Introduction
The Brain
Understanding Cancer
Benign and Malignant Brain Tumors
Tumor Grade
Primary Brain Tumors
Secondary Brain Tumors
Brain Tumors: Who's at Risk?
Symptoms
Diagnosis
Treatment
Getting a Second Opinion
Preparing for Treatment
Methods of Treatment
Side Effects of Treatment
Surgery
Radiation Therapy
Chemotherapy
Supportive Care
Rehabilitation
Followup Care
Support for People with Brain Tumors
The Promise of Cancer Research
National Cancer Institute Booklets
National Cancer Institute Information Resources
Introduction
This National Cancer Institute (NCI) booklet (NIH Publication No. 02-1558) has important information
about
brain tumors.* It discusses
possible causes, symptoms, diagnosis, treatment, and followup care.
It also has information to help patients cope with brain tumors.
|
Primary and Secondary Brain Tumors
A tumor that begins in the brain is called a primary
brain tumor. In children, most brain tumors are primary tumors. In
adults, most tumors in the brain have spread there from the lung, breast,
or other parts of the body. When this happens, the disease is
not brain cancer. The tumor in the brain is a secondary tumor.
It is named for the organ or the tissue in which it began.
Treatment for secondary brain tumors depends on where the cancer
started and the extent of the disease.
|
Information specialists at the NCI's
Cancer Information Service
at 1-800-4-CANCER can answer questions about primary
and secondary brain tumors, and they can send NCI materials.
Many NCI publications and fact sheets can be viewed on the Internet at
http://www.cancer.gov/publications. People in the United States and its territories
may use this Web site to order publications. This Web site also explains
how people outside the United States can mail or fax their requests for
NCI publications.
*Words that may be new to readers appear in italics. The
Dictionary section explains these
terms. Some words in the Dictionary have a
"sounds-like" spelling to show how to pronounce them.
Back to Top
The Brain
The brain is a soft, spongy mass of
tissue. It is protected by the bones of
the skull and three thin membranes
called meninges. Watery fluid called
cerebrospinal fluid
cushions the brain. This fluid flows through spaces between the meninges and
through spaces within the brain called ventricles.
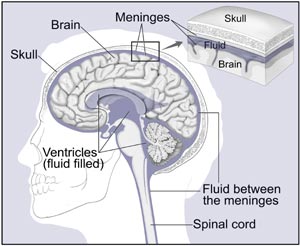
The brain and nearby structures
|
A network of nerves
carries messages back and forth between the brain and the rest of the
body. Some nerves go directly from the brain to the eyes, ears, and
other parts of the head. Other nerves run through the spinal cord to
connect the brain with the other parts of the body. Within the brain
and spinal cord, glial cells
surround nerve cells and
hold them in place.
The brain directs the
things we choose to do (like walking and talking) and the things our body does
without thinking (like breathing). The
brain is also in charge of our senses (sight, hearing, touch, taste, and smell),
memory, emotions, and personality.
The three major parts of the brain control different activities:
Cerebrum—The cerebrum
is the largest part of the brain. It is at the top of the brain. It uses
information from our senses to tell us what is going on around us and tells
our body how to respond. It controls reading, thinking, learning,
speech, and emotions.
The cerebrum is divided into the left and right
cerebral hemispheres,
which control separate activities. The right hemisphere controls the muscles
on the left side of the body. The left hemisphere controls the muscles on
the right side of the body.
Cerebellum—The
cerebellum is under the cerebrum at the back of the
brain. The cerebellum controls balance
and complex actions like walking and talking.
Brain Stem—The brain
stem connects the brain with the spinal cord. It controls hunger and
thirst. It also controls breathing, body temperature, blood pressure, and
other basic body functions.
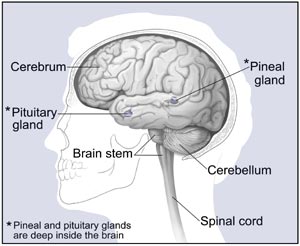
Major parts of the brain
|
Back to Top
Understanding Cancer
Cancer begins in
cells, the building blocks that
make up tissues. Tissues make up the organs of the body.
