 |
 |
 |

'Biomarkers' May Help Spot, Track Alzheimer's
A number of molecules in blood and spinal fluid seem likely candidates, researchers say|
|
HealthDay
Tuesday, July 29, 2008
 TUESDAY, July 29 (HealthDay News) -- Scientists may be succeeding in the hunt for biomarkers for Alzheimer's disease.
TUESDAY, July 29 (HealthDay News) -- Scientists may be succeeding in the hunt for biomarkers for Alzheimer's disease.
A biomarker -- something that can be measured and that gives an indication of what's going on inside the body -- will help in early detection, in testing new therapies and, once doctors have better drugs for Alzheimer's, with earlier intervention in the disease process.
"If we're going to have any kind of medication that alters or modifies the disease, if it's really going to change it rather than treat symptoms, then we need biomarkers that are sensitive to the illness before a person becomes impaired," explained Dr. Gary Kennedy, director of geriatric psychiatry at Montefiore Medical Center in New York City. "In Alzheimer's, we need two things: We need to know who's sick and who's not and, secondly, biomarkers should be treatment-sensitive, meaning if you've got the right treatment, you watch the biomarker go down, like blood sugar and insulin. That's the model we want."
One study being presented at the International Conference on Alzheimer's Disease (ICAD) in Chicago found that differences in levels of CD-69, a protein involved in white blood cell growth and production, allowed researchers to distinguish between people with Alzheimer's, people with Parkinson's-related dementia and those who were cognitively normal.
The study, from researchers at the University of Leipzig in Germany, was based on a theory that Alzheimer's occurs when neurons get a false signal to divide. The more popular theory holds that a build-up of amyloid plaque (made up mostly of beta amyloid protein) in the brain causes Alzheimer's.
"The alternative theory about Alzheimer's is that the [cell] replication process gets triggered pathologically, and then the cells are programmed to die, and that's what's killing the nerve cells, not the amyloid," Kennedy explained. "[This study] all hinges on the theory that it's a false signal to replicate that starts these neurons down the path to killing themselves."
But investigators still have a long way to go. "It's one thing to distinguish the sick group from the healthy group and another to see if you can predict from the healthy group who gets the disease," Kennedy said. "That's the real proof of the pudding."
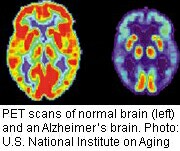
A second study, from researchers at Washington University in St. Louis, confirmed previous findings: that the more amyloid there is in the brain (as measured by PET scans), the less beta amyloid 42 there is in cerebrospinal fluid (CSF). Beta amyloid 42 is an extra-"sticky" type of amyloid protein which accumulates and forms plaques. The theory is that measurements of beta amyloid 42 in spinal fluid could serve as a marker for Alzheimer's disease.
Another study, this time from a team in Ireland and in Germany, found that individuals with mild cognitive impairment (MCI), often considered a transitional stage between normal cognitive functioning and Alzheimer's, had elevated levels of beta-secretase (BACE1) activity in the brain when compared both to healthy people and people with Alzheimer's.
Finally, a fourth study showed that a certain radioactive compound or tracer, 18F-AV-45, may have potential in the diagnosis and early detection of Alzheimer's when used with PET scans. Trials of the substance, conducted by Philadelphia-based Avid Radiopharmaceuticals Inc., are ongoing.
HealthDay
Copyright (c) 2008 ScoutNews, LLC. All rights reserved.
Related News:
More News on this Date
Related MedlinePlus Pages:
| Home | Health Topics | Drugs & Supplements | Encyclopedia | Dictionary | News | Directories | Other Resources | |
| Disclaimers | Copyright | Privacy | Accessibility | Quality Guidelines U.S. National Library of Medicine, 8600 Rockville Pike, Bethesda, MD 20894 National Institutes of Health | Department of Health & Human Services |
Date last updated: 30 July 2008 |




