Section II:E. Water Sampling Guidelines
 Water sampling is critical to determining whether
Legionnaires' disease bacteria (LDB) are present and at what levels. To ensure accurate detection, proper methods
should be used when collecting and transporting samples. A number of analytical techniques are available for detection of
LDB. These vary in their sensitivity, specificity, and turnaround time. Depending on individual circumstances, one or more of these methods may be preferable for a given workplace or system. Water sampling is critical to determining whether
Legionnaires' disease bacteria (LDB) are present and at what levels. To ensure accurate detection, proper methods
should be used when collecting and transporting samples. A number of analytical techniques are available for detection of
LDB. These vary in their sensitivity, specificity, and turnaround time. Depending on individual circumstances, one or more of these methods may be preferable for a given workplace or system.
 Physical Survey Physical Survey |
 |
|
Fig. 1: Site assessment |
Site Assessment: Estimate the size of the building and the number of water services in the facility during the initial walk-through. During the inspection, determine the number of samples needed and arrange with the appropriate laboratory for supply and shipment of sterile sampling containers and swabs and for the analysis of samples. Obtain or prepare a simple schematic diagram of the water services. Note the following features:
- The location of the incoming municipal or private water supply.
- The location of storage tanks, water treatment systems, and pumps.
- The location of water heaters and boilers.
- The type of fittings used in the system such as taps, showers, valves, and the pipe-work material.
- The location of all cooling towers, evaporative condensers, and fluid coolers.
- The location and type of all systems served by the cooling tower water including sump tanks, condensers, and indirect evaporative cooling coils in air-handling units.
- The location of any evaporative cooling systems or humidifiers.
- The location of ornamental fountains, whirlpools, eye washes, safety showers, or other water sources within or near the facility.
Water Route Inspection: Trace the route of the service from the point of entry of the water supply.
- Note the condition of pipes, jointing methods used, insulation, sources of heat, and the kind of insulation in water storage tanks.
- Note any disconnected fittings, "dead legs," and cross-connections with other services. Once you have identified these features, take water samples from:
- The incoming water supply
- Each storage tank and water heater
- A representative number of faucets for each of the hot and cold water systems in the facility
- All cooling towers, evaporative condensers, humidifiers, spas, showers, and other aerosol-generating sources.
- The water entering or leaving any other type of fitting or piece of equipment under particular suspicion
Conditions
That Promote Growth:
LDB is widely
distributed in water systems. Under
ideal conditions, the bacterium is capable of multiplication within
domestic water systems. Low, even
non-detectable, levels of the
organism can colonize a water source
and grow to high concentrations.
Note: It is important to remember that any water system can be a source of bacteria
if the water in it is subjected to conditions that promote growth of the LDB.
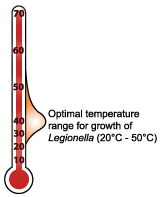 |
- Water conditions that tend to promote the growth of LDB include:
- Stagnation
- Warm water temperatures between 20° and 50°C (68° and 122°F)
- pH between 5.0 and 8.5
- Sediment that tends to promote growth of commensal micro flora
- Microorganisms such as algae, flavobacteria, and Pseudomonas,
which supply essential
nutrients for growth of LDB,
or protozoa that harbor the
organism such as amoebae
- Water systems that frequently provide optimal conditions for growth of LDB include:
- Cooling towers, evaporative condensers, and fluid coolers that use water evaporation to reject heat. These include many industrial processes that use water to remove excess heat.
- Domestic hot-water systems with water heaters that operate below 60°C (140°F) and deliver water to taps below 50°C (122°F).
- Poorly maintained humidifiers and decorative fountains that create a water spray and use water at temperatures favorable to growth.
- Spas and whirlpools with aeration.
- Dental water lines, which are frequently maintained at temperature above 20°C (68°F) and sometimes as warm as 37°C (98.6°F) for patient comfort.
- Possibly other systems such as stagnant water in fire sprinkler systems or warm water for eye washes or safety showers.
 |
| Fig. 2: Note all potential water source |
Other Sources: It is important not to overlook any potential water sources in the building such as:
- Water to ice machines
- Plastic injection molding equipment
- Metal working fluids
- Hot springs (waterfalls)
- Respiratory therapy
equipment
- Supermarket reservoir misters
|
 Water Sampling Protocol Water Sampling Protocol |
 |
|
Fig. 3: Use respiratory
protection when appropriate |
Respiratory Protection: Wear appropriate respiratory protection during the examination of water systems if a significant potential exists for exposure to high concentrations of contaminated aerosols. For example,
wear a respirator while inspecting
and collecting water samples near an
aerosol generating water source,
such as an operating spray
humidifier, water mister, fountain,
or shower, in a facility where there is a confirmed outbreak.