Normally, cells grow and divide to form new cells as the body needs them.
When cells grow old, they die, and new cells take their place.
Sometimes this orderly process goes wrong. New cells form when the body
does not need them, and old cells do not die when they should. These extra
cells can form a mass of tissue called a growth or tumor.
Back to Top
Benign and Malignant Brain Tumors
Brain tumors can be benign or
malignant:
Back to Top
Tumor Grade
Doctors sometimes group brain tumors by
grade—from low grade
(grade I) to high grade (grade IV). The grade of a tumor refers
to the way the cells look under a microscope.
Cells from high-grade tumors look more abnormal and generally grow
faster than cells from low-grade tumors.
Back to Top
Primary Brain Tumors
Tumors that begin in brain tissue are known as
primary tumors of the
brain. (Information about secondary brain tumors appears in the following
section.) Primary brain tumors are named according to
the type of cells or the part of the brain in which they begin.
The most common primary brain tumors are
gliomas. They begin in glial
cells. There are many types of gliomas:
Astrocytoma—The
tumor arises from star-shaped glial cells called
astrocytes. In adults,
astrocytomas most often arise in the cerebrum. In children, they occur
in the brain stem, the cerebrum, and the cerebellum. A grade III astrocytoma is sometimes called an anaplastic
astrocytoma. A grade IV astrocytoma is usually called a
glioblastoma multiforme.
Brain
stem glioma—The tumor occurs in the lowest part of
the brain. Brain stem gliomas most often are diagnosed in young children
and middle-aged adults.
Ependymoma—The
tumor arises from cells that line the ventricles or the central canal of
the spinal cord. They are most commonly found in children and
young adults.
Oligodendroglioma—This
rare tumor arises from cells that make the fatty substance that covers
and protects nerves. These tumors usually occur in the
cerebrum. They grow slowly and usually
do not spread into surrounding brain tissue.
They are most common in middle-aged adults.
Some types of brain tumors do not begin in glial cells. The most common
of these are:
Medulloblastoma—This
tumor usually arises in the cerebellum. It is the most common
brain tumor in children. It is sometimes called a
primitive neuroectodermal tumor.
Meningioma—This tumor arises in the meninges. It usually grows slowly.
Schwannoma—A tumor
that arises from a Schwann cell.
These cells line the nerve that controls balance and hearing. This nerve is
in the inner ear. The tumor is also called an acoustic
neuroma.
It occurs most often in adults.
Craniopharyngioma—The
tumor grows at the base of the brain, near the
pituitary gland.
This type of tumor most often occurs in children.
Germ cell tumor of
the brain—The tumor arises from a
germ cell. Most germ cell
tumors that arise in the brain occur in people younger than 30. The
most common type of germ cell tumor of the brain is a
germinoma.
Pineal
region tumor—This
rare brain tumor arises in or near the
pineal
gland. The pineal gland is located between
the cerebrum and the cerebellum.
Back to Top
Secondary Brain Tumors
When cancer spreads
from its original place to another part of the body, the new tumor has the same
kind of abnormal cells and the same name as the primary tumor. Cancer
that spreads to the brain from another part of the body is different from a
primary brain tumor. When cancer cells
spread to the brain from another organ (such as the lung or breast), doctors
may call the tumor in the brain a
secondary
tumor or metastatic tumor. Secondary tumors in the brain are far more
common than primary brain tumors.
Back to Top
Brain Tumors: Who's at Risk?
No
one knows the exact causes of brain tumors. Doctors can seldom explain why one
person develops a brain tumor and another does not. However, it is clear that brain tumors are not
contagious. No one can "catch" the
disease from another person.
Research has shown that
people with certain risk factors are
more likely than others to develop a brain tumor. A risk factor is anything that increases a person's chance of
developing a disease.
