Agency for Toxic Substances and Disease Registry
Radiation Exposure from Iodine 131
Clinical Evaluation (continued)
- Initial laboratory evaluation should include a serum thyroid stimulating hormone (TSH) level.
No evaluation of the thyroid gland is complete without a structural assessment (physical exam) and a functional assessment (blood analysis to determine the TSH level). Thyroid function tests are mandatory for evaluation of a thyroid nodule; however, these tests do not differentiate between benign and malignant nodules.
- Screening patients for thyroid effects of I-131 is different from evaluating a known thyroid nodule.
In screening programs, it is important to test for the noncancerous effects of I-131. The serum TSH level should be obtained to identify those patients with thyroid gland dysfunction. If TSH is abnormal, serum free thyroxine (FT4) and levothyroxine (T3) levels should be measured. Most patients with thyroid cancer are euthyroid (their thyroid glands function normally), and it is rare for a patient with thyroid cancer to have an abnormal TSH level.
Chronic autoimmune thyroiditis can be found with an increased TSH level and a thyroid nodule or bilateral nodules. Serum antithyroid peroxidase antibody and antithyroglobulin antibody levels can assist in the diagnosis of chronic autoimmune thyroiditis. However, the diagnosis of chronic autoimmune thyroiditis does not exclude the presence of cancer within the thyroid gland. Serum calcium levels should be assessed because of the risk for hyperparathyroidism after I-131 exposure. If the calcium level is abnormal, measure parathyroid hormone and phosphorus.
Ultrasound is useful to determine the size and physical characteristics of a nodule once it has been identified. However, ultrasound cannot differentiate benign from malignant nodules and therefore is not required in the evaluation of a palpable thyroid nodule.
Your patient's lab results were as follows:
- TSH was elevated at 7.0 nanograms per milliliter (ng/mL) (normal 0.36-4.7 ng/mL).
- FT4 was 0.83 (normal 0.83 to 1.44) and T3 resin uptake was 1.2 micrograms per deciliter (µg/dL) (normal 0.8-1.2 µg/dL).
- Calcitonin was 15 picograms per milliliter (pg/mL) (normal < 20 pg/mL).
- Calcium was 9.1 milligrams per deciliter (mg/dL) (normal 8.5-10.4 mg/dL); ionized calcium was 1.30 millimoles per liter (mmol/L) (normal 1.16-1.32 mmol/L).
- Phosphorus was 2.9 mg/dL (normal 2.8-4.6 mg/dL).
- Parathyroid hormone was 50 pg/mL (normal 10-65 pg/mL).
A thyroid ultrasound showed a heterogeneous gland with multiple small cysts and one 1 cm 1-cm cyst in the left lobe.
- Fine needle aspiration biopsy is the procedure of choice for evaluating whether or not a thyroid nodule is malignant.
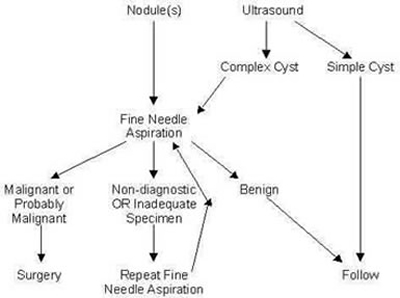
The challenge to clinicians is to distinguish benign nodules from malignant tumors. The prevalence of clinical thyroid cancer in the general population is significantly less than 1%, and the majority of nodules are benign. Fine needle aspiration biopsy (FNAB) is the procedure of choice for evaluating a palpable nodule. The technique is simple and generally free of complications when performed by an experienced physician with appropriate training. If a nodule is found with ultrasound, the physician must differentiate between a simple cyst and a complex cyst. A simple cyst will require followup. A complex cyst must undergo an FNAB. If the results of the cytologic examination indicate the nodule is benign, no further testing is required but followup should be on an annual basis. Nondiagnostic results call for a repeat of the FNAB. Diagnosis of a malignancy or a probable malignancy requires surgery. (Figure 2 illustrates the process of nodule evaluation.)
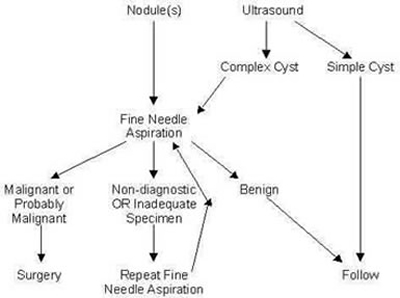
Figure 2. Evaluation of a Euthyroid Nodule
FNAB is reportedly superior to all other techniques for diagnosing thyroid cancer. The use of FNAB can reduce the number of unnecessary surgical operations for suspicious nodules that prove to be benign. It is also the procedure of choice for evaluating a complex cyst after it has been identified on ultrasound imaging of the thyroid gland. Very few palpable thyroid nodules are actually simple cysts (defined as a cystic structure with no internal echoes and no evidence of thickening of the cyst wall). Most palpable thyroid nodules are solid nodules with cystic components. A simple cyst is almost always benign. Occasionally, cancer is found in the wall of the cyst. For this reason, recurrent cysts should be imaged by ultrasound. Surgical evaluation is indicated if evidence exists for a separate lesion or growth in the wall of the cyst.
FNAB for cytology with ultrasound guidance is often a diagnostic procedure; when the nodule is cystic, FNAB might also be curative. A satisfactory aspirate specimen combined with an accurate cytology evaluation by a cytopathologist provides a reliable means of differentiating between a benign and malignant nodule in all but highly cellular or follicular lesions. FNAB does not allow for differentiating Hashimoto disease from lymphoma of the thyroid. This can be done using a combination of FNAB cytology and clinical evaluation. A "nondiagnostic" specimen should be followed up with a repeat FNAB. A nodule that gives persistently nondiagnostic FNAB results should be surgically removed.
In general, 20% to 30% of patients are referred for surgical evaluation on the basis of FNAB cytologic features.
Diagnosis and classification of thyroid cancers are performed by cytology. The most efficient way of screening for thyroid malignancy in a patient is to elicit a thorough history and perform a careful physical examination, followed by an FNAB and interpretation of the specimen by an experienced cytopathologist. Neck ultrasound is an ideal technique for establishing whether a palpable cervical mass is within or adjacent to the thyroid, and for differentiating thyroid nodules from other neck masses such as cystic hygromas, thyroglossal duct cysts, and enlarged lymph nodes. Papillary thyroid cancer is the most common type of cancer found among the population exposed to I-131 releases in Chernobyl.
The patient in the case study was diagnosed with mild hypothyroidism and prescribed levothyroxine (50 µg/day). She was seen 1 month later; test results revealed TSH of 3.1 ng/mL (normal 0.36-4.7 ng/mL). She had lost 3 pounds and felt less tired.
| 9. |
What are the recommendations for managing a thyroid nodule found to be benign by FNAB in a patient with a history of exposure to I-131? |
| 10. |
Are the patient and the rest of her family at increased risk for cancer? Is there increased risk for any other disease? Were there any risks to her daughter's unborn child because of the patient's (and potentially the daughter's) past exposure to I-131? |
Previous Section Next Section
|