

25
Lead Agency: | Centers for Disease Control and Prevention |
[Note: The National Library of Medicine has provided PubMed links to available references that appear at the end of this focus area document.]
Contents
Interim Progress Toward Year 2000 Objectives
Healthy People 2010—Summary of Objectives
Healthy People 2010 Objectives
 Bacterial STD Illness and Disability
Bacterial STD Illness and Disability
 Viral STD Illness and Disability
Viral STD Illness and Disability
 STD Complications Affecting Females
STD Complications Affecting Females
 STD Complications Affecting the Fetus and
Newborn
STD Complications Affecting the Fetus and
Newborn
 Community Protection Infrastructure
Community Protection Infrastructure
Related Objectives From Other Focus Areas
Promote responsible sexual behaviors, strengthen community capacity, and increase access to quality services to prevent sexually transmitted diseases (STDs) and their complications.
Sexually transmitted diseases (STDs) refer to the more than 25 infectious organisms transmitted primarily through sexual activity. STDs are among many related factors that affect the broad continuum of reproductive health agreed on in 1994 by 180 governments at the International Conference on Population and Development (ICPD). At ICPD, all governments were challenged to strengthen their STD programs.[1] STD prevention as an essential primary care strategy is integral to improving reproductive health.
Despite the burdens, costs, complications, and preventable nature of STDs, they remain a significant public health problem, largely unrecognized by the public, policymakers, and public health and health care professionals in the United States. STDs cause many harmful, often irreversible, and costly clinical complications, such as reproductive health problems, fetal and perinatal health problems, and cancer. In addition, studies of the worldwide human immunodeficiency virus (HIV) pandemic link other STDs to a causal chain of events in the sexual transmission of HIV infection.[2] (See Focus Area 13. HIV.)
A 1997 Institute of Medicine (IOM) report characterized STDs as “hidden epidemics of tremendous health and economic consequence in the United States” and stated, “STDs represent a growing threat to the Nation’s health and that national action is urgently needed.”3 IOM’s principal conclusion was that the United States needs to establish a much more effective national system for STD prevention, which takes into account the complex interaction between biological and social factors that sustain STD transmission in populations; focuses on preventing the disproportionate effect that STDs have on some population groups; applies proven, cost-effective behavioral and biomedical interventions; and recognizes that education, mass communication media, financing, and health care infrastructure policies must foster change in personal behaviors and in health care services.[3] (See Focus Area 23. Public Health Infrastructure.)
Biological factors. STDs are behavior-linked diseases that result from unprotected sex.3 Several biological factors contribute to their rapid spread.
Asymptomatic nature of STDs. The majority of STDs either do not produce any symptoms or signs, or they produce symptoms so mild that they often are disregarded, resulting in a low index of suspicion by infected persons who should, but often do not, seek medical care. For example, as many as 85 percent of women and up to 50 percent of men with chlamydia have no symptoms.[4], [5], [6], [7] A person infected with HIV may be asymptomatic and may transmit the disease to another person. That person may, in turn, be infected for years but remain unaware until symptoms manifest themselves.
Lag time between infection and complications. Often, a long interval—sometimes years—occurs between acquiring a sexually transmitted infection and recognizing a clinically significant health problem. Examples are cervical cancer caused by human papillomavirus (HPV), liver cancer caused by hepatitis B virus infection,[8] and infertility and ectopic pregnancy resulting from unrecognized or undiagnosed chlamydia or gonorrhea.[9] The original infection often is asymptomatic, and, as a result, people frequently do not perceive a connection between the original sexually acquired infection and the resulting health problem.
Gender and age. Women are at higher risk than men for most STDs, and young women are more susceptible to certain STDs than are older women. The higher risk is partly because the cervix of adolescent females is covered with cells that are especially susceptible to STDs, such as chlamydia.[10]
Social and behavioral factors. The spread of STDs, especially in certain vulnerable population groups, is directly affected by social and behavioral factors. Social and cultural factors may cause serious obstacles to STD prevention by adversely influencing social norms regarding sex and sexuality.
Poverty and marginalization. STDs disproportionately affect disenfranchised persons and persons who are in social networks in which high-risk sexual behavior is common and either access to care or health-seeking behavior is compromised. Some disproportionately affected groups include sex workers (people who exchange sex for money, drugs, or other goods), adolescents, persons in detention, and migrant workers.3 Without publicly supported STD services, many people in these categories would lack access to STD care.
Substance abuse, sex work, and STDsare closely connected, and substance abuse and sex work frequently are causes for arrest and detention. Studies show that comprehensive screening of incarcerated populations can be done successfully and safely within the criminal justice system.[11], [12], [13] Discussed below are several connected themes relevant to any discussion of poverty and marginalization issues.
Access to health care. Access to high-quality health care is essential for early detection, treatment, and behavior-change counseling for STDs. Often, groups with the highest rates of STDs are the same groups in which access to health services is most limited. This limitation relates to (1) lacking access to publicly supported STD clinics (present in only 50 percent of U.S. public health jurisdictions),[14] (2) having no health care coverage, (3) having coverage that imposes a copayment or deductible, or (4) having coverage that excludes the basic preventive health services that help avert STDs or their complications. (See Focus Area 1. Access to Quality Health Services.)
Substance abuse.Many studies document the association of substance abuse, especially the abuse of alcohol and drugs, with STDs.[15] At the population level, the introduction of new illicit substances into communities often can drastically alter sexual behavior in high-risk sexual networks, leading to the epidemic spread of STDs.[16] Behavioral factors that can increase STD transmission in a community include increases in the exchange of sex for drugs, increases in the number of anonymous sex partners, decreases in motivation to use barrier protection, and decreases in attempts to seek medical treatment. The nationwide syphilis epidemic of the late 1980s, for example, was fueled by increased crack cocaine use.[17] Other substances, including alcohol, may affect an individual’s cognitive and negotiating skills before and during sex, lowering the likelihood that protection against STD transmission and pregnancy will be used.
Sexual coercion. Analysis of adolescent female sexual activity reveals the frequency of coercive behaviors and brings to light that not all young women enter sexual relationships as willing partners.[18] In fact, sexual coercion is a major problem for significant numbers of young women in the United States. In 1995, 16 percent of females whose first sexual intercourse took place when they were aged 15 years or under reported that it was not voluntary.[19] This aspect of adolescent sexual behavior demands increased national and local attention, both for social justice and for health reasons. Sexual violence against women contributes both directly and indirectly to STD transmission. Directly, women experiencing sexual violence are less able to protect themselves from STDs or pregnancy. Indirectly, research demonstrates that women with a history of involuntary sexual intercourse are more likely to have voluntary intercourse at earlier ages—a known risk factor for STDs—than women who are not sexually abused.[20]
Sexuality and secrecy.Perhaps the most important social factor contributing to the spread of STDs in the United States and the factor that most significantly separates the United States from those industrialized countries with low rates of STDs is the stigma associated with STDs and the general discomfort of people in the United States with discussing intimate aspects of life, especially those related to sex.[21] Sex and sexuality pervade many aspects of the Nation’s culture, and people in the United States are fascinated with sexual matters. Paradoxically, while sexuality is considered a normal aspect of human functioning, people in the United States nevertheless are secretive and private about their sexual behavior. Talking openly and comfortably about sex and sexuality is difficult even in the most intimate relationships. One survey showed that, for married couples, about one-fourth of women and one-fifth of men had no knowledge of their partner’s sexual history.[22] In its study, IOM stated, “The secrecy surrounding sexuality impedes sexuality education programs for adolescents, open discussion between parents and their children and between sex partners, balanced messages from mass media, education and counseling activities of health care professionals, and community activism regarding STDs.”[23]
Changing sexual behaviors and sexual norms will be an important part of any long-term strategy to develop a more effective national system of STD prevention in the United States. A new sexual openness needs to become the norm to ensure that all sexual relationships are consensual, nonexploitive, and honest and to protect against disease and unintended pregnancy. This openness would allow (1) parents to talk frankly and comfortably with their children, and teachers and counselors with their students, about responsible behavior and avoiding risks (for example, abstaining from intercourse, delaying initiation of intercourse, reducing the number of sex partners, and increasing the use of effective barrier contraception), (2) sex partners to talk openly about safe behaviors, and (3) health care providers to talk comfortably and knowledgeably with patients about sexuality and sexual risk, to counsel them about risk avoidance, and to screen them regularly for STDs when indicated.[24] (See Focus Area 11. Health Communication.)