The following risk factors are associated
with an increased chance of developing a primary brain tumor:
Being male—In general,
brain tumors are more common in males than females. However, meningiomas are more common in females.
Race—Brain tumors
occur more often among white people than among people of other races.
Age—Most brain tumors
are detected in people who are 70 years old or older. However,
brain tumors are the second most common cancer in
children. (Leukemia is the most common childhood
cancer.) Brain tumors are more common in children younger
than 8 years old than in older children.
Family history—People
with family members who have gliomas may be more likely to develop this
disease.
Being exposed to radiation or certain chemicals at work:
Radiation—Workers in
the nuclear industry have an increased risk of developing a brain tumor.
Formaldehyde—Pathologists and
embalmers who work with formaldehyde have an increased risk of developing brain
cancer. Scientists have not found an
increased risk of brain cancer among other types of workers exposed to
formaldehyde.
Vinyl chloride—Workers who make plastics may be exposed to vinyl
chloride. This chemical may increase
the risk of brain tumors.
Acrylonitrile—People who make textiles and plastics may be exposed to
acrylonitrile. This exposure may
increase the risk of brain cancer.
Scientists are
investigating whether cell phones may cause brain tumors. Studies
thus far have not found an increased
risk of brain tumors among people who use cell phones.
Scientists also continue
to study whether head injuries are a risk factor for brain tumors.
So far, these studies have not found an
increased risk among people who have had head injuries.
Most people who have known
risk factors do not get brain cancer.
On the other hand, many who do get the disease have none of these risk
factors. People who think they may be
at risk should discuss this concern with their doctor. The doctor may be able to suggest ways to
reduce the risk and can plan an appropriate schedule for checkups.
Back to Top
Symptoms
The symptoms of
brain tumors depend on tumor size, type, and location. Symptoms may be caused when a tumor presses
on a nerve or damages a certain area of the brain. They also may be caused when the brain swells or fluid builds up
within the skull.
These are the most common symptoms of brain tumors:
Headaches (usually worse in the morning)
Nausea or vomiting
Changes in speech, vision, or hearing
Problems balancing or walking
Changes in mood, personality, or ability to concentrate
Problems with memory
Muscle jerking or twitching (seizures or convulsions)
Numbness or tingling in the arms or legs
These symptoms are not sure signs of a brain tumor. Other
conditions also could cause these problems.
Anyone with these symptoms should see a doctor as soon as
possible. Only a doctor can diagnose and treat the problem.
Back to Top
Diagnosis
If a person has symptoms that suggest a brain tumor, the doctor
may perform one or more of the following procedures:
Physical exam—The doctor checks general signs of health.
Neurologic exam—The
doctor checks for alertness, muscle strength, coordination, reflexes, and
response to pain. The doctor also examines the eyes to look for swelling
caused by a tumor pressing on the nerve that connects the
eye and brain.
CT scan—An x-ray
machine linked to a computer takes a series of detailed pictures of the
head. The patient may receive an injection of a special dye so the brain
shows up clearly in the pictures. The pictures can show tumors in the brain.
MRI—A powerful magnet
linked to a computer makes detailed pictures of areas inside the body.
These pictures are viewed on a monitor and can also be printed. Sometimes a
special dye is injected to help show differences in the tissues of the brain.
The pictures can show a tumor or other problem in the brain.
The doctor may ask for other tests:
Angiogram—Dye
injected into the bloodstream flows into the blood vessels in the brain
to make them show up on an x-ray. If a tumor is present, the doctor may
be able to see it on the x-ray.
Skull x-ray—Some types of brain tumors cause calcium
deposits in the brain or changes in the bones of the skull.
With an x-ray, the doctor can check for these changes.
Spinal tap—The
doctor may remove a sample of cerebrospinal fluid (the fluid that fills
the spaces in and around the brain and spinal cord). This procedure is
performed with local
anesthesia. The doctor uses a long,
thin needle to remove fluid from the spinal column. A spinal tap takes
about 30 minutes. The patient must lie flat for several hours afterward
to keep from getting a headache. A laboratory
checks the fluid for cancer cells or other signs of problems.
