|

|



(513KB)

You may be a candidate for surgery if you are an adult with:
-
A body mass index (BMI) of 40 or more (about 100 pounds overweight for men and
80 pounds for women) or a BMI between 35 and 39.9
and a serious obesity-related health problem such as type 2 diabetes, coronary
heart disease, or severe sleep apnea (when breathing stops for short periods
during sleep).
-
Acceptable operative risks.
-
An ability to participate in treatment and long-term follow-up.
-
An understanding of the operation and the lifestyle changes you will need to
make.
|
The Normal Digestive Process
How does surgery promote weight loss?
What are the surgical options?
Adjustable Gastric Band
Roux-en-Y Gastric Bypass
Gastric Sleeve
Biliopancreatic Bypass With a Duodenal Switch
What are the complications of these operations?
Open and Laparoscopic Bariatric Surgery
Bariatric Surgery for Adolescents
Medical Costs
Is surgery for you?
Research
Additional Reading
Additional Resource
Severe obesity is a chronic condition that is difficult to treat through diet
and exercise alone. Bariatric surgery is an option for people who are severely
obese and cannot lose weight by traditional means or who suffer from serious
obesity-related health problems. The operation promotes weight loss and reduces
the risk of type 2 diabetes by restricting food intake and, in some operations,
interrupting the digestive process to prevent the absorption of some calories
and nutrients. Recent studies suggest that bariatric surgery may even have a
favorable impact on mortality (death) rates in severely obese patients. The
best results are achieved when bariatric surgery is followed with healthy
eating behaviors and regular physical activity.
|
The
Normal Digestive Process
|
Normally, as food moves along the digestive tract,
digestive juices and enzymes digest and absorb calories and nutrients. After we chew and swallow our food, it moves down the esophagus to
the stomach, where a strong acid continues the digestive process. The stomach
can hold about 3 pints of food at one time. When the stomach contents move to
the duodenum, the first segment of the small intestine, bile and pancreatic
juice speed up digestion. Most of the iron and calcium in the food we eat is
absorbed in the duodenum. The jejunum and ileum, the remaining two segments of
the nearly 20 feet of small intestine, complete the absorption of almost all
calories and nutrients. The food particles that cannot be digested in the small
intestine are stored in the large intestine until eliminated.
|
How
does surgery promote weight loss?
|
Bariatric surgery produces weight loss by restricting food intake
and, in some cases, interfering with nutrition through malabsorption. Patients
who undergo bariatric surgery must also commit to a lifetime of healthy eating
and regular physical activity. These healthy habits help ensure that the weight
loss from surgery is successfully maintained.
|
What are the
surgical options?
|
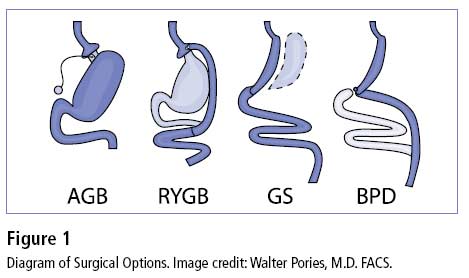
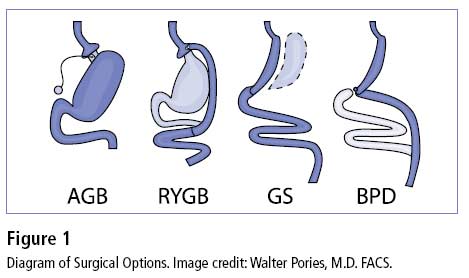
There are four types of operations that are commonly offered in the
United States: adjustable gastric band (AGB), Roux-en-Y gastric bypass (RYGB),
gastric sleeve (GS), and biliopancreatic bypass with a duodenal switch (BPD).