The entertainment industry, particularly television, has noticed interest in sexual themes. While people in the United States are bombarded by sexual messages and images, very little informed, high-quality STD prevention advice or discussion exists regarding contraception, sexuality, or the risks of early, unprotected sexual behavior. Popular television programs depict as many as 25 instances of sexual behaviors for every 1 instance of protected behavior or discussion about STDs or pregnancy prevention.[25]Media companies can play an important part in reshaping sexual behaviors and norms in the United States in the next decade.
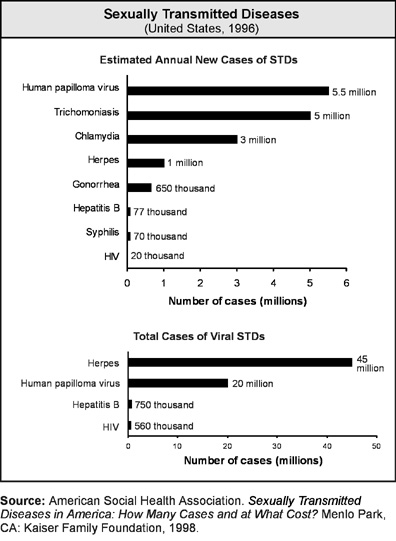
STDs are common, costly, and preventable. Worldwide, an estimated 333 million cases of curable STDs occur annually.[26] In 1995, STDs were the most common reportable diseases in the United States.[27] They accounted for 87 percent of the top 10 infections most frequently reported to the Centers for Disease Control and Prevention (CDC) from State health departments. Of the top 10 infections, 5 were STDs (chlamydia, gonorrhea, AIDS, syphilis, and hepatitis B). Each year an estimated 15 million new STD infections occur in the United States, and nearly 4 million teenagers are infected with an STD.[28] The direct and indirect costs of the major STDs and their complications, including sexually transmitted HIV infection, are conservatively estimated at $17 billion annually.3
Despite recent progress toward controlling some STDs, when compared to other industrialized nations, the United States has failed to go far enough or fast enough in its national attempt to contain acute STDs and STD-related complications.3 STD rates in this Nation exceed those in all other countries of the industrialized world (including the countries of western and northern Europe, Canada, Japan, and Australia). Through a sustained, collaborative, multifaceted approach, other countries have reduced significantly the burden of STDs on their citizens, an accomplishment the United States also should strive to achieve.
All racial, cultural, economic, and religious groups are affected by STDs. People in all communities and sexual networks are at risk for STDs. Nevertheless, some population groups are disproportionately affected by STDs and their complications.
Gender disparities. Women suffer more frequent and more serious STD complications than men do. Among the most serious STD complications are pelvic inflammatory disease (PID), ectopic pregnancy, infertility, and chronic pelvic pain.[29] Women are biologically more susceptible to infection when exposed to a sexually transmitted agent. Often, STDs are transmitted more easily from a man to a woman.[30] Acute STDs (and even some complications) often are very mild or are completely asymptomatic in women. STDs are more difficult to diagnose in women due to the physiology and anatomy of the female reproductive tract. This combination of increased susceptibility and “silent” infection frequently can result in women being unaware of an STD, which results in delayed diagnosis and treatment.
STDs in pregnant women can cause serious health problems or death to the fetus or newborn.[31] Sexually transmitted organisms in the mother can cross the placenta to the fetus or newborn, resulting in congenital infection, or these organisms can reach the newborn during delivery, resulting in perinatal infections. Regardless of the route of infection, these organisms can permanently damage the brain, spinal cord, eyes, auditory nerves, or immune system. Even when the organisms do not reach the fetus or newborn directly, they can significantly complicate the pregnancy by causing spontaneous abortion, stillbirth, premature rupture of the membranes, or preterm delivery.[32] For example, women with bacterial vaginosis are 40 percent more likely to deliver a preterm, low birth weight infant than are mothers without this condition.[33], [34] (See Focus Area 16. Maternal, Infant, and Child Health.)
Age disparities. For a variety of behavioral, social, and biological reasons, STDs also disproportionately affect adolescents and young adults.[35] In 1997, females aged 15 to 19 years had the highest reported rates of both chlamydia and gonorrhea among women; males aged 20 to 24 years had the highest reported rates of both chlamydia and gonorrhea among men.[36] The herpes infection rate of white youth aged 12 to 19 years increased nearly fivefold from the period 1976–80 to the period 1988–94.[37] Indeed, because not all teenagers are sexually active, the actual rate of STDs in teens is probably higher than the observed rates suggest.10 There are several contributing factors:
n | Sexually active teenagers are at risk for STDs. In 1995, 50 percent of females aged 15 to 19 years interviewed for the National Survey of Family Growth (NSFG) indicated that they had had sexual intercourse.19 In the same year, 54 percent of adolescent males in high school reported having had sexual intercourse, including 49 percent of white males, 62 percent of Hispanic males, and 81 percent of African American males.[38] |
n | Teenagers are increasingly likely to have more sex partners at earlier ages. Compounding this factor is the fact that these partners are active in sexual networks already highly infected with untreated STDs.36 In 1971, 39 percent of sexually active adolescent females aged 15 to 19 years had more than one sex partner; in 1988 the percentage had increased to 62 percent.[39] |
n | Sexually active teenagers often are reluctant to obtain STD services, or they may face serious obstacles when trying to obtain them. In addition, health care providers often are uncomfortable discussing sexuality and risk reduction with their patients, thus missing opportunities to counsel and screen young people for STDs.3 |
Racial and ethnic disparities. Certain racial and ethnic groups (mainly African American and Hispanic populations) have high rates of STDs, compared with rates for whites. Race and ethnicity in the United States are risk markers that correlate with other fundamental determinants of health status, such as poverty, limited or no access to quality health care, fewer attempts to get medical treatment, illicit drug use, and living in communities with a high number of cases of STDs. National surveillance data may overrepresent STDs in racial and ethnic groups that are more likely to receive STD services from public-sector STD clinics where timely and complete illness reporting is generally the rule. However, studies using random sampling techniques document higher rates of STDs in marginalized populations, particularly African Americans as compared with whites.37 Surveillance data from 1997 show:36
n | Although chlamydia is a widely distributed STD in population groups, it occurs more frequently in certain racial and ethnic groups. |
n | African Americans (non-Hispanic blacks) accounted for about 77 percent of the total number of reported cases of gonorrhea—31 times the rate in whites (non-Hispanic whites). African American rates were on average about 24 times higher than those of white adolescents aged 15 to 19 years; the rate for African Americans aged 20 to 24 years was almost 28 times greater than that in whites. Gonorrhea rates in Hispanic persons were nearly three times the rate in whites. |
n | The most recent syphilis epidemic occurred largely in heterosexual minority populations. Since 1990, rates of primary and secondary (P&S) syphilis have declined in all racial and ethnic groups except American Indians or Alaska Natives. However, rates for African Americans and Hispanics continue to be higher than those for whites. In 1997, African Americans accounted for about 82 percent of all reported cases of P&S syphilis. |
n | In 1997, the rate of congenital syphilis was 113.5 per 100,000 live births in African Americans and 34.6 per 100,000 live births in Hispanics, compared with 3.3 per 100,000 live births in whites. |
Finally, young heterosexual women, especially minority women, are increasingly acquiring HIV infection and developing AIDS. In 1998, 41 percent of reported AIDS cases in persons aged 13 to 24 years occurred in young women, and more than four of every five AIDS cases reported in women occurred in certain racial and ethnic groups (mostly African American or Hispanic).[40] The U.S. spread of HIV infection through heterosexual transmission closely parallels other STD epidemics.2
Compelling worldwide evidence indicates that the presence of other STDs increases the likelihood of both transmitting and acquiring HIV infection.2 Prospective epidemiologic studies from four continents, including North America, have repeatedly demonstrated that when other STDs are present, HIV transmission is at least two to five times higher than when other STDs are not present. Biological studies demonstrate that when other STDs are present, an individual’s susceptibility to HIV infection is increased, and the likelihood of a dually infected person (having HIV infection and another STD) infecting other people with HIV is increased. Conversely, effective STD treatment can slow the spread of HIVat the individual and community levels.
