Introduction
The Skin
Understanding Skin Cancer
Risk Factors
Prevention
Symptoms
Diagnosis
Staging
Treatment
Follow-up Care
Sources of Support
The Promise of Cancer Research
How To Do a Skin Self-Exam
National Cancer Institute Information Resources
National Cancer Institute Publications
Introduction
This National Cancer Institute (NCI) booklet has important information about
skin
cancer.*
Skin cancer is the most common type of cancer in this country.
About one million Americans develop skin cancer each year.
You will read about causes and ways to prevent skin cancer. You will find
information about symptoms, diagnosis, and treatment. You will also learn how
to do a skin self-exam.
Scientists are studying skin cancer to find out more about how it develops. And
they are looking for better ways to prevent and treat it.
|
There are many types of skin cancer. This booklet is about the two most common
types, basal cell cancer and squamous cell cancer. These are sometimes called
nonmelanoma skin cancer. A much less common type of skin cancer, melanoma, is
not discussed in this booklet. To learn about this disease, see the NCI booklet
What You Need To Know About Melanoma 1.
|
NCI provides information about cancer, including the publications mentioned in
this booklet. You can order these materials by telephone or on the Internet.
You can also read them on the Internet and print your own copy.
-
Telephone (1-800-4-CANCER): Information Specialists at NCI's Cancer
Information Service can answer your questions about cancer. They also can send
NCI booklets, fact sheets, and other materials.
-
Internet (http://www.cancer.gov): You can use NCI's Web
site to find a wide range of up-to-date information. For example, you can find
many NCI booklets and fact sheets at http://www.cancer.gov/publications. People in the United States and
its territories may use this Web site to order printed copies. This Web site
also explains how people outside the United States can mail or fax their
requests for NCI booklets.
You can ask questions online and get help right away from Information
Specialists through
LiveHelp 2 at http://www.cancer.gov/cis.
*Words that may be new to readers appear in italics. The "Dictionary 3"
section explains these terms. Some words in the "Dictionary" have a
"sounds-like" spelling to show how to pronounce them.
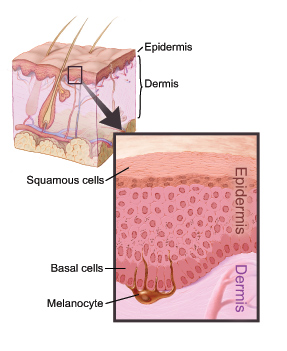
The Skin
The skin is the body's largest
organ.
It protects against heat, light, injury,
and
infection.
It helps control body temperature. It stores water and fat. The
skin also makes vitamin D.
The skin has two main layers:
-
Epidermis:
The epidermis is the top layer of the skin. It is mostly made
of flat
cells.
These are
squamous cells.
Under the squamous cells in the
deepest part of the epidermis are round cells called
basal cells.
Cells called
melanocytes
make the pigment (color) found in skin and are located in the lower
part of the epidermis.
-
Dermis:
The dermis is under the epidermis. It contains blood vessels,
lymph
vessels, and
glands.
Some of these glands make sweat, which helps cool
the body. Other glands make
sebum.
Sebum is an oily substance that helps keep
the skin from drying out. Sweat and sebum reach the surface of the skin through
tiny openings called pores.
|
| This picture shows the layers of the skin. |
Understanding Skin Cancer
Skin cancer begins in cells, the building blocks that make up the skin.
Normally, skin cells grow and divide to form new cells. Every day skin cells
grow old and die, and new cells take their place.
Sometimes, this orderly process goes wrong. New cells form when the skin does
not need them, and old cells do not die when they should. These extra cells can
form a mass of
tissue
called a growth or
tumor.
Growths or tumors can be
benign
or
malignant:
-
Benign growths are not cancer:
-
Benign growths are rarely life-threatening.
-
Generally, benign growths can be removed. They usually do not grow back.
-
Cells from benign growths do not invade the tissues around them.
-
Cells from benign growths do not spread to other parts of the body.
-
Malignant growths are cancer:
-
Malignant growths are generally more serious than benign growths. They may be
life-threatening. However, the two most common types of skin cancer cause only
about one out of every thousand deaths from cancer.
-
Malignant growths often can be removed. But sometimes they grow back.
-
Cells from malignant growths can invade and damage nearby tissues and organs.
-
Cells from some malignant growths can spread to other parts of the body. The
spread of cancer is called
metastasis.