Myelogram—This
is an x-ray of the spine. A spinal tap is performed to inject a special
dye into the cerebrospinal fluid. The patient is tilted to allow the dye
to mix with the fluid. This test helps the doctor detect a tumor in
the spinal cord.
Biopsy—The removal
of tissue to look for tumor cells is called a biopsy. A pathologist looks
at the cells under a microscope to check for abnormal cells.
A biopsy can show cancer, tissue changes that may lead to cancer, and
other conditions. A biopsy is the only
sure way to diagnose a brain tumor.
Surgeons can obtain tissue
to look for tumor cells in three ways:
Needle biopsy—The
surgeon makes a small incision in
the scalp and drills a small hole into the skull. This is called a
burr hole. The doctor passes
a needle through the burr hole and removes a sample of tissue from the
brain tumor.
Stereotactic
biopsy—An imaging
device, such as CT or MRI, guides the needle through the burr hole to the
location of the tumor. The surgeon withdraws a sample of tissue
with the needle.
Biopsy at the same time as treatment—Sometimes the surgeon
takes a tissue sample when the patient has
surgery to remove the tumor.
Sometimes a biopsy is not possible. If the tumor is in the brain stem
or certain other areas, the surgeon may not be able to remove tissue from
the tumor without damaging normal brain tissue.
The doctor uses MRI, CT, or other imaging tests instead.
|
A person who needs a biopsy may want to ask the doctor
the following questions:
Why do I need a biopsy? How will the biopsy affect my treatment plan?
What kind of biopsy will I have?
How long will it take? Will I be awake? Will
it hurt?
What are the chances of infection or bleeding
after the biopsy? Are there any
other risks?
How soon will I know the results?
If I do have a brain tumor, who will talk to me
about treatment? When?
|
Back to Top
Treatment
Many people with brain tumors want to take an active part in making
decisions about their medical care. They want to learn all they can about
their disease and their treatment choices. However, shock and stress after
a diagnosis of a brain tumor can make it hard to think of everything to
ask the doctor. It often helps to make a list of questions before an
appointment. To help remember what the doctor says, patients may take
notes or ask whether they may use a tape recorder. Some also want to have
a family member or friend with them when they talk to the doctor—to
take part in the discussion, to take notes, or just to listen.
The doctor may refer the patient to a specialist, or the patient may
ask for a referral. Specialists who treat brain tumors include
neurosurgeons,
neurooncologists,
medical oncologists,
and
radiation oncologists.
The patient may be referred to other health care professionals who work
together as a team. The medical team may include a
nurse,
dietitian,
mental health counselor,
social worker,
physical therapist,
occupational therapist,
and speech therapist.
Children may need tutors to help with schoolwork. (The section on
"Rehabilitation" has more
information about therapists and tutors.)
Back to Top
Getting a Second Opinion
Before starting treatment, the patient might want a second opinion about
the diagnosis and the treatment plan. Some insurance companies require a
second opinion; others may cover a second opinion if the
patient or doctor requests it.
There are a number of ways to find a doctor for a second opinion:
The patient's doctor may refer the patient to one or more specialists.
At cancer centers, several specialists often work together as a team.
The Cancer Information Service, at 1-800-4-CANCER, can
tell callers about nearby treatment centers.
A person with a brain tumor can request a consultation with a team of
specialists in NCI's Neuro-Oncology Branch of the Warren Grant
Magnuson Clinical Center at the National Institutes
of Health in Bethesda, Maryland (301-402-6298).
A local or state medical society, a nearby hospital, or a medical school
can usually provide the names of specialists.
The American Board of Medical Specialties (ABMS) has a list of doctors who have met certain education and training requirements and have passed specialty examinations. The Official ABMS Directory of Board Certified Medical Specialists lists doctors' names along with their specialty and their educational background. The directory is available in most public libraries. Also, ABMS offers this information on the Internet at http://www.abms.org. (Click on "Who's Certified.")