Prevention opportunities arise from an understanding of STD transmission dynamics. The rate of STD infection in a population is determined by the interaction of three principal factors:[41], [42]
n | The rate at which uninfected individuals have sex with infected persons (rate of sex partner exchange or exposure). |
n | The probability that a susceptible exposed person actually will acquire the infection (transmission). |
n | The time period during which an infected person remains infectious and able to spread disease to others (duration). |
Effective STD prevention requires effective population-level and individual-level interventions that can alter the natural course of these factors. IOM advised in its report, “Use of available information and interventions could have a rapid and dramatic impact on the incidence and prevalence of STDs in the United States. Many effective and efficient behavioral and biomedical interventions are available.”3
Behavioral interventions can be brought to bear on exposure, transmission, and duration factors. They help persons abstain from sexual intercourse, delay initiation of intercourse, reduce the number of sex partners, and increase the use of effective physical barriers, such as condoms, or emerging chemical barriers, such as microbicides. Further attention must be given to helping parents become better at imparting STD information. Currently, a small percentage of adolescents receive STD prevention information from parents.[43] Schools are the main source of STD information for most teenagers,43 indicating that school-based interventions can play a significant role in informing young people about STD exposure and transmission issues and in motivating them to modify their behaviors.43 (See Focus Area 7. Educational and Community-Based Programs.) Both school-based health information and school-based health service programs are potentially beneficial to young persons.[44]
Mass media campaigns have been effective in bringing about significant changes in awareness, attitude, knowledge, and behaviors for other health problems, such as smoking.[45] National communication efforts are needed to help overcome widespread misinformation and lack of awareness about STDs.
Biomedical interventions can affect aspects of transmission and duration factors. Vaccines minimize the probability of infection, disease, or both, after exposure (transmission). While vaccines for some STDs are in various stages of development, the only effective and widely available STD vaccine is for hepatitis B.[46], [47] Unfortunately, hepatitis B vaccine coverage remains minimal, especially in high-risk groups, mainly due to a lack of awareness on the part of health care providers, limited opportunities to reach high-risk youth in traditional health care settings, and limited financial support for wide-scale implementation of this effective intervention. (See Focus Area 14. Immunization and Infectious Diseases.)
Correct and consistent condom use decreases STD transmission.[48] While condom use has been on the rise in the United States over the past few decades,[49] women who use the most effective forms of contraception (sterilization and hormonal contraception) are less likely to use condoms for STD prevention.[50], [51], [52] IOM stated in its report, “Because no single method of preventing STDs or pregnancy confers the maximum level of protection against both conditions, use of dual protection—that is, a condom and another effective contraceptive for pregnancy—is especially important. Not clear, however, is how well the public understands the need for dual protection against STDs and pregnancy.”3 Dual methods could prevent unwanted pregnancy and STDs.[53] Yet most sexually active young people do not employ this strategy.[54] See Focus Area 9. Family Planning.)
Identifying and treating partners of persons with curable STDs to break the chain of transmission in a sexual network always have been integral to organized control programs.[55] Early antimicrobial prophylaxis of the exposed partner reduces the likelihood of transmission and thwarts infection. With partner treatment, the initially infected person benefits from a reduced risk of reinfection from an untreated partner, and the partner avoids acute infection and its potential complications. Future sex partners are protected by treating partners; thus, this treatment strategy also benefits the community.
Active partner notification and partner treatment generally have been the responsibility of personnel in public STD clinics. New approaches for getting more partners treated are being assessed both in traditional and nontraditional STD treatment settings. One approach actively involves initially infected patients in the process of referring their partners for evaluation and treatment.[56] Another approach uses new techniques to assess sexual networks in outbreak situations in order to identify infected patients and their partners more quickly.[57] Because most STD care in the United States is delivered in the private sector, private health care providers, managed-care organizations, and health departments need to work together to overcome barriers to rapid and effective treatment of the nonplan sex partners of health plan members.
Screening and treatment of STDs affect both transmission and duration factors. For curable STDs, screening and treatment can be cost-effective, or even cost-saving, in altering the period during which infected persons can infect others. Screening for STDs clearly meets the criteria for an effective preventive intervention.[58] For STDs that frequently are asymptomatic, screening and treatment benefit those who are likely to suffer severe complications (especially women) if infections are not detected and treated early.[59] For example, in a randomized controlled trial conducted in a large managed-care organization, chlamydia screening reduced by 56 percent new cases of subsequent pelvic inflammatory disease in a screened group.[60] Selective screening for chlamydia in the Pacific Northwest reduced the burden of disease in the screened population by 60 percent in 5 years.[61]
When combined with a new generation of sensitive and rapid diagnostic tests, some of which can be performed on a urine specimen, STD screening of specific high-risk populations in nontraditional settings appears to be a promising control strategy that expands access to underserved groups.[62] The success of screening programs will depend on the availability of funds, the willingness of communities and institutions to support them, and the availability of well-trained health care providers and of well-equipped and accessible laboratories.
Significant progress was made during the 1990s toward reducing the burden of the common bacterial STDs in the United States, such as gonorrhea, syphilis, and congenital syphilis—diseases for which national control programs have existed for the longest period. Encouraging data are emerging from a new and expanding chlamydia prevention program, suggesting that chlamydia screening is reducing disease burden and preventing complications. Nevertheless, STD complications, such as PID, continue to take a heavy toll on women’s health and increase health care costs.
Because so many people are already infected, and millions more are infected annually, viral STDs continue to present challenges for prevention and control. One of the most serious health problems associated with STDs is sexually acquired HIV infection that is facilitated by the presence of an inflammatory or ulcerative STD in one or both sex partners. In 1998, females accounted for 23 percent of all AIDS cases in the United States, with African American and Hispanic females incurring a disproportionate share (similar to other STDs) of heterosexually transmitted HIV infection.40 A nationally representative study showed that genital herpes infection is very common in the United States.37 Nationwide, 45 million persons aged 12 years and older, or 1 out of 5 of the total adolescent and adult population, are infected with herpes simplex virus type 2. As many as 20 million persons in the United States already are infected with strains of the human papillomavirus, and an estimated 5.5 million new infections occur annually.28
Of the 17 STD-related Healthy People 2000 objectives, 10 either met or moved toward their targets. The Nation is making strides in efforts to reduce the occurrence of STDs, educate people about condom use, increase clinic services for HIV and other sexually transmitted diseases, and encourage abstinence from sexual intercourse among adolescents. Routine counseling by clinicians to prevent STDs has slipped away from its target. Two objectives have held steady: adolescents engaging in sexual intercourse and annual first-time consultations about genital herpes and warts. Another four could not be assessed.
Note: Unless otherwise noted, data are from the Centers for Disease Control and Prevention, National Center for Health Statistics, Healthy People 2000 Review, 1998–99.
