|
Developing Effective and Efficient Treatments
Approximately one third of all cancers are avoidable through lifestyle changes. These changes include: stopping
smoking, maintaining a healthy weight, being physically active, eating a moderate-fat diet with enough fruits and
vegetables, avoiding too much alcohol, and protecting the skin from harmful sun exposure. Enough information is
also available to permit the early detection and effective treatment of another one third of cancer cases. Some of
the most commonly occurring cancer types are curable with existing treatments. Nonetheless, millions of cancer
cases worldwide cannot currently be prevented or cured. Therefore, we must continue to develop new and
effective treatments.
Developing new therapies for cancer is central to much of the research supported by NCI. By partnering with
research institutions and investigators around the world, we should be able to accelerate the pace of development
of new drugs and other treatments and shorten the time required to recruit patients into and complete clinical trials.
In Europe, NCI created a liaison office to coordinate many of its research and treatment programs conducted
with European collaborators (see article on the
NCI Liaison Office). More examples of global
NCI-supported programs and efforts to develop new, effective, and efficient treatments for cancer are described
in this section.
NCI is assisting international research institutions with clinical trial investigations of targeted
radiation therapy - also known as radioimmunotherapy - by supplying overseas scientists
with the necessary reagents and expertise pertaining to their use. One clinical trial
that is currently being conducted at the German Cancer Research Center in Heidelberg,
Germany is evaluating a monoclonal antibody conjugated to the radioisotope bismuth-213
for the treatment of NHL. The monoclonal antibody targets a protein antigen called
CD20, which is found on NHL cells. The German researchers obtained the reagents they
needed for this trial from NCI through a Material Transfer Agreement with the Institute.
The NCI supports research projects at several Canadian universities, cancer centers, and
hospitals, as well as clinical trials run by Canadian cooperative groups. One group that
receives NCI support is the Princess Margaret Hospital Phase II Consortium. This consortium
is the only non-U.S.-based trial group funded by NCI to carry out Phase II studies of
new anticancer drugs. In addition, the National Cancer Institute of Canada is a participant
in the NCI Clinical Trials Cooperative Group Program. Individual Canadian institutions
are also members of other NCI-supported cooperative groups, including the
American College of Surgeons Oncology Group, the Cancer and Leukemia Group B, the
Children's Oncology Group, the Eastern Cooperative Oncology Group, the Gynecologic
Oncology Group, the National Surgical Adjuvant Breast and Bowel Project, the North
Central Cancer Treatment Group, the Radiation Therapy Oncology Group, and the
Southwest Oncology Group. More than 90 percent of the investigational drugs shipped
internationally by NCI's Cancer Therapy Evaluation Program (CTEP) currently go to
Canadian investigators (see related article on CTEP).
Routine, complete lymphadenectomy - the surgical removal of regional lymph nodes -
for patients with clinically localized primary melanoma remains controversial because
most patients will have tumor-free nodes. A minimally-invasive procedure called intraoperative
lymphatic mapping and biopsy of the sentinel lymph node is a promising alternative.
Examination of the sentinel lymph node - defined as the regional node most likely
to contain cancer cells spreading from the primary tumor - can identify patients with
occult (microscopic) metastasis. These patients should undergo complete lymphadenectomy,
while other patients do not require further nodal assessment.
The Multicenter Selective Lymphadenectomy Trial (MSLT-I), headed by investigators from
the John Wayne Cancer Institute in Santa Monica, California, is comparing two treatments
for early melanoma: 1) wide excision plus sentinel node biopsy (SNB), followed
immediately by complete lymphadenectomy if the sentinel node contains cancer; and
2) wide excision, followed by complete lymphadenectomy only for clinical evidence of
nodal metastasis during postoperative observation.
MSLT-I, the largest randomized surgical trial for melanoma, enrolled 338 patients from
North America, 630 from Europe, and 1,033 from Australia. International enrollment
allowed rapid accrual. Interim results, which were reported in 2005, showed that SNB
performed by doctors with adequate training and experience can identify occult nodal
metastases with 95 to 97 percent accuracy. The interim data also indicate that SNB significantly
lengthens the disease-free survival of all patients and prolongs the overall survival
of patients with occult nodal metastases.