Skin cancers are named for the type of cells that become cancerous.
The two most common types of skin cancer are
basal cell cancer
and
squamous cell cancer.
These cancers usually form on the head, face, neck, hands, and
arms. These areas are exposed to the sun. But skin cancer can occur anywhere.
-
Basal cell skin cancer grows slowly. It usually occurs on areas of the
skin that have been in the sun. It is most common on the face. Basal cell
cancer rarely spreads to other parts of the body.
-
Squamous cell skin cancer also occurs on parts of the skin that have
been in the sun. But it also may be in places that are not in the sun. Squamous
cell cancer sometimes spreads to
lymph nodes
and organs inside the body.
If skin cancer spreads from its original place to another part of the body, the
new growth has the same kind of abnormal cells and the same name as the
primary growth.
It is still called skin cancer.
Risk Factors
Doctors cannot explain why one person develops skin cancer and another does
not. However, we do know that skin cancer is not contagious. You cannot "catch"
it from another person.
Research has shown that people with certain
risk factors
are more likely than
others to develop skin cancer. A risk factor is something that may increase the
chance of developing a disease.
Studies have found the following risk factors for skin cancer:
-
Ultraviolet (UV) radiation: UV radiation comes from the sun, sunlamps,
tanning beds, or tanning booths. A person's risk of skin cancer is related to
lifetime exposure to UV radiation. Most skin cancer appears after age 50, but
the sun damages the skin from an early age.
UV radiation affects everyone. But people who have fair skin that freckles or
burns easily are at greater risk. These people often also have red or blond
hair and light-colored eyes. But even people who tan can get skin cancer.
People who live in areas that get high levels of UV radiation have a higher
risk of skin cancer. In the United States, areas in the south (such as Texas
and Florida) get more UV radiation than areas in the north (such as Minnesota).
Also, people who live in the mountains get high levels of UV radiation.
UV radiation is present even in cold weather or on a cloudy day.
-
Scars or burns on the skin
-
Infection with certain
human papillomaviruses
-
Exposure to arsenic at work
-
Chronic
skin
inflammation
or skin
ulcers
-
Diseases that make the skin sensitive to the sun, such as
xeroderma pigmentosum,
albinism,
and
basal cell nevus syndrome
-
Radiation therapy
-
Medical conditions or drugs that suppress the
immune system
-
Personal history of one or more skin cancers
-
Family history of skin cancer
-
Actinic keratosis:
Actinic keratosis is a type of flat, scaly growth on
the skin. It is most often found on areas exposed to the sun, especially the
face and the backs of the hands. The growths may appear as rough red or brown
patches on the skin. They may also appear as cracking or peeling of the lower
lip that does not heal.
Without treatment, a small number of these scaly growths may turn into squamous
cell cancer.
-
Bowen's disease: Bowen's disease is a type of scaly or thickened patch
on the skin. It may turn into squamous cell skin cancer.
If you think you may be at risk for skin cancer, you should discuss this
concern with your doctor. Your doctor may be able to suggest ways to reduce
your risk and can plan a schedule for checkups.
 |
Prevention
The best way to prevent skin cancer is to protect yourself from the sun. Also,
protect children from an early age. Doctors suggest that people of all ages
limit their time in the sun and avoid other sources of UV radiation:
-
It is best to stay out of the midday sun (from mid-morning to late afternoon)
whenever you can. You also should protect yourself from UV radiation reflected
by sand, water, snow, and ice. UV radiation can go through light clothing,
windshields, windows, and clouds.
-
Wear long sleeves and long pants of tightly woven fabrics, a hat with a wide
brim, and sunglasses that absorb UV.
-
Use
sunscreen
lotions. Sunscreen may help prevent skin cancer, especially
broad-spectrum sunscreen (to filter
UVB
and
UVA
rays) with a
sun protection factor (SPF) of at least 15. But you still need to avoid the sun and wear
clothing to protect your skin.
-
Stay away from sunlamps and tanning booths.
Symptoms
Most basal cell and squamous cell skin cancers can be cured if found and treated early.
A change on the skin is the most common sign of skin cancer. This may be a new growth, a sore that doesn't heal, or a change in an old growth. Not all skin cancers look the same. Skin changes to watch for:

- Small, smooth, shiny, pale, or waxy lump

- Firm, red lump
- Sore or lump that bleeds or develops a crust or a scab

- Flat red spot that is rough, dry, or scaly and may become itchy or tender

- Red or brown patch that is rough and scaly
Sometimes skin cancer is painful, but usually it is not.