Sexually Transmitted Diseases
Goal: Promote responsible sexual behaviors, strengthen community capacity, and increase access to quality services to prevent sexually transmitted diseases (STDs) and their complications.
|
Number |
Objective Short Title |
|
Bacterial STD Illness and Disability |
|
|
25-1 |
Chlamydia |
|
25-2 |
Gonorrhea |
|
25-3 |
Primary and secondary syphilis |
|
Viral STD Illness and Disability |
|
|
25-4 |
Genital herpes |
|
25-5 |
Human papillomavirus infection |
|
STD Complications Affecting Females |
|
|
25-6 |
Pelvic inflammatory disease (PID) |
|
25-7 |
Fertility problems |
|
25-8 |
Heterosexually transmitted HIV infection in women |
|
STD Complications Affecting the Fetus and Newborn |
|
|
25-9 |
Congenital syphilis |
|
25-10 |
Neonatal STDs |
|
Personal Behaviors |
|
|
25-11 |
Responsible adolescent sexual behavior |
|
25-12 |
Responsible sexual behavior messages on television |
|
Community Protection Infrastructure |
|
|
25-13 |
Hepatitis B vaccine services in STD clinics |
|
25-14 |
Screening in youth detention facilities and jails |
|
25-15 |
Contracts to treat nonplan partners of STD patients |
|
Personal Health Services |
|
|
25-16 |
Annual screening for genital chlamydia |
|
25-17 |
Screening of pregnant women |
|
25-18 |
Compliance with recognized STD treatment standards |
|
25-19 |
Provider referral services for sex partners |
Reduce the proportion of adolescents and young adults with Chlamydia trachomatis infections. |
Target and baseline:
|
Objective |
Reduction in Chlamydia
trachomatis |
1997 |
2010 |
|
Percent |
|||
|
25-1a. |
Females aged 15 to 24
years attending |
5.0 |
3.0 |
|
25-1b. |
Females aged 15 to 24 years attending STD clinics |
12.2 |
3.0 |
|
25-1c. |
Males aged 15 to 24 years attending STD clinics |
15.7 |
3.0 |
Target setting method: Better than the best.
Data source: STD Surveillance System, CDC, NCHSTP.
|
Persons Aged 15 to 24
Years |
Infected With Chlamydia |
||
|
25-1a.
|
25-1b.
|
25-1c.
|
|
|
Percent |
|||
|
TOTAL |
5.0 |
12.2 |
15.7 |
|
Race and ethnicity |
|||
|
American Indian or Alaska Native |
6.3 |
13.1 |
12.6 |
|
Asian or Pacific Islander |
4.7 |
12.0 |
16.6 |
|
Asian |
DNC |
DNC |
DNC |
|
Native Hawaiian and |
DNC |
DNC |
DNC |
|
Black or African American |
DNC |
DNC |
DNC |
|
White |
DNC |
DNC |
DNC |
|
|
|||
|
Hispanic or Latino |
5.2 |
14.0 |
18.5 |
|
Not Hispanic or Latino |
DNC |
DNC |
DNC |
|
Black or African American |
11.1 |
15.2 |
18.1 |
|
White |
3.1 |
9.2 |
11.5 |
|
Family income level |
|||
|
Poor |
DNC |
DNC |
DNC |
|
Near poor |
DNC |
DNC |
DNC |
|
Middle/high income |
DNC |
DNC |
DNC |
DNA = Data have not been analyzed. DNC = Data are not collected. DSU = Data are statistically unreliable.
25-2 | Reduce gonorrhea. |
Target: 19 new cases per 100,000 population.
Baseline: 123 new cases of gonorrhea per 100,000 population occurred in 1997.
Target setting method: Better than the best.
Data source: STD Surveillance System, CDC, NCHSTP.
|
Total Population, 1997 |
New Gonorrhea Cases |
||
|
25-2.
|
Females* |
Males* |
|
|
Rate per 100,000 |
|||
|
TOTAL |
123 |
119 |
125 |
|
Race and ethnicity |
|||
|
American Indian or Alaska Native |
100 |
131 |
67 |
|
Asian or Pacific Islander |
20 |
21 |
18 |
|
Asian |
DNC |
DNC |
DNC |
|
Native Hawaiian and |
DNC |
DNC |
DNC |
|
Black or African American |
DNC |
DNC |
DNC |
|
White |
DNC |
DNC |
DNC |
|
|
|||
|
Hispanic or Latino |
69 |
72 |
67 |
|
Not Hispanic or Latino |
DNC |
DNC |
DNC |
|
Black or African American |
808 |
714 |
912 |
|
White |
26 |
32 |
20 |
|
Family income level |
|||
|
Poor |
DNC |
DNC |
DNC |
|
Near poor |
DNC |
DNC |
DNC |
|
Middle/high income |
DNC |
DNC |
DNC |
|
Age |
|||
|
15 to 24 years |
512 |
617 |
414 |
|
25 to 34 years |
198 |
161 |
235 |
|
35 to 44 years |
71 |
40 |
101 |
DNA = Data have not been analyzed. DNC = Data are not
collected. DSU = Data are statistically unreliable.
*Data for females and males are displayed to further
characterize the issue.
25-3 | Eliminate sustained domestic transmission of primary and secondary syphilis. |
Target: 0.2 cases per 100,000 population.
Baseline: 3.2 cases of primary and secondary syphilis per 100,000 population occurred in 1997.
Target setting method: Better than the best and consistent with the National Plan to Eliminate Syphilis from the United States, CDC, 1999.
Data source: STD Surveillance System, CDC, NCHSTP.
Total Population, 1997 |
Primary and Secondary Syphilis Cases |
|||
|
25-3.
|
Females* |
Males* |
||
|
Rate per 100,000 |
||||
|
TOTAL |
3.2 |
2.9 |
3.6 |
|
|
Race and ethnicity |
||||
|
American Indian or Alaska Native |
2.0 |
1.8 |
2.3 |
|
|
Asian or Pacific Islander |
0.3 |
0.4 |
0.3 |
|
|
Asian |
DNC |
DNC |
DNC |
|
|
Native Hawaiian and other |
DNC |
DNC |
DNC |
|
|
Black or African American |
DNC |
DNC |
DNC |
|
|
White |
DNC |
DNC |
DNC |
|
|
|
||||
|
Hispanic or Latino |
1.6 |
1.0 |
2.1 |
|
|
Not Hispanic or Latino |
DNC |
DNC |
DNC |
|
|
Black or African American |
22.0 |
19.3 |
25.0 |
|
|
White |
0.5 |
0.5 |
0.6 |
|
|
Family income level |
||||
|
Poor |
DNC |
DNC |
DNC |
|
|
Near poor |
DNC |
DNC |
DNC |
|
|
Middle/high income |
DNC |
DNC |
DNC |
|
|
Sexual orientation |
DNC |
DNC |
DNC |
|
DNA = Data have not been analyzed. DNC = Data are not
collected. DSU = Data are statistically unreliable.
*Data for females and males are displayed to further
characterize the issue.
The United States has a unique opportunity to eliminate syphilis within its borders. Syphilis is easy to detect and cure, given adequate access to and use of care. Nationally, it is at the lowest rate ever recorded and is confined to a very limited number of geographic areas. The last epidemic peaked in 1990, with the highest syphilis rate in 40 years. By 1997, the number of cases had declined by 84 percent.62 In addition, where syphilis does persist in the United States, it disproportionately affects African Americans living in poverty. Although the black:white ratio for reported syphilis has decreased since the early 1990s, the 1997 primary and secondary syphilis rate for non-Hispanic blacks was still 44 times greater than that for non-Hispanic whites.62 In 1997, of the 1,034 reported congenital syphilis cases with known race or ethnicity of the mother, non-Hispanic blacks and Hispanics accounted for 88 percent of these reported cases, while accounting for only 23 percent of the female population and 33 percent of all births.62 The persistence of high rates of syphilis in the United States is a sentinel event identifying communities in which there is a fundamental failure of basic public health capacity to control infectious diseases and ensure reproductive health.
Elimination of syphilis would have far-reaching public health implications because it would remove two devastating consequences of the disease—increased likelihood of HIV transmission and compromised ability to have healthy babies due to spontaneous abortions, stillbirths, and multisystem disorders caused by congenital syphilis acquired from mothers with syphilis. Eliminating syphilis in the United States would be a landmark achievement because it would remove these direct health burdens and would significantly decrease one of this Nation’s most glaring racial disparities in health.
While many other endemic diseases, such as polio, measles, and smallpox, have been eliminated through widespread use of vaccines, the strategies for syphilis elimination differ from these efforts largely because there currently is no vaccine. Five strategies are critical for eliminating syphilis from the United States. Two strategies—strengthened community involvement and partnerships and rapid outbreak response—will be new in many parts of the United States. The three remaining strategies—enhanced surveillance, expanded clinical and laboratory services, and enhanced health promotion—have been used for syphilis control and will be intensified and expanded for syphilis elimination.