Because these findings strongly support early lymphadenectomy for occult nodal metastasis,
MSLT-I data are changing the standard of care. A follow-up study, MSLT-II, is now
open to patient accrual and will enroll at least 1,925 patients in another international
collaboration of melanoma centers.
|
| Scanning Electron
Microscope Picture of
a Breast Cancer Cell |
An international clinical trial led by the National Cancer Institute of
Canada Clinical Trials Group (NCIC CTG), with support from the
Canadian Cancer Society (CCS), and in partnership with NCI and
Novartis Pharmaceuticals, showed that the estrogen-suppressing
drug letrozole (Femara®) reduced the risk of breast cancer recurrence
and the incidence of new breast cancer in the opposite breast by
42 percent compared to placebo in women whose tumors were
hormone receptor-positive.
Previous studies had shown that 5 years of treatment with the drug tamoxifen after
surgery, radiation therapy, and chemotherapy for early-stage breast cancer could reduce
the risk of recurrence by almost half in women whose tumors were estrogen receptorpositive.
Some of these studies also showed, however, that no additional benefit is
obtained by continuing tamoxifen treatment beyond 5 years. Because more than
50 percent of the women who experience a recurrence of their cancer do so more than
5 years after diagnosis, additional treatment options are necessary. This trial showed
that a 5-year course of letrozole, when given after 5 years of tamoxifen therapy,
significantly reduced the risk of local recurrence and metastasis (distant recurrence).
In addition to patients recruited through the NCIC CTG and NCI, European participants
were enrolled in the letrozole study by the European Organization for Research and
Treatment of Cancer (EORTC) and the International Breast Cancer Study Group
(IBCSG). Participants in the trial were enrolled through hospitals, cancer centers, and
institutes throughout Canada, the United States, England, Belgium, Ireland, Italy, Poland,
Portugal, and Switzerland. The trial's participants will continue to be followed for 10 to
15 years.

|
| NCI Frederick Cancer
Research and
Development Facility
Prepares Samples of
Natural Substances
for Chemical Analysis |
Between 1986 and 2004, NCI's Developmental Therapeutics Program
(DTP) acquired plants and continues to collect marine organisms to
screen for potential anticancer compounds through collection agreements
with over 25 tropical and subtropical countries. More than
50,000 plant specimens were collected in Africa and Madagascar,
Central and South America, and Southeast Asia. More than 13,000
specimens of marine invertebrates and marine algae have been collected
to date, initially from the Indo-Pacific region, and, since 2002,
from areas worldwide.
In undertaking these collections, NCI committed itself to the conservation
of biological diversity, as well as to policies of fair and equitable
collaboration and compensation in interacting with the source countries
participating in the collection programs. Agreements based on the
NCI Letter of Collection (LOC) or Memoranda of Understanding
(MOUs) have been signed with relevant government organizations in
many of the source countries. The first such agreement was signed with Madagascar in
1990, 3 years before an international conference in Rio de Janeiro, Brazil, that led to the
signing of the Convention on Biodiversity (CBD). In addition, the NCI model agreements
have formed the basis for many international accords not involving the Institute or the
United States and are still used as a basis for discussion by many organizations wishing
to conduct biodiscovery programs.
More information about DTP's international outreach initiatives is found
in NCI's Developmental Therapeutics Program.
|
Since its inception, NCI's Cancer Therapy Evaluation Program (CTEP) has provided promising anticancer drugs to
international researchers for both preclinical and clinical studies. In 2004 alone, new investigational drugs were
shipped to, among others, Australia, Canada, China, Germany, Hong Kong, Peru, and the United Kingdom for clinical
trials, special exceptions ("compassionate use") treatment, and laboratory research.
Most drugs are provided under CTEP to investigators who are collaborating on NCI-sponsored clinical trials led by
investigators in the United States. International participation in clinical trials allows for increased patient accrual,
more rapid trial completion, and access to patients with cancers that may be rare in the United States. For studies
led by foreign investigators, both the trial concept and protocol are reviewed in detail by NCI before an agreement
is reached.
Requests to CTEP for "compassionate use" access to experimental drugs are reviewed on a patient-by-patient basis,
and all approved patients must meet the same eligibility criteria as patients in the United States.
Currently, NCI is also providing investigational new drugs developed by CTEP to foreign investigator-led trials in both
Europe and Asia. Three trials in the United Kingdom, sponsored by Cancer Research U.K., are testing the investigational
compounds provided by CTEP. In addition, CTEP is providing experimental drugs for several trials conducted by
the Cancer Therapeutics Research Group in the Far East, comprised of investigators in Hong Kong, Singapore, Korea,
and Australia.