Each has its own benefits and risks. To select the option that is best for you,
you and your physician will consider that operation’s benefits and risks
along with many other factors, including BMI, eating behaviors, obesity-related
health conditions, and previous operations.
|
Adjustable Gastric Band
|
AGB works primarily by decreasing food intake. Food
intake is limited by placing a small bracelet-like band around the top of the
stomach to produce a small pouch about the size of a thumb. The outlet size is
controlled by a circular balloon inside the band that can be inflated or
deflated with saline solution to meet the needs of the patient.
|
Roux-en-Y Gastric
Bypass
|
RYGB works by restricting food intake and by
decreasing the absorption of food. Food intake is limited by a small pouch that
is similar in size to the adjustable gastric band. In addition, absorption of
food in the digestive tract is reduced by excluding most of the stomach,
duodenum, and upper intestine from contact with food by routing food directly
from the pouch into the small intestine.
|
Gastric
Sleeve
|
GS is usually performed as the first stage of
biliopancreatic bypass with duodenal switch in patients who may be at high risk
for complications from more extensive types of surgery. These patients’
high risk levels are due to body weight or medical conditions. A GS operation
restricts food intake and does not lead to decreased absorption of food.
However, most of the stomach is removed, which may decrease production of a
hormone called ghrelin. A decreased amount of ghrelin may reduce hunger more
than other purely restrictive operations, such as gastric band.
|
Biliopancreatic
Bypass With a Duodenal Switch
|
BPD, usually referred to as a “duodenal
switch,” is a complex bariatric operation that includes removing the
lower portion of the stomach and creating a gastric sleeve with the small pouch
that remains. That pouch is connected directly to the small intestine,
completely bypassing the duodenum and upper small intestine from contact with
food. BPD produces significant weight loss. However, the mortality rate is
higher than with other bariatric operations and there are more long-term
complications because of decreased absorption of food, vitamins, and minerals.
|
What
are the complications of these operations?
|
Early complications of these operations can include
bleeding, infection, leaks from the site where the intestines are sewn
together, and blood clots in the legs that can progress to the lungs and heart.
Examples of complications that may occur later include malnutrition, especially
in patients who do not take their prescribed vitamins and minerals. In some
cases, if the malnutrition is not addressed promptly, diseases such as
pellagra, beri beri, and kwashiorkor may occur along with permanent damage to
the nervous system. Other late complications include strictures (narrowing of
the sites where the intestine is joined) and hernias.
Two kinds of hernias may occur after a patient has bariatric surgery. An
incisional hernia is a weakness that sticks out from the abdominal wall’s
fascia (connective tissue) and may cause a blockage in the bowel. An internal
hernia occurs when the small bowel is displaced into pockets in the lining of
the abdomen. These pockets are created when the intestines are sewn together.
Internal hernias are considered more dangerous than incisional ones and need
prompt attention to avoid serious complications.
Research indicates that about 10 percent of patients who undergo bariatric
surgery may have unsatisfactory weight loss or regain much of the weight that
they lost. Some behaviors such as frequent snacking on high-calorie foods or
lack of exercise can contribute to inadequate weight loss. Technical problems
that may occur with the operation, like a stretched pouch or separated
stitches, may also contribute to inadequate weight loss.
Some patients may also require emotional support to help them
through the postoperative changes in body image and personal relationships.
|
Open
and Laparoscopic Bariatric Surgery
|
Bariatric surgery may be performed through “open”
approaches, which make abdominal incisions in the traditional manner, or by
laparoscopy. With the laparoscopic approach, sophisticated instruments are
inserted through 1/2-inch incisions and guided by a small camera that sends
images to a television monitor. Most bariatric surgery today is performed
laparoscopically because it requires a smaller cut, creates less tissue damage,
leads to earlier discharges from the hospital, and has fewer complications,
especially postoperative hernias.
However, not all patients are suitable for laparoscopy. Patients who are
extremely obese, who have had previous abdominal surgery, or have complicating
medical problems may require the open approach.
|
Bariatric
Surgery for Adolescents
|
Rates of obesity among youth are on the rise. Bariatric surgery is
sometimes considered as a treatment option for adolescents who have developed
extreme obesity. Although it is becoming clear that adolescents can lose weight
following bariatric surgery, there are numerous unanswered questions about the
long-term effects of these operations on adolescents’ developing bodies
and minds.