Reduce the proportion of adults with genital herpes infection. |
Target: 14 percent.
Baseline: 17 percent of adults aged 20 to 29 years had genital herpes infection in 1988–94 (as measured by herpes simplex virus type 2 [HSV-2] antibody).
Target setting method: Better than the best.
Data source: National Health and Nutrition Examination Survey (NHANES), CDC, NCHS.
|
Adults Aged 20 to 29 Years, 1988–94 |
Infected With Genital Herpes |
|
Percent |
|
|
TOTAL |
17 |
|
Race and ethnicity |
|
|
American Indian or Alaska Native |
DSU |
|
Asian or Pacific Islander |
DSU |
|
Asian |
DNC |
|
Native Hawaiian and other Pacific Islander |
DNC |
|
Black or African American |
34 |
|
White |
15 |
|
|
|
|
Hispanic or Latino |
DSU |
|
Mexican American |
15 |
|
Not Hispanic or Latino |
DNA |
|
Black or African American |
33 |
|
White |
15 |
|
Gender |
|
|
Female (all ages) |
26 |
|
Male (all ages) |
18 |
|
Family income level |
|
|
Poor |
28 |
|
Near poor |
14 |
|
Middle/high income |
15 |
|
Age |
|
|
12 to 19 years* |
6 |
|
20 to 29 years |
17 |
|
30 to 39 years* |
28 |
|
40 to 49 years* |
27 |
DNA = Data have not been analyzed. DNC = Data are not
collected. DSU = Data are statistically unreliable.
*Data for persons aged 12 to 19 years, 30 to 39 years, and
40 to 49 years are displayed to further characterize the issue.
(Developmental) Reduce the proportion of persons with human papillomavirus (HPV) infection. |
Potential data source: National Health and Nutrition Examination Survey (NHANES), CDC, NCHS.
Reducing the number of new HPV cases can help to minimize theoverall number of cases of high-risk subtypes associated with cervical cancer in females aged 15 to 44 years. Over the past 15 years, molecular, biochemical, and epidemiologic data have firmly established the central role of several types of HPV (types 16, 18, 31, and 45) in the pathogenesis of cervical cancer.[63]
Reduce the proportion of females who have ever required treatment for pelvic inflammatory disease (PID). |
Target: 5 percent.
Baseline: 8 percent of females aged 15 to 44 years required treatment for PID in 1995.
Target setting method: Better than the best.
Data source: National Survey of Family Growth (NSFG), CDC, NCHS.
|
Females Aged 15 to 44 Years, 1995 |
Treated for PID |
|
Percent |
|
|
TOTAL |
8 |
|
Race and ethnicity |
|
|
American Indian or Alaska Native |
DSU |
|
Asian or Pacific Islander |
DSU |
|
Asian |
DNC |
|
Native Hawaiian and other Pacific Islander |
DNC |
|
Black or African American |
11 |
|
White |
7 |
|
|
|
|
Hispanic or Latino |
8 |
|
Not Hispanic or Latino |
8 |
|
Black or African American |
11 |
|
White |
7 |
|
Family income level (aged 22 to 44 years) |
|
|
Poor |
12 |
|
Near poor |
11 |
|
Middle/high income |
8 |
|
Education level (aged 22 to 44 years) |
|
|
Less than high school |
14 |
|
High school graduate |
9 |
|
At least some college |
7 |
DNA = Data have not been analyzed. DNC = Data are not collected. DSU = Data are statistically unreliable.
PID is among the most serious threats to female reproductive capability. PID is caused most frequently by chlamydial infections and gonorrhea that ascend past the cervix into the upper reproductive tract.[64] More than 1 million women have an episode of PID annually.[65], [66] PID often results in scarring and either complete or partial blockage of the fallopian tubes. As a result, as many as one-quarter of women with acute PID experience serious long-term sequelae, most often an ectopic pregnancy or tubal factor infertility. Women who have had PID are 6 to 10 times more likely to have an ectopic pregnancy compared with women who have not had PID.9 In 1992, approximately 9 percent of all pregnancy-related deaths were caused by ectopic pregnancy.[67]
Reduce the proportion of childless females with fertility problems who have had a sexually transmitted disease or who have required treatment for pelvic inflammatory disease (PID). |
Target: 15 percent.
Baseline: 27 percent of childless females aged 15 to 44 years with fertility problems had a history of STDs or PID treatment in 1995.
Target setting method: 44 percent improvement.
Data source: National Survey of Family Growth (NSFG), CDC, NCHS.
|
Childless Females Aged
15 to 44 Years |
STD History or PID Treatment |
|
Percent |
|
|
TOTAL |
27 |
|
Race and ethnicity |
|
|
American Indian or Alaska Native |
DSU |
|
Asian or Pacific Islander |
DSU |
|
Asian |
DNC |
|
Native Hawaiian and other Pacific Islander |
DNC |
|
Black or African American |
33 |
|
White |
27 |
|
|
|
|
Hispanic or Latino |
27 |
|
Not Hispanic or Latino |
27 |
|
Black or African American |
32 |
|
White |
27 |
|
Education level (aged 22 to 44 years) |
|
|
Less than high school |
30 |
|
High school graduate |
27 |
|
At least some college |
28 |
|
Age |
|
|
15 to 24 years |
23 |
|
25 to 34 years |
26 |
|
35 to 44 years |
31 |
DNA = Data have not been analyzed. DNC = Data are not collected. DSU = Data are statistically unreliable.
In 1995, there were approximately 24.2 million women aged 15 to 44 years who had not given birth to a child and had not had a sterilizing operation. Most of them (21.2 million) were presumed to be able to have a child. Perhaps these women were not aware of fertility problems (see Terminology) because they had not yet tested their fertility potential. This presumption is supported by the fact that most of these 21.2 million childless women were using contraception in 1995. While some fraction of them may remain voluntarily childless and never choose to test their fertility, most are likely to pursue childbearing at some point in the future. Approximately 2.3 million of these “untested” women in 1995 had a history of STDs or PID treatment, increasing the likelihood that some of them will experience a fertility problem in the future. If the social stigma associated with STDs resulted in any underreporting of STDs in this self-report survey, the 2.3 million women at risk for future fertility problems may be a low estimate.
At the time of the NSFG in 1995, nearly 3 million of the 24.2 million childless women had a fertility problem. A subset of this group, approximately 800,000 women, had a history of STDs or PID treatment. This subset comprised 27 percent of the women with known fertility problems, which may be a low estimate of the contribution made by previous STDs or PID to the fertility problems among childless women. Because bacterial STDs and PID may be asymptomatic when present and because diagnosing tubal factor infertility caused by PID is both difficult and expensive, many women with fertility problems may not be aware of having had an STD or PID in the past. Evidence has shown that reducing the burden of bacterial STDs in reproductive age women can dramatically reduce the amount of PID60 and through this mechanism could reduce fertility problems.
(Developmental) Reduce HIV infections in adolescent and young adult females aged 13 to 24 years that are associated with heterosexual contact. |
Potential data source: HIV/AIDS Surveillance System, CDC, NCHSTP.
Reduce congenital syphilis. |
Target: 1 new case per 100,000 live births.
Baseline: 27 new cases of congenital syphilis per 100,000 live births were reported in 1997.
Target setting method: Better than the best and consistent with the National Plan to Eliminate Syphilis from the United States, CDC, 1998.
Data sources: STD Surveillance System, CDC, NCHSTP; National Vital Statistics System (NVSS), CDC, NCHS.
|
Live Births, 1997 |
New
Congenital |
|
Rate per 100,000 |
|
|
TOTAL |
27 |
|
Mother’s race and ethnicity |
|
|
American Indian or Alaska Native |
11 |
|
Asian or Pacific Islander |
8 |
|
Asian |
DNC |
|
Native Hawaiian and other Pacific Islander |
DNC |
|
Black or African American |
DNC |
|
White |
DNC |
|
|
|
|
Hispanic or Latino |
34 |
|
Not Hispanic or Latino |
DNC |
|
Black or African American |
123 |
|
White |
4 |
|
Family income level |
|
|
Poor |
DNC |
|
Near poor |
DNC |
|
Middle/high income |
DNC |
DNA = Data have not been analyzed. DNC = Data are not collected. DSU = Data are statistically unreliable.
