubby fingers or premature degenerative arthritis (breakdown of the joint cartilage).
Radiation and medications - Research has suggested that chemotherapy given for childhood cancers may negatively affect bone growth. Prolonged use of steroids for inflammatory conditions such as juvenile idiopathic arthritis can also harm bone growth.
Neurological disorders - Children with certain neurological disorders that result in sensory deficit or muscular imbalance are prone to growth plate fractures, especially at the ankle and knee. Children who are born with insensitivity to pain can have similar types of injuries.
Genetics - The growth plates are where many inherited disorders that affect the musculoskeletal system appear. Scientists are just beginning to understand the genes and gene mutations involved in skeletal formation, growth, and development. This new information is raising hopes for improving treatment for children who are born with poorly formed or improperly functioning growth plates.
Metabolic disease - Disease states such as kidney failure and hormone disorders can affect the growth plates and their function. The bone growth of children with long-term conditions of this kind may be negatively affected.
Signs That Require a Visit to the Doctor
- inability to continue play because of pain following an acute or sudden injury
- decreased ability to play over the long term because of persistent pain following a previous injury
- visible malformation of the child’s arms or legs
- severe pain from acute injuries that prevent the use of an arm or leg.
Adapted from Play It Safe, a Guide to Safety for Young Athletes with permission of the American Academy of Orthopaedic Surgeons.
How Are Growth Plate Fractures Diagnosed?
A child who has persistent pain, or pain that affects athletic performance or the ability to move and put pressure on a limb, should never be allowed or expected to “work through the pain.” Whether an injury is acute or due to overuse, it should be evaluated by a doctor, because some injuries, if left untreated, can cause permanent damage and interfere with proper growth of the involved limb.
The doctor will begin the diagnostic process by asking about the injury and how it occurred and by examining the child. The doctor will then use x rays to determine if there is a fracture, and if so, the type of fracture. Often the doctor will x ray not only the injured limb but the opposite limb as well. Because growth plates have not yet hardened into solid bone, neither the structures themselves nor injuries to them show up on x rays. Instead, growth plates appear as gaps between the shaft of a long bone, called the metaphysis, and the end of the bone, called the epiphysis. By comparing x rays of the injured limb to those of the noninjured limb, doctors can look for differences that indicate an injury.
Very often the x ray is negative, because the growth plate line is already there, and the fracture is undisplaced (the two ends of the broken bone are not separated). The doctor can still diagnose a growth plate fracture on clinical grounds because of tenderness of the plate. Children do get ligament strains if their growth plates are open, and they often have undisplaced growth plate fractures.
Other tests doctors may use to diagnose a growth plate injury include magnetic resonance imaging (MRI), computed tomography (CT), and ultrasound.
Because these tests enable doctors to see the growth plate and areas of other soft tissue, they can be useful not only in detecting the presence of an injury, but also in determining the type and extent of the injury.
What Are the Different Types of Growth Plate Injuries?
Since the 1960s, the Salter-Harris classification, which divides most growth plate fractures into five categories based on the type of damage, has been the standard. The categories are as follows:
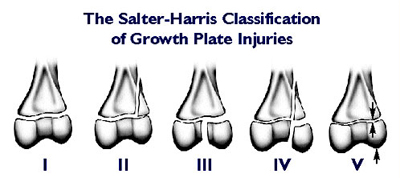
Adapted from Disorders and Injuries of the Musculoskeletal System, 3rd Edition. Robert B. Salter, Baltimore, Williams and Wilkins, 1999. Used with the author’s permission.
-
Type I
Fracture through the growth plate: The epiphysis is completely separated from the end of the bone or the metaphysis, through the deep layer of the growth plate. The growth plate remains attached to the epiphysis. The doctor has to put the fracture back into place if it is significantly displaced. Type I injuries generally require a cast to protect the plate as it heals. Unless there is damage to the blood supply to the growth plate, the likelihood that the bone will grow normally is excellent.
Type II
Fracture through the growth plate and metaphysis: This is the most common type of growth plate fracture. It runs through the growth plate and the metaphysis, but the epiphysis is not involved in the injury. Like type I fractures, type II fractures may need to be put back into place and immobilized. However, the growth plate fracture heals a great deal, especially in younger children. If it is not too displaced, the doctor may not need to put it back into position. In this case, it will strengthen with time.