Back to Top
Preparing for Treatment
The doctor can describe treatment choices and discuss the results expected
with each treatment option. The doctor and patient can work
together to develop a treatment plan that fits the patient's needs.
Treatment depends on a number of factors, including the type, location,
size, and grade of the tumor. For some types of brain cancer, the doctor
also needs to know whether cancer cells were found in the
cerebrospinal fluid.
|
These are some questions a person may want to ask the doctor
before treatment begins:
What type of brain tumor do I have?
Is it benign or malignant?
What is the grade of the tumor?
What are my treatment choices? Which do
you recommend for me? Why?
What are the benefits of each kind of treatment?
What are the risks and possible
side
effects of each treatment?
What is the treatment likely to cost?
How will treatment affect my normal activities?
Would a
clinical trial
(research study) be appropriate for me? Can you help
me find one?
|
People do not need to ask all of their questions or understand all of
the answers at one time. They will have other chances to ask the doctor
to explain things that are not clear and to ask for more information.
Back to Top
Methods of Treatment
People with brain tumors have several treatment options. Depending on
the tumor type and stage, patients
may be treated with surgery,
radiation therapy,
or chemotherapy. Some
patients receive a combination of treatments.
In addition, at any stage of disease, patients may have treatment to control
pain and other symptoms of the cancer, to relieve the side effects of therapy,
and to ease emotional problems. This kind of treatment is called
symptom management,
supportive care,
or palliative care.
The doctor is the best person to describe the treatment choices and
discuss the expected results.
A patient may want to talk to the doctor about taking part in a clinical
trial, which is a research study of new treatment methods. The section on
"The Promise of Cancer Research" has more
information about clinical trials.
Surgery is the usual treatment for most brain tumors. Surgery
to open the skull is called a
craniotomy. It is performed
under general anesthesia.
Before surgery begins, the scalp is shaved. The surgeon then makes an
incision in the scalp and uses a special type of saw to remove a piece of
bone from the skull. After removing part or all of the tumor, the surgeon
covers the opening in the skull with that piece of bone or with a piece
of metal or fabric. The surgeon then closes the incision in the scalp.
|
These are some questions a person may want to ask the
doctor before having surgery:
How will I feel after the operation?
What will you do for me if I have pain?
How long will I be in the hospital?
Will I have any long-term effects? Will my hair grow back?
Are there any side effects from using metal or fabric to
replace the bone in the skull?
When can I get back to my normal activities?
What is my chance of a full recovery?
|
Sometimes surgery is not possible. If the tumor is in the brain stem
or certain other areas, the surgeon may not be able to remove the tumor
without damaging normal brain tissue. Patients who cannot have
surgery may receive radiation or other treatment.
Radiation therapy (also called radiotherapy) uses
high-energy rays to kill tumor cells. The radiation
may come from x-rays,
gamma rays,
or protons. A
large machine aims radiation at the tumor and the tissue close
to it. Sometimes the radiation may be directed to the entire
brain or to the spinal cord.
Radiation therapy usually follows
surgery. The radiation kills tumor
cells that may remain in the area.
Sometimes, patients who cannot have
surgery have radiation therapy
instead.
The patient goes to a hospital or clinic for radiation therapy.
The treatment schedule depends on the type and size of the tumor
and the age of the patient. Each treatment lasts only a few minutes.
Doctors take steps to protect the healthy
tissue around the brain tumor:
Fractionation—Radiation
therapy usually is given five days a week for several weeks.
Giving the total dose of radiation over an extended period helps to
protect healthy tissue in the area of the tumor.
Hyperfractionation—The patient gets smaller doses of radiation
two or three times a day instead of a larger amount once a day.
Stereotactic radiation therapy—Narrow beams of radiation are directed
at the tumor from different angles. For
this procedure, the patient wears a rigid head frame. An MRI or CT scan creates pictures of the tumor's exact
location. The doctor uses a computer to
decide on the dose of radiation needed, as well as the sizes and angles of the
radiation beams. The therapy may be given
during a single visit or over several visits.