Experts in pediatric obesity and bariatric surgery recommend that surgical
treatment only be considered when adolescents have tried for at least 6 months
to lose weight and have not been successful. Candidates should be extremely
obese (typically with BMI greater than 40), have reached their adult height
(usually 13 or older for girls and 15 or older for boys), and have serious
weight-related health problems, such as type 2 diabetes, sleep apnea, heart
disease, or significant functional or psychosocial impairment. In addition,
potential patients and their parents should be evaluated to see how emotionally
prepared they are for the operation and the lifestyle changes they will need to
make. Patients should be referred to specialized adolescent bariatric surgery
centers with a team of experts qualified to meet their unique needs.
A growing body of research suggests that both weight and health of extremely
obese youth can be favorably changed by bariatric surgery. Over the years,
gastric bypass surgery has been the predominant operation used to treat
adolescent extreme obesity. An estimated 2,700 adolescent bariatric surgeries
were performed between 1996 and 2003 (Arch Pediatr Adolesc Med. 2007;161:217–221).
A review of short-term data from the national inpatient sample (the largest
inpatient database in the United States) suggests that these operations are at
least as safe for adolescents as adults. As yet, the adjustable gastric band
has not been approved for use in the United States for people younger than age
18, but favorable weight-loss outcomes following adjustable gastric banding for
adolescents have been reported internationally.
|
Medical
Costs
|
Bariatric procedures, on average, cost from $20,000 to $25,000.
Medical insurance coverage varies by state and insurance provider. In 2004, the
U.S. Department of Health and Human Services reduced barriers to obtaining
Medicare coverage for obesity treatments. Bariatric surgery may be covered if
it is medically appropriate and if it is performed to correct an
obesity-related illness. If you are considering bariatric surgery, contact your
regional Medicare or Medicaid office or health insurance plan to find out if
the procedure is covered.
|
Is surgery for you?
Bariatric surgery may be the next step for people who remain
severely obese after trying nonsurgical approaches, especially if they
have an obesity-related disease.
|
Bariatric surgery may be the next step for people who remain
severely obese after trying nonsurgical approaches, especially if they have an
obesity-related disease. Surgery to produce weight loss is a serious
undertaking. Anyone thinking about undergoing this type of operation should
understand what it involves. Answers to the following questions may help you
decide whether weight-loss surgery is right for you.
Are you:
-
Unlikely to lose weight or keep it off over the long-term with nonsurgical measures?
-
Well informed about the surgical procedure and the effects of treatment?
-
Determined to lose weight and improve your health?
-
Aware of how your life may change after the operation (adjustment to the side
effects of the operation, including the need to chew food well and inability to
eat large meals)?
-
Aware of the potential risk for serious complications, dietary restrictions,
and occasional failures?
-
Committed to lifelong healthy eating and physical activity habits, medical
follow-up, and vitamin/mineral supplementation?
Remember: There are no guarantees for any method, including surgery, to
produce and maintain weight loss. Success is possible only with maximum
cooperation and commitment to behavioral change and medical follow-up—and
this cooperation and commitment must be carried out for the rest of your life.
|
Research
Success is possible only with maximum cooperation and commitment to behavioral change and medical follow-up—and this cooperation and commitment must be carried out for the rest of your life.
|
In 2003, the National Institute of Diabetes and Digestive and
Kidney Diseases (NIDDK) of the National Institutes of Health (NIH) formed a
partnership with researchers called the Longitudinal Assessment of Bariatric
Surgery, or LABS. LABS researchers are experts in bariatric surgery, obesity
research, internal medicine, behavioral science, and related fields. Their
mission is to plan and conduct studies that will lead to better understanding
of bariatric surgery and its impact on the health and well-being of patients
with extreme obesity. For more information on LABS, visit
www.niddklabs.org.