Type III
Fracture through growth plate and epiphysis: This fracture occurs only rarely, usually at the lower end of the tibia, one of the long bones of the lower leg. It happens when a fracture runs completely through the epiphysis and separates part of the epiphysis and growth plate from the metaphysis. Surgery is sometimes necessary to restore the joint surface to normal. The outlook or prognosis for growth is good if the blood supply to the separated portion of the epiphysis is still intact and if the joint surface heals in a normal position.
Type IV
Fracture through growth plate, metaphysis, and epiphysis: This fracture runs through the epiphysis, across the growth plate, and into the metaphysis. Surgery is frequently needed to restore the joint surface to normal and to perfectly align the growth plate. Unless perfect alignment is achieved and maintained during healing, prognosis for growth is poor, and angulation (bending) of the bone may occur. This injury occurs most commonly at the end of the humerus (the upper arm bone) near the elbow.
Type V
Compression fracture through growth plate: This uncommon injury occurs when the end of the bone is crushed and the growth plate is compressed. It is most likely to occur at the knee or ankle. Prognosis is poor, since premature stunting of growth is almost inevitable.
A newer classification, called the Peterson classification, adds a type VI fracture, in which a portion of the epiphysis, growth plate, and metaphysis is missing. This usually occurs with open wounds or compound fractures, and often involves lawnmowers, farm machinery, snowmobiles, or gunshot wounds. All type VI fractures require surgery, and most will require later reconstructive or corrective surgery. Bone growth is almost always stunted.
What Kind of Doctor Treats Growth Plate Injuries?
For all but the simplest injuries, your child’s doctor will probably refer him or her to an orthopaedic surgeon (a doctor who specializes in bone and joint problems in children and adults) for treatment. Some problems may require the services of a pediatric orthopaedic surgeon, who specializes in injuries and musculoskeletal disorders in children.
How Are Growth Plate Injuries Treated?
Treatment for growth plate injuries depends on the type of injury. In all cases, treatment should be started as soon as possible after injury and will generally involve a mix of the following:
-
Immobilization
The affected limb is often put in a cast or splint, and the child is told to limit any activity that puts pressure on the injured area.
Manipulation or Surgery
If the fracture is displaced (meaning the ends of the injured bones no longer meet as they should), the doctor will have to put the bones or joints back in their correct positions, either by using his or her hands (called manipulation) or by performing surgery. Sometimes the doctor needs to fix the break and hold the growth plate in place with screws or wire. After the procedure, the bone will be set in place (immobilized) so it can heal without moving. This is usually done with a cast that encloses the injured growth plate and the joints on both sides of it. The cast is left in place until the injury heals, which can take anywhere from a few weeks to 2 or more months for serious injuries. The need for manipulation or surgery depends on the location and extent of the injury, its effect on nearby nerves and blood vessels, and the child’s age.
Strengthening and Range-of-Motion Exercises
These are exercises designed to strengthen the muscles that support the injured area of the bone and to improve or maintain the joint’s ability to move in the way that it should. Your child’s doctor may recommend these after the fracture has healed. A physical therapist can work with your child and his or her doctor to design an appropriate exercise plan.
Long-Term Followup
Long-term followup is usually necessary to monitor the child’s recuperation and growth. Evaluation includes x rays of matching limbs at 3- to 6-month intervals for at least 2 years. Some fractures require periodic evaluations until the child’s bones have finished growing. Sometimes a growth arrest line (a line on the x ray where the bone stopped growing temporarily) may appear as a marker of the injury. Continued bone growth away from that line may mean there will not be a long-term problem, and the doctor may decide to stop following the patient.
Will the Affected Limb of a Child With a Growth Plate Injury Still Grow?
About 85 percent of growth plate fractures heal without any lasting effect. Whether an arrest of growth occurs depends on the treatment provided, and the following factors, in descending order of importance:
- Severity of the injury - If the injury causes the blood supply to the epiphysis to be cut off, growth can be stunted. If the growth plate is shifted, shattered, or crushed, the growth plate may close prematurely, forming a bony bridge or “bar.” The risk of growth arrest is higher in this setting. An open injury in which the skin is broken carries the risk of infection, which could destroy the growth plate.
- Age of the child - In a younger child, the bones have a great deal of growing to do; therefore, growth arrest can be more serious, and closer surveillance is needed. It is also true, however, that younger bones have a greater ability to heal.
- Which growth plate is injured - Some growth plates, such as those in the region of the knee, are more involved in extensive bone growth than others.
- Type of fracture - Of the 6 fracture types described earlier, types IV, V, and VI are the most serious.