(Developmental) Reduce neonatal consequences from maternal sexually transmitted diseases, including chlamydial pneumonia, gonococcal and chlamydial ophthalmia neonatorum, laryngeal papillomatosis (from human papillomavirus infection), neonatal herpes, and preterm birth and low birth weight associated with bacterial vaginosis. |
Potential data source: STD Surveillance System, CDC, NCHSTP.
Increase the proportion of adolescents who abstain from sexual intercourse or use condoms if currently sexually active. |
Target: 95 percent.
Baseline: 85 percent of adolescents in grades 9 through 12 abstained from sexual intercourse or used condoms in 1999 (50 percent had never had intercourse; 14 percent had intercourse but not in the past 3 months; and 21 percent currently were sexually active and used a condom at last intercourse).
Target setting method: 12 percent improvement.
Data source: Youth Risk Behavior Surveillance System (YRBSS), CDC, NCCDPHP.
|
Students in Grades 9 Through 12, 1999 |
25-11. |
NOT Currently Sexually Active |
Currently Sexually Active |
||||
|
Never Had Intercourse* [Column b] |
No Intercourse in Past 3 Months* [Column c] |
Used Condom at Last Intercourse* [Column d] |
Did NOT Use Condom at Last Intercourse [Column e] |
||||
|
Percent |
|||||||
|
TOTAL |
85 |
50 |
14 |
21 |
15 |
||
|
Race and ethnicity |
|||||||
|
American Indian or Alaska Native |
DSU |
DSU |
DSU |
DSU |
DSU |
||
|
Asian or Pacific |
DSU |
DSU |
DSU |
DSU |
DSU |
||
|
Asian |
DNC |
DNC |
DNC |
DNC |
DNC |
||
|
Native
Hawaiian and other Pacific |
DNC |
DNC |
DNC |
DNC |
DNC |
||
|
Black
or African |
83 |
30 |
17 |
36 |
17 |
||
|
White |
86 |
55 |
13 |
18 |
14 |
||
|
|
|||||||
|
Hispanic or Latino |
84 |
46 |
18 |
20 |
16 |
||
|
Not Hispanic or Latino |
85 |
51 |
13 |
21 |
15 |
||
|
Black or African |
84 |
29 |
18 |
37 |
16 |
||
|
White |
85 |
55 |
12 |
18 |
15 |
||
|
Gender |
|||||||
|
Female |
81 |
52 |
11 |
18 |
18 |
||
|
Male |
87 |
48 |
16 |
23 |
13 |
||
|
Grade |
|||||||
|
9th |
90 |
61 |
12 |
17 |
10 |
||
|
10th |
87 |
53 |
14 |
20 |
13 |
||
|
11th |
84 |
47 |
15 |
22 |
16 |
||
|
12th |
73 |
35 |
14 |
24 |
27 |
||
|
Sexual orientation |
DNC |
DNC |
DNC |
DNC |
DNC |
||
|
Select populations |
|||||||
|
Number of sex partners(past 3 months) |
|||||||
|
None |
100 |
79 |
21 |
NA |
NA |
||
|
1 |
57 |
NA |
NA |
57 |
43 |
||
|
2 to 3 |
62 |
NA |
NA |
62 |
38 |
||
|
4 or more |
60 |
NA |
NA |
60 |
40 |
||
DNA = Data have not been
analyzed. DNC = Data are not collected. DSU = Data are statistically unreliable.
NA = Not applicable.
*Data for never had intercourse, had intercourse but
not in the past 3 months, and currently sexually active and used a condom at
last intercourse are displayed to further characterize the issue.
Promoting responsible adolescent sexual behavior targets three protective behaviors that reduce the risk of STDs (including HIV infection) and unintended pregnancy. These behaviors are especially relevant to young people who, as a group, experience a disproportionate share of STDs and unintended pregnancies when they engage in sexual intercourse.36, 37 The protective behaviors of interest are completely abstaining from sexual intercourse during adolescence (primary abstinence), reverting to abstinence for long periods of time after having had intercourse in the past (secondary abstinence), and at least using condoms (a single method that offers protection against both pregnancy and some STDs) consistently and correctly if regular intercourse is occurring. In 1999, 85 percent of high school youth demonstrated at least one of these behaviors. In contrast, the remaining 15 percent were sexually active and did not use a condom at last intercourse, placing them at high risk for STDs and unwanted pregnancy. Increasing and maintaining the proportion of youth who exhibit the above protective behaviors reduce the risks of HIV infection, other STDs, and unintended pregnancies for adolescents because the proportion of youth who are currently sexually active and do not use condoms will be reduced.
Various societal institutions (such as parents and families, schools, health care providers, postsecondary institutions, religious organizations, media, employers, community agencies that serve youth, celebrities, and government agencies) can positively influence the health and behaviors of the Nation’s youth. Collaboration among these institutions can (1) help adolescents abstain from sexual intercourse, (2) help them overcome pressure to become sexually active prematurely, and (3) ensure accessible, confidential community counseling and clinical services for young people who are or have been sexually active.
Abstaining from sexual intercourse offers maximum protection to adolescents who are generally poorly prepared to deal with the physical and psychological consequences of HIV infection, other STDs, and pregnancy. Overall, 50 percent of high school youth fell into this category (see objective 25-11 population data table). Abstaining from sexual intercourse while in high school varied by race and ethnicity, for example, from 55 percent among white youth to 29 percent among African American youth. Abstaining from intercourse decreased as young people progressed through high school, from 61 percent among 9th graders to 35 percent among 12th graders. These data point out that while 61 percent of 9th graders had never had sexual intercourse, at least 39 percent had intercourse during or before 9th grade. Among the 39 percent, 12 percent had not had intercourse in the past 3 months, 17 percent were currently sexually active and used a condom at last intercourse, and the remaining 10 percent were sexually active and did not use a condom at last intercourse. These data suggest a need for counseling, support, education, and services for many young people even before high school begins.
Young people who have had sexual intercourse in the past but are not currently sexually active need special attention and services. Overall, 14 percent of high school youth fall into this category. Slightly more males (16 percent) than females (11 percent) fit into this category. More African American (18 percent) and Hispanic (18 percent) youth fit into this category than do white (12 percent) youth. Even if pregnancy were avoided in the past, the same may not be true for STDs. Some youth may have acquired viral or bacterial STDs that have not been recognized or treated. Previously sexually active adolescents need to be educated about this possibility, and medical evaluation and counseling are strongly suggested both to identify treatable conditions and to reinforce abstinence messages.
Young people who are currently sexually active also require special attention and services. This requirement applies both to the 21 percent of high school youth who were sexually active and used a condom at last intercourse and the remaining 15 percent of youth who were currently sexually active and did not use a condom at last intercourse. These data illustrate wide variation in current sexual activity by race/ethnicity. For African American high school youth, 53 percent were sexually active (37 percent were sexually active and used a condom at last intercourse, and 16 percent were sexually active but did not use a condom at last intercourse). For Hispanic youth, 36 percent were sexually active (20 percent were sexually active and used a condom, and 16 percent were sexually active and did not use a condom). Among white youth, 33 percent were sexually active (18 percent used a condom at last intercourse, and 15 percent did not use a condom). Also, fewer sex partners among currently sexually active youth does not equate with a much higher degree of condom use. Regardless of the number of sex partners in a given interval, approximately one of every two sexually active adolescents did not use a condom at last intercourse. For example, for adolescents who had four or more sex partners in the past 3 months, 40 percent of them would be considered to be at very high risk for STDs (including HIV infection) and possibly pregnancy by not using condoms consistently. Even for youth with one sex partner in the past 3 months, 43 percent did not use condoms consistently. In addition to reinforcing abstinence messages, adult counselors of currently sexually active adolescents must be aware that there is ongoing, very high risk of HIV infection, other STDs, and pregnancy. Responsible and influential adults should help young males and females gain easy access to high quality, confidential, comprehensive reproductive health care in their communities that can help them reduce HIV infection, STD, and pregnancy risk. This is especially true for adolescent females, who bear all the physical consequences of unintended pregnancy and bear disproportionate short- and long-term complications from STDs.