To help determine if bariatric surgery is appropriate for adolescents, NIH
launched a prospective study called Teen-LABS in 2007. Over the next 5 years,
the multicenter study will collect data from adolescents who are scheduled for
surgery to evaluate bariatric surgery’s benefits and risks. Researchers
will collect data about obesity-related medical problems, other health risk
factors, and quality of life from the patients before they undergo surgery and
2 years after surgery. Researchers will then compare the adolescent outcomes to data collected from adults.
For more information about Teen-LABS, visit
www.nih.gov/news/pr/apr2007/niddk-16.htm and
www.cincinnatichildrens.org/teen-LABS.
|
| Additional Reading |
Clinical Guidelines on the Identification, Evaluation, and
Treatment of Overweight and Obesity in Adults. National Heart, Lung,
and Blood Institute, NIH. September 1998. Available at
www.nhlbi.nih.gov.guidelines/obesity/ob_gdlns.pdf.
Dieting and Gallstones. NIH Publication No. 06–3677. This fact
sheet explains what gallstones are, how they are formed, and the roles obesity
and rapid weight loss play in the development of gallstones. Available from
WIN.
Gastrointestinal Surgery for Severe Obesity. Consensus Statement, NIH
Consensus Development Conference, March 25–27, 1991; Public Health
Service, National Institutes of Health, Office of Medical Applications of
Research. This publication, written for health professionals, summarizes the
findings of a conference discussing treatments for severe obesity. Available at
http://consensus.nih.gov/1991/1991GISurgeryObesity084html.htm.
Pharmacological and Surgical Treatment of Obesity: Evidence
Report/Technology Assessment: Number 103. Shekelle PG, Morton SC,
Maglione M, et al. Agency for Healthcare Research and Quality (AHRQ). AHRQ
Publication Number 04–E028–1; 2004. Rockville, MD. This report
reviews the scientific evidence on weight-loss drugs and bariatric surgery
among children, adolescents, and adults. Available at
www.ahrq.gov/downloads/pub/evidence/pdf/obespharm/obespharm.pdf.
Weight Loss for Life. NIH Publication No. 04–3700. This booklet
describes ways to lose weight and encourages healthy eating habits and regular
physical activity. Available from WIN.
|
| Additional Resource |
American Society for Metabolic and Bariatric Surgery
100 SW 75th Street
Suite 201
Gainesville, FL 32607
Phone: (352) 331–4900
Fax: (352) 331–4975
Internet: www.asbs.org
|
| |
Weight-control Information Network
1 WIN Way
Bethesda, MD 20892–3665
Phone: (202) 828–1025
Toll-free number: 1–877–946–4627
Fax: (202) 828–1028
Email: win@info.niddk.nih.gov
Internet: www.win.niddk.nih.gov
The Weight-control Information Network (WIN) is a service of the National
Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National
Institutes of Health, which is the Federal Government’s lead agency
responsible for biomedical research on nutrition and obesity. Authorized by
Congress (Public Law 103–43), WIN provides the general public, health
professionals, the media, and Congress with up-to-date, science-based health
information on weight control, obesity, physical activity, and related
nutritional issues.
Publications produced by WIN are reviewed by both NIDDK scientists and outside
experts. This fact sheet was also reviewed by Walter Pories, M.D., FACS,
Professor of Surgery and Biochemistry, Brody School of Medicine at East
Carolina University; and Thomas Inge, M.D., Ph.D., FACS, FAAP, Assistant
Professor of Surgery and Pediatrics and Surgical Director, Comprehensive Weight
Management Center, Cincinnati Children’s Hospital Medical Center.
This publication is not copyrighted. WIN encourages users of this brochure to
duplicate and distribute as many copies as desired.
|


|
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
National Institutes of Health
NIH Publication No. 08–4006
December 2004
Updated March 2008
|
| |
|
|
|