3-dimensional conformal radiation therapy—A computer
creates a 3-dimensional image of the tumor and nearby brain tissue.
The doctor aims multiple radiation beams to the exact shape of the
tumor. The precise focus of the
radiation beams protects normal brain tissue.
Proton beam radiation therapy—The source of radiation is protons rather than x-rays. The doctor aims the proton beams at the
tumor. Protons can pass through healthy tissue
without damaging it.
|
These are some questions a person may want to ask the
doctor before having radiation therapy:
Why do I need this treatment?
When will the treatments begin? When will they end?
How will I feel during therapy? Are there side effects?
What can I do to take care of myself during therapy?
How will we know if the radiation is working?
Will I be able to continue my normal activities during
treatment?
|
Chemotherapy, the use of drugs to kill cancer cells, is sometimes
used to treat brain tumors. The drugs may be given by mouth or by injection.
Either way, the drugs enter the bloodstream and travel throughout the body.
The drugs are usually given in cycles so that a recovery period follows
each treatment period.
Chemotherapy may be given in an outpatient part of the hospital, at the
doctor's office, or at home. Rarely, the patient may need to stay in
the hospital.
Children are more likely than adults to have chemotherapy. However,
adults may have chemotherapy after surgery and radiation therapy.
For some patients with
recurrent cancer
of the brain, the surgeon removes the tumor and implants
several wafers that contain chemotherapy. Each wafer is about the size
of a dime. Over several weeks, the wafers dissolve, releasing the drug
into the brain. The drug kills cancer cells.
|
Patients may want to ask these questions about
chemotherapy:
Why do I need this treatment?
What will it do?
Will I have side effects? What can I do about them?
When
will treatment start? When will it
end?
How often will I need checkups?
|
Back to Top
Side Effects of Treatment
Because treatment may damage healthy cells and tissues, unwanted side
effects are common. These side effects depend on many factors,
including the location of the tumor and the type and extent of the
treatment. Side effects may not be the
same for each person, and they may even change from one treatment session to
the next. Before treatment starts, the
health care team will explain possible side effects and suggest ways to help
the patient manage them.
The NCI provides helpful booklets about cancer treatments and coping with
side effects, such as
Radiation Therapy and You,
Chemotherapy and You,
and Eating Hints for Cancer Patients.
See the sections "National Cancer Institute
Information Resources" and "National Cancer Institute Booklets"
for other sources of information about side effects.
Back to Top
Surgery
Patients often have a headache or are uncomfortable for the first few
days after surgery. However, medicine can usually control their
pain. Patients should feel free to discuss pain relief with the doctor
or nurse.
It is also common for patients to feel tired or weak. The length of time
it takes to recover from an operation varies for each patient.
Other, less common,
problems may occur. Cerebrospinal fluid
or blood may build up in the brain.
This swelling is called edema.
The health care team monitors the patient
for signs of these problems. The
patient may receive steroids to help
relieve swelling. A second surgery may
be needed to drain the fluid. The
surgeon may place a long, thin tube
(shunt)
in a ventricle of the brain. The tube
is threaded under the skin to another part of the body, usually the
abdomen. Excess fluid is carried from
the brain and drained into the abdomen.
Sometimes the fluid is drained into the heart instead.
Infection is another problem that may develop after surgery.
If this happens, the health care team gives the patient an
antibiotic.
Brain surgery may damage normal tissue. Brain
damage can be a serious problem. The patient may have
problems thinking, seeing, or speaking. The patient
also may have personality changes or seizures. Most
of these problems lessen or disappear with time.
But sometimes damage to the brain is permanent. The
patient may need physical therapy,
speech therapy, or occupational therapy.