Checking your skin for new growths or other changes is a good idea. A guide for checking your skin is below 4. Keep in mind that changes are not a sure sign of skin cancer. Still, you should report any changes to your health care provider right away. You may need to see a
dermatologist, a doctor who has special training in the diagnosis and treatment of skin problems.
Diagnosis
If you have a change on the skin, the doctor must find out whether it is due to
cancer or to some other cause. Your doctor removes all or part of the area that
does not look normal. The sample goes to a lab. A
pathologist
checks the sample
under a microscope. This is a
biopsy.
A biopsy is the only sure way to diagnose
skin cancer.
You may have the biopsy in a doctor's office or as an
outpatient in a clinic or hospital. Where it is done depends on the size and
place of the abnormal area on your skin. You probably will have
local anesthesia.
There are four common types of skin biopsies:
-
Punch biopsy:
The doctor uses a sharp, hollow tool to remove a circle of
tissue from the abnormal area.
-
Incisional biopsy:
The doctor uses a
scalpel
to remove part of the
growth.
-
Excisional biopsy:
The doctor uses a scalpel to remove the entire growth
and some tissue around it.
-
Shave biopsy:
The doctor uses a thin, sharp blade to shave off the
abnormal growth.
You may want to ask your doctor these questions before having a biopsy:
-
Which type of biopsy do you recommend for me?
-
How will the biopsy be done?
-
Will I have to go to the hospital?
-
How long will it take? Will I be awake? Will it hurt?
-
Are there any risks? What are the chances of infection or bleeding after the
biopsy?
-
What will my scar look like?
-
How soon will I know the results? Who will explain them to me?
|
Staging
If the biopsy shows that you have cancer, your doctor needs to know the extent
(stage)
of the disease. In very few cases, the doctor may check your lymph
nodes to stage the cancer.
The stage is based on:
-
The size of the growth
-
How deeply it has grown beneath the top layer of skin
-
Whether it has spread to nearby lymph nodes or to other parts of the body
These are the stages of skin cancer:
-
Stage 0: The cancer involves only the top layer of skin. It is
carcinoma in situ.
-
Stage I: The growth is 2 centimeters wide (three-quarters of an inch) or
smaller.
-
Stage II: The growth is larger than 2 centimeters wide (three-quarters
of an inch).
-
Stage III: The cancer has spread below the skin to
cartilage,
muscle,
bone, or to nearby lymph nodes. It has not spread to other places in the body.
-
Stage IV: The cancer has spread to other places in the body.
Treatment
Sometimes all of the cancer is removed during the biopsy. In such cases, no
more treatment is needed. If you do need more treatment, your doctor will
describe your options.
Treatment for skin cancer depends on the type and stage of the disease, the
size and place of the growth, and your general health and medical history. In
most cases, the aim of treatment is to remove or destroy the cancer completely.
It often helps to make a list of questions before an appointment. To help
remember what the doctor says, you may take notes or ask whether you may use a
tape recorder. You may also want to have a family member or friend with you
when you talk to the doctor -- to take part in the discussion, to take notes, or
just to listen.
Your doctor may refer you to a specialist, or you may ask for a referral.
Specialists who treat skin cancer include
dermatologists,
surgeons, and
radiation oncologists.
Before you have treatment, you might want a second opinion about the diagnosis
and treatment plan. Many insurance companies cover a second opinion if you or
your doctor requests it. It may take some time and effort to gather medical
records and arrange to see another doctor. Usually it is not a problem to take
several weeks to get a second opinion. In most cases, the delay will not make
treatment less effective. To make sure, you should discuss this delay with your
doctor. Sometimes people with skin cancer need treatment right away.
There are a number of ways to find a doctor for a second opinion:
-
Your doctor may refer you to one or more specialists. At cancer centers,
several specialists often work together as a team.
-
NCI's Cancer Information Service, at 1-800-4-CANCER, can tell you about nearby
treatment centers. Information Specialists also can provide online assistance
through
LiveHelp 2 at http://www.cancer.gov/cis.
-
A local or state medical society, a nearby hospital, or a medical school can
usually provide the names of specialists.