The most frequent complication of a growth plate fracture is premature arrest of bone growth. The affected bone grows less than it would have without the injury, and the resulting limb could be shorter than the opposite, uninjured limb. If only part of the growth plate is injured, growth may be lopsided and the limb may become crooked.
Growth plate injuries at the knee have the greatest risk of complications. Nerve and blood vessel damage occurs most frequently there. Injuries to the knee have a much higher incidence of premature growth arrest and crooked growth.
What Are Researchers Trying To Learn About Growth Plate Injuries?
Researchers continue to seek better ways to diagnose and treat growth plate injuries and to improve patient outcomes. Examples of such work include:
removal of a growth-blocking “bridge” or bar of bone that can form across a growth plate following a fracture. After the bridge is removed, fat, cartilage, or other materials are inserted in its place to prevent the bridge from forming again. Investigators are studying the use of cultured chondrocytes (cartilage cells grown in a dish) to replace the bridge.
use of gene therapy and/or other means to enhance the body’s production of chondrocytes. These cells are essential to growth at the ends of the bones.
research on drugs that protect the growth plate during radiation treatment. One study of animals showed that the drug amifostine1, in combination with pentoxifylline, selenium, or misoprostol, reduced the risk of limb-length discrepancies that can occur when radiation is used to treat cancer in a limb.
a study of radiologic predictors for premature closure of the growth plate following fractures. By predicting the injuries most likely to result in arrested growth, doctors could opt to treat them differently and more aggressively.
research on cancer drugs to determine which ones are likely to affect the growth plates. One recent study, for example, showed that in rats the chemotherapy agent doxorubicin affected the growth plate of the tibia at the knee while two other agents, methotrexate and cisplatin, did not.
development of methods to regenerate musculoskeletal tissue by using principles of tissue engineering.
NIAMS currently funds Core Centers for Musculoskeletal Disorders at major medical centers. These centers provide the resources for established, currently funded investigators who are often from different disciplines, to adopt a multidisciplinary approach to common research problems in musculoskeletal disorders.
The centers foster research to better understand the mechanisms of bone repair and regeneration, including fracture healing and development of techniques for growth plate repair.
1 Brand names included in this booklet are provided as examples only, and their inclusion does not mean that these products are endorsed by the National Institutes of Health or any other Government agency. Also, if a particular brand name is not mentioned, this does not mean or imply that the product is unsatisfactory.
Where Can People Find More Information About Growth Plate Injuries?
-
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Information Clearinghouse
National Institutes of Health1 AMS Circle
Bethesda, MD 20892-3675
Phone: 301-495-4484
Toll Free: 877-22-NIAMS (226-4267)
TTY: 301–565–2966
Fax: 301-718-6366
Email: NIAMSinfo@mail.nih.gov
Website: http://www.niams.nih.govNIAMS provides information on arthritis and rheumatic disease and bone, muscle, joint, and skin diseases. It distributes patient and professional education materials and refers people to other sources of information. Additional information and updates can also be found on the NIAMS Web site.
-
American Academy of Orthopaedic Surgeons (AAOS)
P.O. Box 2058
Des Plaines, IL 60017
Toll Free: 800-824-BONE (2663)
Email: pemr@aaos.org
Website: http://www.aaos.orgThe academy provides education and practice management services for orthopaedic surgeons and allied health professionals. It also serves as an advocate for improved patient care and informs the public about the science of orthopaedics. The orthopaedist's scope of practice includes disorders of the body's bones, joints, ligaments, muscles, and tendons. For a single copy of an AAOS brochure, send a self-addressed stamped envelope to the address above or visit the AAOS Web site.
-
American Academy of Pediatrics
141 Northwest Point Boulevard
Elk Grove Village, IL 60007-1098
Phone: 847-434-4000
Fax: 847-434-8000
Website: http://www.aap.orgThe American Academy of Pediatrics (AAP) and its member pediatricians dedicate their efforts and resources to the health, safety, and well-being of infants, children, adolescents, and young adults. Activities of the AAP include advocacy for children and youth, public education, research, professional education, and membership service and advocacy for pediatricians.
-
American Orthopaedic Society for Sports Medicine (AOSSM)
6300 N. River Road, Suite 500
Rosemont, IL 60018
Phone: 847-292-4900
Fax: 847-292-4905
Email: aossm@aossm.org
Website: http://www.sportsmed.orgThe society is an organization of orthopaedic surgeons and allied health professionals dedicated to educating health care professionals and the general public about sports medicine. It promotes and supports educational and research programs in sports medicine, including those concerned with fitness, as well as programs designed to advance knowledge of the recognition, treatment, rehabilitation, and prevention of athletic injuries.