Back to Top
Radiation Therapy
Some patients have nausea for several hours after treatment. The
health care team can suggest ways to help patients cope with this
problem. Radiation therapy also may cause patients to become very
tired as treatment continues. Resting is important, but doctors
usually advise patients to try to stay as active as they can.
In addition, radiation therapy commonly causes hair loss. Hair
usually grows back within a few months. Radiation therapy also may
affect the skin in the treated area. The scalp and ears may become
red, dry, and tender. The health care team can suggest ways to relieve
these problems.
Sometimes radiation therapy causes brain tissue to swell.
Patients may get a headache or feel pressure. The health care team
watches for signs of this problem. They can provide medicine to reduce
the discomfort.
Radiation sometimes kills healthy brain tissue. This side effect
is called radiation necrosis.
Necrosis can cause headaches, seizures, or even the patient's death.
In children, radiation may damage the pituitary gland and other areas
of the brain. This could cause learning problems or slow down growth and
development. In addition, radiation during childhood increases the risk
of secondary tumors later in life. Researchers are studying whether
chemotherapy may be used instead of radiation therapy in young children
with brain tumors.
Side effects may be worse if chemotherapy and radiation therapy are
given at the same time. The doctor can suggest ways to ease these
problems.
Back to Top
Chemotherapy
The side effects of chemotherapy depend mainly on the drugs that
are used. The most common side effects include fever and chills, nausea
and vomiting, loss of appetite, and weakness. Some side effects may be
relieved with medicine.
Patients who receive an implant (a wafer) that contains a drug are
monitored by the health care team for signs of infection after surgery.
An infection can be treated with an antibiotic.
Back to Top
Supportive Care
At any stage of disease, people with brain tumors receive supportive
care to prevent or control problems and to improve their comfort and
quality of life
during treatment. Patients may have treatment to control pain and other
symptoms of a brain tumor, to relieve the side effects of therapy, and
to ease emotional problems.
These are common types of supportive care for people with brain tumors:
Steroids—Most patients with brain tumors
need steroids to help relieve swelling of the brain.
Anticonvulsant medicine—Brain
tumors can cause seizures. Patients
may take an anticonvulsant medicine
to prevent or control seizures.
Shunt—If fluid builds up in the brain, the
surgeon may place a shunt to drain the fluid.
Information about shunts is under "Surgery"
in the "Side Effects" section.
Many people with brain tumors receive supportive care along with
treatments intended to slow the progress of the disease. Some decide
not to have antitumor treatment and receive only supportive care to manage
their symptoms.
Back to Top
Rehabilitation
Rehabilitation can be a very important part of the treatment plan.
The goals of rehabilitation depend on the person's needs and how
the tumor has affected daily activities.
The health care team makes every effort to help the patient return to
normal activities as soon as possible.
Several types of therapists can help:
Physical therapists—Brain tumors and their treatment
may cause paralysis.
They may also cause weakness and problems with balance. Physical
therapists help patients regain strength and balance.
Speech therapists—Speech therapists help patients
who have trouble speaking, expressing thoughts, or swallowing.
Occupational therapists—Occupational therapists help
patients learn to manage activities of daily living, such as eating,
using the toilet, bathing, and dressing.
Children with brain tumors may have special needs. Sometimes children
have tutors in the hospital or at home. Children who have problems learning or
remembering what they learn may need tutors or special classes when they return
to school.
Back to Top
Followup Care
Regular followup is very important after treatment for a brain tumor.
The doctor checks closely to make sure that the tumor has not returned.
Checkups may include careful physical and neurologic exams. From time
to time, the patient may have MRI or CT scans. If the patient has a shunt,
the doctor checks to see that it is working well. The doctor can explain
the followup plan—how often the patient must visit the doctor and
what tests will be needed.
The NCI has prepared a booklet for people who have completed their
treatment to help answer questions about followup care and other concerns.
Facing Forward Series: Life After Cancer Treatment
provides tips for making the best use of medical visits. It describes the
kinds of help people may need.