-
The American Board of Medical Specialties (ABMS) has a list of doctors who have
had training and passed exams in their specialty. You can find this list in the
Official ABMS Directory of Board Certified Medical Specialists. This Directory
is in most public libraries. Also, ABMS offers this information at
http://www.abms.org 5. (Click on "Who's Certified.")
-
NCI provides a helpful fact sheet called "How To Find a Doctor or Treatment
Facility If You Have Cancer 6."
|
You may want to ask the doctor these questions before treatment begins:
-
What is the stage of the disease?
-
What are my treatment choices? Which do you recommend for me? Why?
-
What are the expected benefits of each kind of treatment?
-
What are the risks and possible
side effects
of each treatment? What can we do
to control my side effects?
-
Will the treatment affect my appearance? If so, can a
reconstructive surgeon
or
plastic surgeon
help?
-
Will treatment affect my normal activities? If so, for how long?
-
What is the treatment likely to cost? Does my insurance cover this treatment?
-
How often should I have checkups?
-
Would a
clinical trial
(research study) be appropriate for me?
|
Your doctor can describe your treatment choices and what to expect. You and
your doctor can work together to develop a treatment plan that meets your
needs.
Surgery
is the usual treatment for people with skin cancer. In some cases, the
doctor may suggest
topical chemotherapy,
photodynamic therapy,
or
radiation therapy.
Because skin cancer treatment may damage healthy cells and tissues, unwanted
side effects sometimes occur. Side effects depend mainly on the type and extent
of the treatment. Side effects may not be the same for each person.
Before treatment starts, your doctor will tell you about possible side effects
and suggest ways to help you manage them.
Many skin cancers can be removed quickly and easily. Even so, you may need
supportive care
to control pain and other symptoms, to relieve the side effects
of treatment, and to ease emotional concerns. Information about such care is
available on NCI's Web site at http://www.cancer.gov/cancertopics/coping,
and from Information Specialists at 1-800-4-CANCER or
LiveHelp 2.
You may want to talk to your doctor about taking part in a clinical trial, a
research study of new ways to treat cancer or prevent it from coming back. The
section on "The Promise of Cancer
Research 4" has more information about clinical trials.
Surgery to treat skin cancer may be done in one of several ways. The method
your doctor uses depends on the size and place of the growth and other factors.
Your doctor can further describe these types of surgery:
-
Excisional skin surgery
is a common treatment to remove skin cancer.
After numbing the area, the surgeon removes the growth with a scalpel. The
surgeon also removes a border of skin around the growth. This skin is the
margin.
The margin is examined under a microscope to be certain that all the
cancer cells have been removed. The size of the margin depends on the size of
the growth.
-
Mohs surgery
(also called Mohs micrographic surgery) is often used for
skin cancer. The area of the growth is numbed. A specially trained surgeon
shaves away thin layers of the growth. Each layer is immediately examined under
a microscope. The surgeon continues to shave away tissue until no cancer cells
can be seen under the microscope. In this way, the surgeon can remove all the
cancer and only a small bit of healthy tissue.
-
Electrodesiccation
and
curettage
is often used to remove small basal
cell skin cancers. The doctor numbs the area to be treated. The cancer is
removed with a sharp tool shaped like a spoon. This tool is a
curette.
An
electric current is sent into the treated area to control bleeding and kill any
cancer cells that may be left. Electrodesiccation and curettage is usually a
fast and simple procedure.
-
Cryosurgery
is often used for people who are not able to have other
types of surgery. It uses extreme cold to treat early stage or very thin skin
cancer. Liquid nitrogen creates the cold. The doctor applies liquid nitrogen
directly to the skin growth. This treatment may cause swelling. It also may
damage nerves, which can cause a loss of feeling in the damaged area. The NCI
fact sheet "Cryosurgery in Cancer Treatment: Questions and Answers 7" has more
information.
-
Laser surgery
uses a narrow beam of light to remove or destroy cancer
cells. It is most often used for growths that are on the outer layer of skin
only. The NCI fact sheet "Lasers in Cancer Treatment: Questions and Answers 8"
has more information.
-
Grafts
are sometimes needed to close an opening in the skin left by
surgery. The surgeon first numbs and then removes a patch of healthy skin from
another part of the body, such as the upper thigh. The patch is then used to
cover the area where skin cancer was removed. If you have a skin graft, you may
have to take special care of the area until it heals.