- Respirators should be in the form of a half-face respirator (fig. 3) equipped with a HEPA or similar filter capable of effectively collecting particles of 1-micrometer.
Sample Collection:
Please Note: It is important not to flush water outlets before taking a
sample because the end section of the water system may be a contaminated site.
 |
| Fig. 4: Measure water temperature |
- Collect 250 milliliter to 1 Liter of water in sterile polypropylene containers with a
sufficient type and amount of neutralizer for any disinfectant agent in the water system. For
example, sodium thiosulfate is used to neutralize residual chlorine and other halogens.
Water samples high in copper or zinc and wastewater samples high in heavy metals can be treated
with a chelating agent that will reduce metal toxicity. Contact the biocide manufacturer for
instructions on appropriate neutralization to prevent continuation of bactericidal action during sample transit.
- Collect swab samples using pre-packaged sterile swabs in their own
containers or small sterile glass or polypropylene bottles.
Sample Analysis:
- Submit the water samples to a laboratory that is certified for microbial water analysis and
experienced in LDB detection using culture methods that measure colony forming
units (CFU) of LDB per milliliter of water.
- The microbiological laboratory that will analyze the samples should be able to provide sampling supplies
or recommend commercial sources. Many commercially available collection bottles for drinking
water samples contain sodium thiosulfate.
Source of Supply Water Sampling:
- Detectable levels of LDB in a water system may indicate contamination of the
source water supply. The concentration of
LDB in the source water represents the
maximum allowable level in the system.
Measurement of Water Temperature:
- Measure the temperature of the sampled water (place the thermometer in the water stream flowing from
an outlet valve or faucet, not in the sample container, or use an infrared thermometer) (fig.4).
- When measuring temperature from faucets, showers, fountains, etc., record the initial water temperature.
Allow the water to run and measure the temperature every two minutes until the temperature stabilizes.
- Record the initial and final water temperatures and the time needed for the water temperature to stabilize.
- Compare the initial and final water temperatures with the set temperature.
Temperatures in cold-water systems should be maintained at a sufficiently low temperature
(20°C, 68°F, or lower) to minimize bacterial growth. Temperature in hot-water systems should be
maintained at a sufficiently high temperature (60°C, 140°F, or higher).
- Sanitize the thermometer with isopropyl alcohol before measuring the temperature of each sample to avoid cross-contamination of the samples.
Collection of Pre- and Post-flush Samples:
- Collect a 250-mL to 1-Liter 'pre-flush" sample of the first water drawn from bottom drains
and outlet valves of storage tanks, sumps, and water heaters as will as faucets and showerheads.
- Allow the water to run until the temperature stabilizes and collect a second "post-flush" sample when
the water temperature is constant.
Collection of Swab and Material Samples:
- Swab areas where there is scale build up (pre-wet the swabs with water taken form the sampling site).
- Collect samples of sludge, slime, or sediment with swabs or in sterile containers.
|
 Sample Transportation Sample Transportation |
 |
| Fig. 5: Samples should be protected and shipped quickly |
Sample Preparation:
- Wrap vinyl tape clockwise around the neck of each bottle to hold its screw cap firmly in place and seal the interface between the cap and the bottle.
- Wrap absorbent paper around bottles, and place the bottles in a sealable (zip-lock) plastic bag.
- Place the sealed plastic bag in an insulated container (Styrofoam chest or box).
Storage:
- Samples should be protected from temperature extremes such as sunlight or other external heat or cold sources during transport and storage, for example, temperatures below 3°C
(37°F) and above 30°C (86°F).
- Samples should be stored at room temperature (20° ± 5°C,
68°F) and processed within two days.
Shipping:
- Ship samples to the testing laboratory using overnight mail.
- Make arrangements for weekend receipt when shipping on a Friday.
|
 Monitoring Monitoring |
 |
| Fig. 6: Water samples are the best means of source identification |
Air: Air samples collected on special culture plates with an Andersen-type sampler rarely demonstrate the presence of
LDB in the air.
- Negative results are frequent because of the difficulty in maintaining viability of the organism on the culture plates.
- Air sampling for LDB is strongly discouraged as a means of measuring potential exposure, because of the high likelihood of false-negative results.
Water: Analysis of water samples from a source suspected of
LDB contamination is a valuable means of identifying potential sources of the bacterium.