Back to Top
Support for People with Brain Tumors
Living with a serious disease such as a brain tumor is not easy. Some people
find they need help coping with the emotional and practical aspects of their
disease. Support groups can help. In these groups, patients or their family
members get together to share what they have learned about coping with the
disease and the effects of treatment. Patients may want to talk with a member
of their health care team about finding a support group. Groups may offer
support in person, over the telephone, or on the Internet.
People living with a brain tumor may worry about caring for their
families, keeping their jobs, or
continuing daily activities. Concerns
about treatments and managing side effects, hospital stays, and medical bills
are also common. Doctors, nurses, and
other members of the health care team can answer questions about treatment,
working, or other activities. Meeting
with a social worker, counselor, or member of the clergy can be helpful to
those who want to talk about their feelings or discuss their concerns. Often,
a social worker can suggest resources
for financial aid, transportation, home care, or emotional support.
The Cancer Information
Service can provide information to help patients and their families locate
programs, services, and publications.
Back to Top
The Promise of Cancer Research
Doctors all over the country are
conducting many types of clinical trials. These are research studies in which
people take part voluntarily. Studies
include new ways to treat brain tumors.
Research has already led to advances, and researchers continue to search
for more effective approaches.
Patients who join these studies have the
first chance to benefit from treatments that have shown promise in earlier
research. They also make an important
contribution to medical science by helping doctors learn more about the disease. Although clinical trials may pose some
risks, researchers take very careful steps to protect their patients.
Researchers are
testing new anticancer drugs, doses, and treatment schedules. They are working with various drugs and drug
combinations, as well as combinations of drugs and radiation therapy. They also are testing new methods and
schedules of radiation therapy.
Patients who are interested in being part of a clinical
trial should talk with their doctor.
They may want to read the NCI booklet Taking Part in Cancer Treatment Research Studies. It explains how clinical trials are carried out and explains their possible benefits and risks. NCI's Web site
includes a section on clinical trials at http://www.cancer.gov/clinicaltrials. This section of the Web site provides
general information about clinical trials.
It also offers detailed information about ongoing studies of treatment
for brain tumors. The Cancer
Information Service at 1-800-4-CANCER can answer questions and provide
information about clinical trials.
Back to Top
National Cancer Institute Booklets
National Cancer Institute (NCI) publications can be ordered by writing
to the address below, and some can be viewed and downloaded from
http://www.cancer.gov/publications
on the Internet.
Publications Ordering Service
National Cancer Institute
Suite 3036A
6116 Executive Boulevard, MSC 8322
Bethesda, MD 20892-8322
In addition, people in the United States and its
territories may order these and other NCI booklets by calling the Cancer
Information Service at 1-800-4-CANCER.
They may also order many NCI publications on-line at
http://www.cancer.gov/publications.
See the complete index of What You Need To Know About™ Cancer publications.
Booklets About Cancer Treatment
Booklets About Living With Cancer
Back to Top
National Cancer Institute Information Resources
You may want more information for yourself, your family, and your doctor. The following National Cancer Institute (NCI) services are available to help you.
Cancer Information Service (CIS)
Provides accurate, up-to-date information on cancer to patients and their families, health professionals, and the general public. Information specialists translate the latest scientific information into understandable language and respond in English, Spanish, or on TTY equipment.
Toll-free: 1-800-4-CANCER (1-800-422-6237)
TTY (for deaf and hard of hearing callers): 1-800-332-8615
The NCI's Cancer.gov™ Web site provides information from numerous
NCI sources. It offers current information on cancer prevention, screening,
diagnosis, treatment, genetics, supportive care, and ongoing clinical trials.
It also provides information about NCI's research programs and funding
opportunities, cancer statistics, and the Institute itself. Cancer.gov can be accessed at
http://www.cancer.gov on the Internet.
Cancer.gov also provides live, online assistance through LiveHelp.
Information specialists are available Monday through Friday from 9:00 AM
to 10:00 PM Eastern Time. LiveHelp is at
http://www.cancer.gov on the Internet.
Back to Top
|