The time it takes to heal after surgery is different for each person. You may
be uncomfortable for the first few days. However, medicine can usually control
the pain. Before surgery, you should discuss the plan for pain relief with your
doctor or nurse. After surgery, your doctor can adjust the plan if you need
more pain relief.
Surgery nearly always leaves some type of scar. The size and color of the scar
depend on the size of the cancer, the type of surgery, and how your skin heals.
For any type of surgery, including skin grafts or
reconstructive surgery,
it is
important to follow your doctor's advice on bathing, shaving, exercise, or
other activities.
|
You may want to ask your doctor these questions about surgery:
-
What kind of surgery will I have?
-
Will I need a skin graft?
-
What will the scar look like? Can anything be done to help reduce the scar?
Will I need
plastic surgery
or reconstructive surgery?
-
How will I feel after the operation?
-
If I have pain, how will it be controlled?
-
Will I have to stay in the hospital?
-
Am I likely to have infection, swelling, blistering, or bleeding, or to get a
scab where the cancer was removed?
|
Chemotherapy uses anticancer drugs to kill skin cancer cells. When a drug is
put directly on the skin, the treatment is topical chemotherapy. It is most
often used when the skin cancer is too large for surgery. It is also used when
the doctor keeps finding new cancers.
Most often, the drug comes in a cream or lotion. It is usually applied to the
skin one or two times a day for several weeks. A drug called
fluorouracil
(5-FU) is used to treat basal cell and squamous cell cancers that are in the
top layer of the skin only. A drug called
imiquimod
also is used to treat basal
cell cancer only in the top layer of skin.
These drugs may cause your skin to turn red or swell. It also may itch, hurt,
ooze, or develop a rash. It may be sore or sensitive to the sun. These skin
changes usually go away after treatment is over. Topical chemotherapy usually
does not leave a scar. If healthy skin becomes too red or raw when the skin
cancer is treated, your doctor may stop treatment.
|
You may want to ask your doctor these questions about topical chemotherapy:
-
Do I need to take special care when I put chemotherapy on my skin? What do I
need to do? Will I be sensitive to the sun?
-
When will treatment start? When will it end?
|
Photodynamic therapy (PDT) uses a chemical along with a special light source,
such as a laser light, to kill cancer cells. The chemical is a
photosensitizing agent.
A cream is applied to the skin or the chemical is injected. It stays in
cancer cells longer than in normal cells. Several hours or days later, the
special light is focused on the growth. The chemical becomes active and
destroys nearby cancer cells.
PDT is used to treat cancer on or very near the surface of the skin.
The side effects of PDT are usually not serious. PDT may cause burning or
stinging pain. It also may cause burns, swelling, or redness. It may scar
healthy tissue near the growth. If you have PDT, you will need to avoid direct
sunlight and bright indoor light for at least 6 weeks after treatment.
The NCI fact sheet "Photodynamic Therapy for Cancer: Questions and Answers 9" has
more information.
|
You may want to ask your doctor these questions about PDT:
-
Will I need to stay in the hospital while the chemical is in my body?
-
Will I need to have the treatment more than once?
|
Radiation therapy (also called radiotherapy) uses high-energy rays to kill
cancer cells. The rays come from a large machine outside the body. They affect
cells only in the treated area. This treatment is given at a hospital or clinic
in one dose or many doses over several weeks.
Radiation is not a common treatment for skin cancer. But it may be used for
skin cancer in areas where surgery could be difficult or leave a bad scar. You
may have this treatment if you have a growth on your eyelid, ear, or nose. It
also may be used if the cancer comes back after surgery to remove it.
Side effects depend mainly on the dose of radiation and the part of your body
that is treated. During treatment your skin in the treated area may become red,
dry, and tender. Your doctor can suggest ways to relieve the side effects of
radiation therapy. Also, the NCI booklet
Radiation Therapy and You: A Guide to
Self-Help During Cancer Treatment 10 offers more information.
|
You may want to ask your doctor these questions about radiation therapy:
-
How will I feel after the radiation?
-
Am I likely to have infection, swelling, blistering, or bleeding, or to get a scar
in the treated area?