- A microbiological laboratory certified for microbial water analysis and experienced in
LDB detection can determine the number of organisms present in colony forming units (CFU) per volume of water and can identify the different serogroups
of
L. pneumophila well as other species of
Legionella.
|
 Microbiological Analysis Microbiological Analysis |
 |
| Fig. 7: Cultured samples can identify specific serogroups |
Cultured Samples: Water samples are cultured on a buffered charcoal yeast extract (BCYE)
culture growth medium.
- Preliminary culture results typically require three to five days for confirmation from the time of submission.
- Confirmation of culture results may take additional time because some
LDB take 10 to 14 days to form visible colonies.
- Hold primary plates for a minimum of 14 days before reporting them negative.
- Selective isolation processes can reduce overgrowth by other microorganisms and can aid in the determination of
LDB.
- Analyze cultured samples to identify specific serogroups. There is strong evidence of a casual link when the same serogroup and subtype of an organism is isolated from a patient and a water source.
Direct Fluorescence Antibody (DFA): The number of organisms in a water sample can also be determined via direct fluorescence antibody (DFA) conjugate tests that stain the organism with a fluorescent dye.
- This test is unable to distinguish between live and dead bacteria and may have some cross-reactivity with other bacteria.
- Use caution in interpreting the results of DFA tests since the potential exists for both false-positive and -negative results.
- Sample results can be available in one or two days.
DNA Amplification: A relatively new method for rapid, specific detection of
LDB in water employs a polymerase chain reaction (PCR) process to amplify and then detect portions of DNA unique to
LDB.
- This method may produce results in one day.
- Preliminary evidence indicates that
PCR sensitivity and specificity are comparable to those of cell culture, which can take 3 to 14 days to obtain results.
- Further testing may lead to acceptance of this technique as the method of choice for monitoring water sources for contamination.
Test Results:
- Make the results of all water monitoring tests available to building occupants when excessive levels of
LDB are found. Visitors and employees have rights to sampling results as per OSHA Standard
29 CFR 1910.1020(a).
Additional
information (App I:A) on serogroups and subtypes is also
available.
For more information on culture
techniques, see:
|
 Sampling Guidelines Sampling Guidelines |
OSHA Guidelines:
- Use the following suggested guidelines
seen in Table 1. to assess the effectiveness of water system maintenance and to interpret sampling results. These guidelines are based on limited data and are subject to change. They are intended to apply only to water systems being used by healthy individuals and are not necessarily protective for people who are immuno-compromised.
|
Table 1. Colony forming units (CFU) of
LDB per milliliter |
| Action |
Cooling tower/Evaporative Condenser |
Potable water |
Humidifiers and Misters |
1
2 |
100
1,000 |
10
100 |
1
10 |
The levels requiring action vary for the source of exposure, based on the assumption that some routes of exposure result in a greater dose to the lung. For this reason humidifiers and similar devices (such as misters and evaporative condensers) produce aerosol mists and, therefore, need to be controlled to lower levels than cooling towers and domestic water supplies to minimize the risk of inhalation. Levels of
LDB equal to or greater than the values in the table constitute a need for action, as described below:
Action 1
- Cleaning followed by biocide treatment of the system, if appropriate.
Action 2
- Cleaning and or biocide treatment.
- Take immediate steps to prevent employee exposure.
|
**Remember that these numbers are only suggested guidelines, and the goal is zero detectable
LDB in a water source.
[Adapted from George K. Morris and Brian G. Shelton, PathCon Technical Bulletin 1.5, p-2, Legionella Bacteria in Environmental Samples: Hazard Analysis and Suggested Remedial Actions, June 1998, Pathogen Control Associates, 270 Scientific Dr., Suite 3, Norcross, GA 30092] |
Association of Water Technologies (AWT) Guidelines:
- The action plan seen in Table 2. represents a composite compilation of
various AWT
member Water Treatment Company LDB actions plans for cooling tower operations. The frequency of tower
sampling for LDB varies widely amongst the programs and is generally determined
from specific site and system Legionnaires' disease risk assessments.
|
Table 2. Cooling Tower Legionella Count, colony forming units (CFU) per milliliter |
|
>0-10 |
>10-100 |
>100-1000 |
>1000 |
|
a. |
b. |
c. |
d. |
a. Increase biocide addition/s.
b. Increase biocides; review program; retest till <10.
c. Disinfect and clean within 30 days; review program.
d. Disinfect and clean within 7 days; review program. |
For additional information, see:
-
Industry Resources.
Association of Water Technologies
(AWT).
- Legionella 2003: An Update and Statement by the Association of Water Technologies (AWT).
964 KB
PDF, 33 pages.
Accessibility Assistance: Contact the OSHA Directorate of Science, Technology and Medicine at 202-693-2300 for assistance
accessing PDF materials.
|
|
|
|