(Developmental) Increase the number of positive messages related to responsible sexual behavior during weekday and nightly prime-time television programming. |
Potential data source: CDC, NCHSTP.
Television messages hold the potential to promote responsible sexual behaviors, such as abstinence, delaying sexual intercourse, or using effective methods to prevent STDs and pregnancy, such as use of condoms and hormonal contraception.
Increase the proportion of Tribal, State, and local sexually transmitted disease programs that routinely offer hepatitis B vaccines to all STD clients. |
Target: 90 percent.
Baseline: 5 percent of State and local STD programs offered hepatitis B vaccines to clients in accordance with CDC guidelines in 1998.46, [68] Tribal STD program data are developmental.
Target setting method: 85 percentage point improvement.
Data sources: Survey of STD Programs, National Coalition of STD Directors (NCSD); IHS.
Routine vaccination of infants is expected to produce a highly immune population to eliminate hepatitis B virus transmission in the United States. However, high rates of acute hepatitis B continue to occur in young adult risk groups, particularly persons with a history of another sexually transmitted disease and persons with multiple sex partners. Approximately 50 percent of new infections occur in persons with a sexual risk factor for transmission, and most of these persons have had a missed opportunity to be vaccinated. For example, 42 percent of acute hepatitis B cases reported in the CDC Sentinel Counties Study of Viral Hepatitis in 1996 had been treated for a sexually transmitted disease in the past.
25-14. | (Developmental) Increase the proportion of youth detention facilities and adult city or county jails that screen for common bacterial sexually transmitted diseases within 24 hours of admission and treat STDs (when necessary) before persons are released. |
Potential data sources: Annual Survey of Correctional Facilities, CDC, NCHSTP and National Institute of Justice; U.S. Department of Justice, Bureau of Justice Statistics.
25-15. | (Developmental) Increase the proportion of all local health departments that have contracts with managed care providers for the treatment of nonplan partners of patients with bacterial sexually transmitted diseases (gonorrhea, syphilis, and chlamydia). |
Potential data source: Survey of STD Programs, National Coalition of STD Directors (NCSD).
25-16. | (Developmental) Increase the proportion of sexually active females aged 25 years and under who are screened annually for genital chlamydia infections. |
Potential data sources: Family Planning Annual Report, OPA; STD Surveillance System, CDC, NCHSTP.
Routine screening for asymptomatic infection with Chlamydia trachomatis during pelvic examination is recommended for all sexually active female adolescents and for other women at high risk for chlamydial infection. While evidence is insufficient to make a recommendation concerning routine screening of sexually active males, in situations where asymptomatic chlamydial infection is high in males, screening using urine-based tests may be recommended to prevent spread of the infection.58 Reported chlamydial infection rates in males are highest among those aged 20 to 24 years.
25-17. | (Developmental) Increase the proportion of pregnant females screened for sexually transmitted diseases (including HIV infection and bacterial vaginosis) during prenatal health care visits, according to recognized standards. |
Potential data source: STD Surveillance System, CDC, NCHSTP.
While evidence is insufficient to make a recommendation concerning routine screening of pregnant females for STDs, the benefits of early intervention in HIV-asymptomatic pregnant women, for example, are known. Similar benefits have been demonstrated in detecting and treating asymptomatic chlamydia infection in pregnancy.58
25-18. | Increase the proportion of primary care providers who treat patients with sexually transmitted diseases and who manage cases according to recognized standards. |
Target: 90 percent.
Baseline: 70 percent of primary care providers treated patients with STDs according to CDC STD Treatment Guidelines in 1988.
Target setting method: Retain 2000 target.
Data sources: National Disease and Therapeutic Index, IMS America; National Ambulatory Medical Care Survey (NAMCS), CDC, NCHS.
25-19. | (Developmental) Increase the proportion of all sexually transmitted disease clinic patients who are being treated for bacterial STDs (chlamydia, gonorrhea, and syphilis) and who are offered provider referral services for their sex partners. |
Potential data source: STD Surveillance System, CDC, NCHSTP.
(A listing of abbreviations and acronyms used in this publication appears in Appendix H.)
Bacterial and protozoal STDs: Refer to curable sexually transmitted infections caused by Chlamydia trachomatis (chlamydia), Neisseria gonorrhoeae (gonorrhea), Treponema pallidum (syphilis), Haemophilus ducreyi (chancroid), Trichomonas vaginalis (trichomoniasis), bacterial vaginosis, and other organisms.
Congenital syphilis: A condition in a fetus or newborn caused by infection with the syphilis bacteria from an untreated mother. Infected newborns show a wide spectrum of clinical signs, and only severe cases are clinically apparent at birth. Severe illness or death can result after birth if the newborn is not treated.
Fertility problems: Refer to the standard medical definitions of infertility (have not used contraception and have not become pregnant for 12 months or more) or impaired fecundity (women reporting no sterilizing operation and classified as finding it difficult or impossible to get pregnant or carry a baby to term).
Provider referral: Formerly called contact tracing, the process whereby health department personnel directly and confidentially notify the sex partners of infected individuals about their exposure to a sexually transmitted disease for the purposes of education, counseling, and referral to health care services.
STD complications: Refer to serious health problems that occur following an acute bacterial or viral STD. Among the most serious of these complications:
Cancer: Includes cervical cancer and its precursors (due to some strains of human papillomavirus) and liver cancer that can result after chronic infection with hepatitis B virus.
Infection of a fetus or newborn: Includes conditions such as congenital syphilis, neonatal herpes, HIV infection, eye infections, and pneumonia.
Pelvic inflammatory disease (PID): Can cause permanent damage to the female reproductive tract and lead to ectopic pregnancy, infertility, or chronic pelvic pain.
Preterm birth: Can result from maternal infection.
Sexually transmitted HIV infection: Can be facilitated by the presence of an inflammatory or ulcerative STD in one or both sex partners.
Syphilis elimination: Refers to the elimination of sustained domestic transmission of syphilis. Term means that there is no continuing transmission of the disease within a community or jurisdiction and absence of transmission within a jurisdiction except within 90 days of report of an imported case.
Viral STDs: Refer to the sexually transmitted viral infections—HIV infection, genital herpes, and HPV infection. Initial infections with these organisms may be asymptomatic or may cause only mild symptoms. Hepatitis B virus and hepatitis C virus can be transmitted through sexual activity.
[1] United Nations. Report of the International Conference on Population and Development Cairo, Egypt, September 5-13, 1994. New York, NY: United Nations, 1995.
[2] St. Louis, M.E.; Wasserheit, J.N.; and Gayle, H.D. (Editorial) Janus considers the HIV pandemic-harnessing recent advances to enhance AIDS prevention. American Journal of Public Health 87:10-12, 1997. PubMed; PMID 9065212
[3] Institute of Medicine (IOM). Eng, T.R., and Butler, W.T., eds. The Hidden Epidemic: Confronting Sexually Transmitted Diseases. Washington, DC: National Academy Press, 1997.
[4] Fish, A.; Fairweather, D.; Oriel, J.; et al. Chlamydia trachomatis infection in a gynecology clinic population: Identification of high-risk groups and the value of contact tracing. European Journal of Obstetrics, Gynecology and Reproductive Biology 31:67-74, 1989. PubMed; PMID 2653896
[5] Handsfield, H.; Jasman, L.; Roberts, P.; et al. Criteria for selective screening for Chlamydia trachomatis infection in women attending family planning clinics. Journal of the American Medical Association 255:1730-1734, 1986. PubMed; PMID 3081742
[6] Judson, F. Gonorrhea. Medical Clinics of North America 74:1353-1367, 1990. PubMed; PMID 2123279
[7] Stamm, W., and Holmes, K. Chlamydia trachomatis infections in the adult. In: Holmes, K.; Mardh, P.A.; Sparling, P.; et al.; eds. Sexually Transmitted Diseases. 2nd ed. New York, NY: McGraw-Hill, Inc., 1990, 181-193.