-
How should I take care of the treated area?
|
Follow-up Care
Follow-up care after treatment for skin cancer is important. Your doctor will
monitor your recovery and check for new skin cancer. New skin cancers are more
common than having a treated skin cancer spread. Regular checkups help ensure
that any changes in your health are noted and treated if needed. Between
scheduled visits, you should check your skin regularly. You will find a guide
for checking your skin below 4. You
should contact the doctor if you notice anything unusual. It also is important
to follow your doctor's advice about how to reduce your risk of developing skin
cancer again.
Facing Forward Series: Life After Cancer Treatment 11 is an NCI booklet for people
who have completed their treatment. It answers questions about follow-up care
and other concerns. It has tips for making the best use of medical visits. It
also suggests ways to talk with the doctor about creating a plan of action for
your recovery and future health.
Sources of Support
Skin cancer has a better
prognosis,
or outcome, than most other types of
cancer. Still, learning you have any type of cancer can be upsetting. You may
worry about treatments, managing side effects, and medical bills. Doctors,
nurses, and other members of the health care team can answer your questions.
Meeting with a social worker, counselor, or member of the clergy can be helpful
if you want to talk about your feelings or concerns. Often, a social worker can
suggest resources for financial aid, transportation, or emotional support.
Support groups also can help. In these groups, patients or their family members
meet with other patients or their families to share what they have learned
about coping with cancer and the effects of treatment. Groups may offer support
in person, over the telephone, or online. You may want to talk with a member of
your health care team about finding a support group.
Information Specialists at 1-800-4-CANCER and at
LiveHelp 2 (http://www.cancer.gov/cis) can
help you locate programs, services, and publications. Also, you may want to see
the NCI fact sheet "National Organizations That Offer Services to People With
Cancer and Their Families 12."
The Promise of Cancer Research
Doctors are conducting clinical trials (research studies in which people
volunteer to take part).
Clinical trials are designed to answer important questions and to find out
whether new approaches are safe and effective. Research already has led to
advances, such as photodynamic therapy, and researchers continue to search for
better ways to prevent and treat skin cancer.
For basal cell cancer, researchers are studying gene changes that may be risk
factors for the disease. They also are comparing
biological therapy
with
surgery to treat basal cell cancer.
People who join clinical trials may be among the first to benefit if a new
approach is effective. And even if participants do not benefit directly, they
still make an important contribution by helping doctors learn more about the
disease and how to control it in other patients. Although clinical trials may
pose some risks, researchers do all they can to protect their patients.
If you are interested in being part of a clinical trial, talk with your doctor.
You may want to read the NCI booklet Taking Part in Cancer Treatment Research Studies 13. It explains how clinical trials are carried out and explains their possible benefits and risks.
NCI's Web site includes a section on clinical trials at http://www.cancer.gov/clinicaltrials.
It has general information about clinical trials as well as detailed
information about specific ongoing studies of skin cancer. Information
Specialists at 1-800-4-CANCER or at
LiveHelp 2 at http://www.cancer.gov can
answer questions and provide information about clinical trials.
How To Do a Skin Self-Exam
Your doctor or nurse may suggest that you do a regular skin self-exam to check
for skin cancer, including
melanoma.
The best time to do this exam is after a shower or bath. You should check your
skin in a room with plenty of light. You should use a full-length mirror and a
hand-held mirror. It's best to begin by learning where your birthmarks, moles,
and other marks are and their usual look and feel.
Check for anything new:
-
New mole (that looks different from your other moles)
-
New red or darker color flaky patch that may be a little raised
-
New flesh-colored firm bump
-
Change in the size, shape, color, or feel of a mole
-
Sore that does not heal
Check yourself from head to toe. Don't forget to check your back, scalp,
genital area, and between your buttocks.
-
Look at your face, neck, ears, and scalp. You may want to use a comb or a blow
dryer to move your hair so that you can see better. You also may want to have a
relative or friend check through your hair. It may be hard to check your scalp
by yourself.
-
Look at the front and back of your body in the mirror. Then, raise your arms
and look at your left and right sides.
-
Bend your elbows. Look carefully at your fingernails, palms, forearms
(including the undersides), and upper arms.
-
Examine the back, front, and sides of your legs. Also look around your genital
area and between your buttocks.
-
Sit and closely examine your feet, including your toenails, your soles, and the
spaces between your toes.
By checking your skin regularly, you will learn what is normal for you. It may
be helpful to record the dates of your skin exams and to write notes about the
way your skin looks. If your doctor has taken photos of your skin, you can
compare your skin to the photos to help check for changes. If you find anything
unusual, see your doctor.