Key Words
Computed (or computerized) tomography (CT) scan - An imaging technique that provides doctors with a threedimensional picture of the bone. It also shows “slices” of the bone, making the picture much clearer than x rays.
Displaced fracture - A fracture in which the two ends of the broken bone are separated from one another.
Epiphyseal plate - The area of developing tissue near the end of the long bones in children and adolescents. It is also called the physis or growth plate.
Epiphysis - The end of a long bone, which is initially separated by cartilage from the shaft of the bone and develops separately. It eventually fuses with the shaft (diaphysis) of the bone to form a complete bone.
Femur - The thigh bone.
Fibula - The long, thin outer bone of the lower leg.
Growth plate - The area of developing tissue near the end of the long bones in children and adolescents. Each long bone has at least two growth plates: one at each end. The growth plate determines the future length and shape of the mature bone. When growth is complete - sometime during adolescence - the growth plates are replaced by solid bone. The growth plate is also called the physis or epiphyseal plate.
Humerus - The bone of the upper arm.
Ligaments - Tough bands of connective tissue that connect bones.
Metaphysis - The growing portion of a long bone that lies between the ends of the bones (epiphyses) and the shaft (diaphysis).
Magnetic resonance imaging (MRI) - A procedure in which a strong magnet is used to pass a force through the body, resulting in a clear, detailed, cross-sectional image. Unlike standard x rays, it can show soft tissue as well as bone and thus is useful in diagnosing injuries to the growth plates.
Neurological - Having to do with the nervous system (made up of the brain, spinal cord and peripheral nerves), this system of tissues uses electrical and chemical means to record and distribute information within the body.
Orthopaedic surgeon - A physician who specializes in treating (through surgery, casting, or other means) abnormalities of or injuries to the bones.
Physis - The area of developing tissue near the end of the long bones in children and adolescents. The physis is also called the growth plate.
Radius - The smaller of the two bones of the forearm. It is located on the thumb side of the arm.
Tendons - Tough but flexible bands of tissue that connect muscles to bones.
Tibia - The larger of the two bones that make up the lower leg. It is also referred to as the shin bone.
Ultrasound - A technique that allows doctors to view the soft tissues of the body by bouncing sound waves off the tissue and then converting the echoes into a picture called a sonogram.
Acknowledgments
NIAMS gratefully acknowledges the assistance of James S. Panagis, M.D., M.P.H., NIAMS, NIH; R. Tracy Ballock, M.D., Case Western Reserve University, Cleveland, OH; Michael G. Ehrlich, M.D., Brown University, Providence, RI; Ryan Goodwin, M.D., Cleveland Clinic, Cleveland, OH; and Robert B. Salter, M.D., Hospital for Sick Children, Toronto, Ontario, Canada, in the preparation and review of this booklet. NIAMS also acknowledges the American Academy of Orthopaedic Surgeons for the use of its publication, Skeletal Growth and Development: Clinical Issues and Basic Science Advances.
The mission of the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), a part of the Department of Health and Human Services’ National Institutes of Health (NIH), is to support research into the causes, treatment, and prevention of arthritis and musculoskeletal and skin diseases; the training of basic and clinical scientists to carry out this research; and the dissemination of information on research progress in these diseases. The National Institute of Arthritis and Musculoskeletal and Skin Diseases Information Clearinghouse is a public service sponsored by the NIAMS that provides health information and information sources. Additional information can be found on the NIAMS Web site at www.niams.nih.gov.
For Your Information
This publication contains information about medications used to treat the health condition discussed here. When this booklet was printed, we included the most up-to-date (accurate) information available. Occasionally, new information on medication is released.
For updates and for any questions about any medications you are taking, please contact the U.S. Food and Drug Administration at 1-888-INFO-FDA (1-888-463-6332, a toll-free call) or visit their Web site at www.fda.gov.
This booklet is not copyrighted. Readers are encouraged to duplicate and distribute as many copies as needed.
Additional copies of this booklet are available from
-
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Information Clearinghouse
National Institutes of Health1 AMS Circle
Bethesda, MD 20892-3675
Phone: 301-495-4484
Toll Free: 877-22-NIAMS (226-4267)
TTY: 301–565–2966
Fax: 301-718-6366
Email: NIAMSinfo@mail.nih.gov
Website: http://www.niams.nih.gov