Many existing collaborative relationships under CTEP are the result of NCI's strong training programs, which invite
international scientists to study at NCI and take what they have learned back to their home countries (see
NCI's Visiting Scientist Programs).
These investigators often choose to maintain the professional relationships developed during their time at NCI, and
they become active participants in international studies.
In addition, many NCI-sponsored Clinical Trials Cooperative Groups that use investigational new drugs developed by
CTEP have international investigators as members. Such groups include the National Surgical Adjuvant Breast and
Bowel Project, the Eastern Cooperative Oncology Group, and the Children's Oncology Group.
|

|
| Three Strains of Mice
Used in Experiments |
NCI is collaborating with investigators at the
Peter McCollum Cancer Centre in Melbourne,
Australia and Juntendo University in Tokyo,
Japan to explore combination treatment of
a number of mouse tumor types with bortezomib
(Velcade®) and an agonist antibody
against the Apo2L/TRAIL "death receptor."
As part of the collaboration, the Australian
and Japanese investigators have supplied NCI
with a quantity of the purified antibody and
with lymphocyte - tumor hybrid cells called
"hybridomas" that produce it.
The Apo2L/TRAIL receptor is one of several members of the tumor necrosis factor
superfamily of receptors that are able to induce apoptosis (programmed cell death)
when activated. This receptor has received considerable attention lately because of the
finding that many cancer cell types are sensitive to Apo2L/TRAIL-induced apoptosis,
whereas most normal cells are not.
Bortezomib works by blocking the action of structures inside cells called "proteasomes,"
which are large enzyme complexes that degrade abnormal or misfolded proteins and
proteins that are normally targeted for destruction. Some proteins are normally targeted
for orderly destruction to maintain cellular growth control. Research has shown that
proteasome inhibition can induce apoptosis and that cancer cells are more sensitive to
this effect of bortezomib than normal cells.
The antibody against the Apo2L/TRAIL receptor alone has shown some efficacy against
tumor cells, but preliminary experiments have indicated that bortezomib enhances its
activity. This combination treatment will hopefully allow a reduction of tumor burden in
the absence of the major immunosuppression that can occur during traditional chemotherapy
or radiation therapy. The investigators' aims are to promote local tumor destruction
and, hopefully, to improve the natural immune response against the tumor cells.
|
Since 1955, NCI's Developmental Therapeutics Program (DTP), part of the Division of Cancer Treatment and Diagnosis,
has been tasked with planning, conducting, and facilitating the discovery and development of new therapeutic agents
for cancer.
One service of DTP that is open to investigators throughout the world is a screening program that can test new
compounds for anticancer activity both in the "test tube" (in vitro) and in animal models (in vivo). Among the more
than 24,000 compounds accepted for screening by DTP since the beginning of 2000, approximately 64 percent came
from international institutions.
For many years, DTP has also formally collaborated in drug development with the European Organization for Research
and Treatment of Cancer, Cancer Research U.K., and the Southern Europe New Drug Organization in Italy.
For example, DTP's Pharmaceutical Resources Branch and Toxicology and Pharmacology Branch have participated in
the formulation and evaluation of the pharmacokinetics and toxicity of benzothiazole and its analogs to determine the
suitability of these compounds for testing in early clinical trials. DTP also carried out the formulation, development,
and production of clomesone, bryostatin, rhizoxin, and SJG-136, which had their initial clinical evaluations in Europe.
A number of anticancer agents in development by DTP originally came from Japan. One of these, a benzoylphenylurea
produced by a Japanese chemical company, involved very active joint research in which the company provided
a number of prodrugs to NCI. Prodrugs are inactive compounds that the body can metabolize to become active drugs.
In addition to collaborations with larger organizations, DTP works directly with investigators in Europe and Japan
who have expertise in the selection of candidate agents for screening. Current projects include the development
of benzothiazoles and pyrrolobenzodiazepines (United Kingdom) and aminoflavone derivatives (Japan). These
compounds are currently in early clinical trials in those countries.
|
Following a successful pilot study, NCI is supporting a cooperative agreement to develop
an ICTCM that partners the University of Texas M. D. Anderson Cancer Center with
the Cancer Hospital, Fudan University in Shanghai, China. Researchers affiliated with
the center will investigate the benefits of some traditional Chinese medicine (TCM)
treatments for cancer patients.
