Home > Weekly Newsletters > Women
September 15, 2008
Natural Childbirth Moms More Attuned to Babies' Cry
THURSDAY, Sept. 11 (HealthDay News) -- Mothers who delivered their babies vaginally appear to be much more sensitive to the cry of their own child within a few weeks of the birth compared with those who deliver by Caesarean section, a new study shows.
The finding, published in The Journal of Child Psychology and Psychiatry, give researchers insight into why postpartum depression seems to be linked more often to Caesarean birth.
The researchers based their findings on MRI scans that show heightened activity in the sections of the brain thought to regulate emotions, motivation and habitual behaviors. They believe this may be because vaginal childbirth involves the release of oxytocin -- a key mediator of maternal behavior in animals -- from the posterior pituitary, uterine contractions and vagino-cervical stimulation.
The researchers also studied areas of the brain affected by delivery conditions and found ties between brain activity and measures of mood. This suggests that some of the same brain regions may help regulate postpartum mood.
"As more women opt to wait until they are older to have children, and by association be more likely to have a Caesarean-section delivery, these results are important, because they could provide better understanding of the basic neurophysiology and psychology of parent-infant attachment," lead author James Swain, of Yale University's Child Study Centre, said in a news release issued by the journal's publisher. "This work could lead to early detection of families at risk for postpartum depression and attachment problems and form a model for testing interventions."
Caesarean delivery, which occurs via incisions in the abdominal and uterine wall, is required at times to protect the health or survival of infant or mother. The procedure's use has increased in the United States dramatically, from 4.5 percent of all deliveries in 1965 to a recent high in 2006 of 29.1 percent.
More information
The U.S. Department of Health & Human Services has more about postpartum depression.
Fall Risk Higher in Older Women Who Sleep Less

MONDAY, Sept. 8 (HealthDay News) -- Getting five hours or less of sleep a night increases the risk of falls among women aged 70 and older, says a U.S. study.
It also found that the use of sleep medications doesn't seem to influence the link between amount of sleep and fall risk.
Researchers measured sleep, sleep efficiency (percentage of time in bed spent sleeping) and frequency of falls in 2,978 women aged 70 and older. The women averaged 6.8 hours of sleep per night and spent an average 77.2 minutes awake after initial sleep onset.
Overall, the average number of falls one year after the collection of sleep data was 0.84. But 549 (18.4 percent) of the women had two or more falls during that year. Women who slept five hours or less per night were more likely to have two or more falls than those who slept more than seven to eight hours a night.
The researchers found that women with a sleep efficiency of less than 70 percent were 1.36 times more likely to have a fall than women with a sleep efficiency of 70 percent or more. Women with 120 minutes or more of wake time after sleep onset were 1.33 times more likely to fall than those who were awake less than 120 minutes after sleep onset.
"In all, 214 subjects (7.2 percent) reported current use of benzodiazepines (hypnotic medicines used to treat insomnia). Use of any benzodiazepine (short and long combined) was associated with a 1.34-fold increased risk of falls, whereas short- and long-acting benzodiazepine use was associated with an increased odds of 1.43 and 1.18, respectively," wrote Katie L. Stone, of the California Pacific Medical Center Research Institute in San Francisco, and colleagues.
The study was published in the Sept. 8 issue of the Archives of Internal Medicine.
"Future studies, in particular randomized trials, are needed to determine the effects of newer pharmaceutical interventions for insomnia (e.g., benzodiazepine receptor agonists) or cognitive behavioral therapy for insomnia on risk of falls," the authors concluded. "In addition, future studies using comprehensive and objective measures of sleep should examine the interrelationships between specific sleep characteristics (e.g., sleep-related breathing disorder, hypoxia and measures of sleep duration and fragmentation) to determine if these disorders contribute independently toward risk of falls."
More information
The U.S. National Institute on Aging has more about older adults and falls.
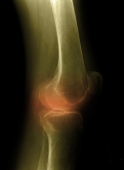
Postmenopausal Women With Breast Cancer Face Joint Issues
TUESDAY, Aug. 12 (HealthDay News) -- Postmenopausal women with breast cancer who are receiving endocrine treatment may be at increased risk of joint issues, including arthritis, a new study finds.
British researchers publishing in the September issue of The Lancet Oncology, found that previous use of hormone replacement therapy (HRT), hormone-receptor positivity, previous chemotherapy, obesity and treatment with anastrozole -- an aromatase inhibitor -- all increased the chances of these women developing joint problems.
These increased risks appear to be tied to the significant drop in estrogen levels the patients experience during endocrine treatment. Estrogen deficiency previously has been associated with joint issues in other studies.
The researchers made their discoveries during a trial comparing the use of either an aromatase inhibitor (anastrozole) or tamoxifen in some 9,000 postmenopausal women with breast cancer. In the study, joint symptoms were reported in:
- 41 percent of women who had previously used HRT versus 29 percent of those who had not.
- Women who received previous chemotherapy also reported significantly more joint symptoms than those who had not (39 percent versus 31 percent).
- The more obese the women was, based on the body-mass index, the more likely she had joint issues.
"Awareness of risk factors for joint symptoms will help both clinicians and patients to anticipate and manage these symptoms and ensure optimum adherence to endocrine treatment," researcher Dr. Ivana Sestak of Cancer Research UK, said in a news release issued by her organization.
More information
The National Cancer Institute has more about breast cancer.
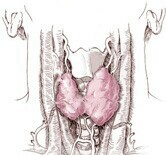
Thyroid Hormone May Boost Women's Alzheimer's Risk
TUESDAY, July 29 (HealthDay News) -- High or low levels of the hormone thyrotropin may be associated with an increased risk of Alzheimer's disease in women. Thyrotropin affects thyroid gland function and thyroid hormone levels.
Between 1977 and 1979, researchers at Beth Israel Deaconess Medical Center and Harvard Medical School measured thyrotropin levels in 1,864 people, average age 71, without cognitive problems. The participants were then assessed for dementia every two years.
After an average of 12.7 years of follow-up, 209 participants developed Alzheimer's disease. After they adjusted for the other factors, the researchers found that women with the lowest (less than one milli-international unit per liter) and highest (more than 2.1 milli-international units per liter) levels of thyrotropin had more than a twofold increased risk of Alzheimer's.
No association between thyrotropin levels and Alzheimer's risk was noted in men.
"Whether altered thyrotropin levels occur before or after onset of Alzheimer's disease, the neuropathologic mechanism is unclear," the study authors wrote.
Brain changes caused by Alzheimer's disease may cause a decrease in the amount of thyrotropin released or changes in the body's responsiveness to the hormone, the researchers said. Or, it may be that high or low thyrotropin levels damage neurons or blood vessels, resulting in cognitive problems.
"In conclusion, low and high thyrotropin levels were associated with an increased risk of incident Alzheimer's disease in women but not in men. These findings should be considered hypothesis-generating and should be validated in other populations before clinical conclusions are drawn," the researchers wrote.
The study was published in the July 28 issue of the journal Archives of Internal Medicine.
More information
The U.S. National Institute on Aging has more about Alzheimer's disease.