National Cancer Institute Information Resources
You may want more information for yourself, your family, and your doctor. The
following National Cancer Institute (NCI) services are available to help you.
Telephone
The NCI's Cancer Information Service (CIS) provides accurate, up-to-date
information on cancer to patients and their families, health professionals, and
the general public. Information Specialists translate the latest scientific
information into understandable language and respond in English, Spanish, or on
TTY equipment. Calls to the CIS are free.
Telephone: 1-800-4-CANCER (1-800-422-6237)
TTY: 1-800-332-8615
Internet
The NCI's Web site (http://www.cancer.gov) provides information
from numerous NCI sources. It offers current information on cancer prevention,
screening, diagnosis, treatment, genetics, supportive care, and ongoing
clinical trials. It has information about NCI's research programs and funding
opportunities, cancer statistics, and the Institute itself. Information
Specialists provide live, online assistance through
LiveHelp 2.
National Cancer Institute Publications
National Cancer Institute (NCI) publications can be ordered by writing to the
address below:
Publications Ordering Service
National Cancer Institute
Suite 3035A
6116 Executive Boulevard, MSC 8322
Bethesda, MD 20892-8322
Many NCI publications can be viewed, downloaded, and ordered from
http://www.cancer.gov/publications 14 on the Internet. In addition,
people in the United States and its territories may order these and other NCI
publications by calling the NCI's Cancer Information Service at 1-800-4-CANCER.
Booklets About Skin Changes and Skin Cancer
What You Need To Know
About™ Skin Cancer 15
What You Need To
Know About™ Melanoma 1
What
You Need To Know About™ Moles and Dysplastic Nevi 16
Booklets and Fact Sheets About Cancer Treatment and Support
Radiation Therapy and You: A Guide to Self-Help During Cancer Treatment 10
(also available in Spanish: La radioterapia y usted: una guía de autoayuda
durante el tratamiento del cáncer)
Biological Therapy: Treatments That Use Your Immune System to Fight
Cancer
Eating Hints for Cancer Patients: Before, During & After Treatment 17
(also available in Spanish: Consejos de alimentación para pacientes con cáncer:
antes, durante y después del tratamiento)
Understanding Cancer Pain 18 (also available in Spanish:
El dolor
relacionado con el cáncer 19)
Pain Control: A Guide for People with Cancer and Their Families 20 (also
available in Spanish: Control del dolor: guía para las personas con cáncer y
sus familias)
Get Relief from Cancer Pain
Thinking About Complementary and Alternative Medicine: A Guide for People with Cancer 21
"Biological Therapies for Cancer: Questions and Answers 22" (also available in
Spanish: "Terapias biológicas: el uso del sistema inmune para tratar el
cáncer 23")
"How To Find a Doctor or Treatment Facility If You Have Cancer 6" (also available
in Spanish: "Cómo encontrar a un doctor o un establecimiento de tratamiento si
usted tiene cáncer 24")
"Understanding Prognosis and Cancer Statistics 25" (also available in Spanish:
" 26La
interpretación de los pronósticos y las estadísticas del cáncer")
"National Organizations That Offer Services to People With Cancer and Their
Families 12" (also available in Spanish: "Organizaciones nacionales que brindan
servicios a las personas con cáncer y a sus familias 27")
"How To Find Resources in Your Own Community If You Have Cancer 28" (also
available in Spanish: "Cómo encontrar recursos en su comunidad si usted tiene
cáncer 29")
"Cryosurgery in Cancer Treatment: Questions and Answers 7"
"Photodynamic Therapy for Cancer: Questions and Answers 9"
"Lasers in Cancer Treatment: Questions and Answers 8"
Publications About Living With Cancer
Advanced Cancer: Living Each Day 30
Facing Forward Series: Life After
Cancer Treatment 11 (also available in Spanish:
Siga adelante: la vida después del tratamiento del cáncer 31)
Facing Forward Series: Ways You Can Make a
Difference in Cancer 32
Taking Time: Support for People with Cancer and
the People Who Care About Them 33
When Cancer Recurs: Meeting the Challenge 34
Publications About Clinical Trials
Taking Part in Cancer Treatment Research Studies 13
Taking Part in
Clinical Trials: Cancer Prevention Studies: What Participants Need To Know 35
(also available in Spanish: La participación en los estudios
clínicos: estudios para la prevención del cáncer)
|