During the 2-year pilot study, which began in 2003, the ICTCM investigated three
categories of TCM: 1) herbal and natural treatments that target the disease and related
symptoms; 2) acupuncture for some side effects of cancer treatment; and 3) the biobehavioral
effects of qigong, a self-healing art that combines movement and meditation, and
other mind/body interventions. This work is being advanced further under a new 4-year
cooperative agreement.
While the NCI has supported research in individual topics related to TCM, such as
acupuncture, these are the first NCI grants to support the development of an international
partnership to study multiple aspects of TCM.
|
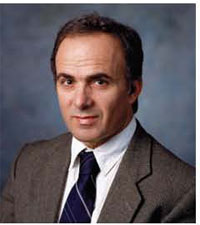
| Dr. Yosef Yarden |
NCI has named Dr. Yosef Yarden of the Weizmann Institute of Science in Rehovot,
Israel as a MERIT Award recipient for his project titled "Next Generation Strategies to
Intercept ErbB Signaling." The MERIT Awards were established to provide experienced
investigators with long-term, stable support to foster their continued creativity.
Dr. Yarden is investigating the epidermal growth factor receptor (EGFR/ErbB) family of
proteins with the goal of designing therapies that inhibit their oncogenic properties. He has
been involved in many crucial developments in this field, including isolating EGFR/ErbB-1,
identifying several proteins that bind to EGFR/ErbB-1, and understanding the role of another
member of the EGFR family (HER2/ErbB-2) in cell signaling and tumor development.
In his MERIT-funded research, Dr. Yarden will focus on developing therapies that target
ErbB. This work will be carried out through development of: 1) novel molecules that bind
EGFR/ErbB receptors; 2) engineered soluble portions of these receptors; and 3) inhibitors
of EGFR/ErbB receptor activation that promote receptor degradation. Immunotherapy
strategies will also be explored.
|
The NCI Liaison Office, located in Brussels, Belgium, coordinates several of the Institute's research and treatment
programs in Europe through formal agreements with organizations such as the European Organization for Research
and Treatment of Cancer (EORTC), Cancer Research U.K. (CRUK), and the Southern Europe New Drugs Organization
(SENDO). Additional Liaison Office activities involve less formal interactions with other European cancer research
organizations, institutes, laboratories, and pharmaceutical/chemical corporations.
The primary goal of the Liaison Office is to foster exchanges of information, experimental drugs, research protocols,
scientists, and scientific expertise between NCI and its European collaborators. The Liaison Office participates in
numerous European committees and working groups involved in new drug development. It also provides representation
to the EORTC Board and Council and the CRUK Phase I/II clinical trials committee. In addition, the Office has
observer status with the European Drug Development Network (EDDN) and supports an international exchange of
experimental drugs for preclinical and clinical evaluation.
The NCI Liaison Office also collects European cancer clinical research protocols and coordinates their inclusion in
NCI's Physician Data Query (PDQ®) cancer information database, the contents of which are made available worldwide
through various channels (see description of PDQ®).
A collaborative relationship has also been established between the Liaison Office and the International Network
for Cancer Treatment and Research (INCTR), which is also based in Brussels (for more information on
INCTR,
see International Network for Cancer Treatment and Research).
Finally, the Liaison Office serves as the European hub for the TELESYNERGY® Medical Consultation WorkStation,
which was developed by the National Institutes of Health's Center for Information Technology and is deployed by
NCI. TELESYNERGY® is an integrated telecommunications system of computers, microscopes, cameras, and other
equipment that can transmit X-rays and other medical images or a live examination of a patient to distant sites,
where clinicians can discuss the case as if they were in the same room (see more about this program).
|
The AIDS Malignancy Consortium (AMC) is an NCI-supported clinical trials group
founded in 1995 to support innovative trials for AIDS-associated malignancies, including
non-Hodgkin lymphoma, primary central nervous system lymphoma, Kaposi sarcoma,
and cervical cancer. The International Working Group of the AMC - one of five AMC
working groups - is focused on developing partnerships with international investigators
to pursue non-myelosuppressive, hypothesis-driven clinical trials for AIDS-associated
malignancies that are suitable for evaluation in resource-poor settings.
In one such clinical trial, researchers with the East Africa-Case Western Reserve
University Research Collaboration confirmed that dose-modification of oral chemotherapy
in the management of AIDS-related non-Hodgkin lymphoma results in less toxicity
and does not compromise efficacy. Future AMC clinical trials will include international
sites in areas most affected by the global AIDS pandemic, such as Uganda, Zambia,
Kenya, Tanzania, and Brazil.
Back to Top
< Previous Section | Next Section > |