[8] Beasley, R.P.; Hwang, L.Y.; Lin, C.C.; et al. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22,707 men in Taiwan. Lancet 2(8256):1129-1133, 1981. PubMed; PMID 6087457
[9] Marchbanks, P.; Annegers, J.; Coulam, C.; et al. Risk factors for ectopic pregnancy: A population-based study. Journal of the American Medical Association 259:1823-1827, 1988.
[10] Cates, W. Epidemiology and control of sexually transmitted diseases in adolescents. In: Schydlower, M., and Shafer, M., eds. AIDS and Other Sexually Transmitted Diseases. Philadelphia, PA: Hanly & Belfus, Inc., 1990, 409-427.
[11] Blank, S.; McDonnell, D.; Rubin, et al. New approaches to syphilis control: Finding opportunities for syphilis treatment and congenital syphilis prevention in a women’s correctional setting. Sexually Transmitted Diseases 24(4):218-228, 1997. PubMed; PMID 9101633
[12] Cohen, D.; Scribner, R.; Clark, J.; et al. The potential role of custody facilities in controlling sexually transmitted diseases. American Journal of Public Health 82:552-556, 1992. PubMed; PMID 1546771
[13] Oh, M.; Cloud, G.; Wallace, L.; et al. Sexual behavior and sexually transmitted diseases among male adolescents in detention. Sexually Transmitted Diseases 21:127-132, 1994. PubMed; PMID 8073340
[14] Landry, D., and Forrest, J. Public health departments providing STD services. Family Planning Perspectives 28:261-266, 1996. PubMed; PMID 8959416
[15] Beltrami, J.; Wright-DeAguero, L.; Fullilove, M.; et al. Substance Abuse and the Spread of Sexually Transmitted Diseases. Commissioned paper for the IOM Committee on Prevention and Control of STDs, 1997.
[16] Marx, R.; Aral, S.; Rolfs, R.; et al. Crack, sex, and STDs. Sexually Transmitted Diseases 18:92-101, 1991. PubMed; PMID 1862466
[17] Gunn, R.; Montes, J.; Toomey, K.; et al. Syphilis in San Diego County 1983–1992: Crack cocaine, prostitution, and the limitations of partner notification. Sexually Transmitted Diseases 22:60-66, 1995. PubMed; PMID 7709327
[18] Abma, J.; Driscoll, A.; and Moore, K. Young women’s degree of control over first intercourse: An exploratory analysis. Family Planning Perspectives 30(1):12-18, 1998. PubMed; PMID 9494810
[19] Abma, J.; Chandra, A.; Mosher, W.; et al. Fertility, family planning, and women’s health: New data from the 1995 National Survey of Family Growth. Vital and Health Statistics 23(19), 1997. PubMed; PMID 9201902
[20] Miller, B.; Monson, B.; and Norton, M. The effects of forced sexual intercourse on white female adolescents. Child Abuse and Neglect 19:1289-1301, 1995. PubMed; PMID 8556443
[21] Brandt, A. No Magic Bullet: A Social History of Venereal Disease in the United States Since 1880. New York, NY: Oxford University Press, Inc., 1985.
[22] EDK Associates. The ABCs of STDs. New York, NY: EDK Associates, 1995.
[23] IOM. Summary—The Hidden Epidemic: Confronting Sexually Transmitted Diseases. Washington, DC: National Academy Press, 1997.
[24] Lawrence, L. How OB-GYNs are failing women. Glamour 10:292, 1997.
[25] Lowry, D., and Schindler, J. Prime time TV portrayals of sex, “Safe sex and AIDS: A longitudinal analysis.” Journalism Quarterly 70:628-637, 1993.
[26] Tsui, A.; Wasserheit, J.; and Haaga, J. Reproductive Health in Developing Countries: Expanding Dimensions, Building Solutions. Washington, DC: National Academy Press, 1997.
[27] Centers for Disease Control and Prevention (CDC). Ten leading national notifiable infectious diseases—United States, 1995. Morbidity and Mortality Weekly Report 45:883-884, 1996. PubMed; PMID 8927008
[28] American Social Health Association. Sexually Transmitted Diseases in America: How Many Cases and at What Cost? Menlo Park, CA: Kaiser Family Foundation, 1998.
[29] Chandra, A., and Stephen, E. Impaired fecundity in the United States: 1982–1995. Family Planning Perspectives 30(1):34-42, 1998. PubMed; PMID 9494814
[30] Holmes, K.; Johnson, D.; and Trostle, H. An estimate of the risk of men acquiring gonorrhea by sexual contact with infected females. American Journal of Epidemiology 91:170-174, 1970. PubMed; PMID 5416250
[31] Brunham, R.; Holmes, K.; and Embree, J. Sexually transmitted diseases in pregnancy. In: Holmes, K.; Mardh, P.; Sparling, P.; et al.; eds. Sexually Transmitted Diseases. 2nd ed. New York, NY: McGraw-Hill, Inc., 1990, 771-801.
[32] Goldenberg, R.L.; Andrews, W.W.; Yuan, A.C.; et al. Sexually transmitted diseases and adverse outcomes of pregnancy. Clinics in Perinatology 24(1):23-41, 1997. PubMed; PMID 9099500
[33] Hillier, S.; Nugent, R.; Eschenbach, D.; et al. Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. New England Journal of Medicine 333:1737-1742, 1995. PubMed; PMID 7491137
[34] Meis, P.J.; Goldenberg, R.L.; Mercer, G.; et al. The preterm prediction study: Significance of vaginal infections. American Journal of Obstetrics and Gynecology 173(4):1231-1235, 1995. PubMed; PMID 7485327
[35] Alan Guttmacher Institute. Sex and America’s Teenagers. New York, NY: the Institute, 1994.
[36] CDC, Division of STD Prevention. Sexually Transmitted Disease Surveillance, 1997. U.S. Department of Health and Human Services (HHS), Public Health Service (PHS). Atlanta, GA: CDC, September 1998.
[37] Fleming, D.T.; McQuillan, G.M.; Johnson, R.E.; et al. Herpes Simplex Virus Type 2 in the United States, 1976 to 1994. New England Journal of Medicine 337:1105-1111, 1997. PubMed; PMID 9329932
[38] Warren, C.; Santelli, J.; Everett, S.; et al. Sexual behavior among U.S. high school students, 1990–1995. Family Planning Perspectives 30(4):170-172, 1998. PubMed; PMID 9711454
[39] Kost, I., and Forrest, J.D. American Women’s sexual behavior and exposure to risk of sexually transmitted diseases. Family Planning Perspectives 24:244-254, 1992. PubMed; PMID 1483527
[40] CDC. HIV/AIDS Surveillance Report, 1998 10(No. 2), 1998.
[41] Anderson, R. The transmission dynamics of sexually transmitted diseases: The behavior component. In: Wasserheit, H.; Aral, S.; Holmes, K.; et al.; eds. Research Issues in Human Behavior and Sexually Transmitted Diseases in the AIDS Era. Washington, DC: American Society for Microbiology, 1991, 38-60.
[42] May, R., and Anderson, R. Transmission dynamics of HIV infection. Nature 326:137-142, 1987. PubMed; PMID 3821890
[43] American Social Health Association. Teenagers know more than adults about STDs, but knowledge among both groups is low. STD News 3:1, 5, 1996.
[44] Kirby, D. Sexuality and HIV education programs in schools. In: Garrison, J.; Smith, M.; and Besharov, D.; eds. Sexuality and American Social Policy: A Seminar Series. Sex Education in the Schools. Menlo Park, CA: Henry J. Kaiser Family Foundation, 1994, 1-41.
[45] Flay, B. Mass media and smoking cessation: A critical review. American Journal of Public Health 77:153-160, 1987. PubMed; PMID 3541650
[46] CDC. Hepatitis B virus: A comprehensive strategy for eliminating transmission in the United States through universal childhood vaccination: Recommendations of the Immunization Practices Advisory Committee (ACIP). Morbidity and Mortality Weekly Report 40(RR-13):1-20, 1991. PubMed; PMID 1835756
[47] CDC. Under vaccination for hepatitis B among young men who have sex with men—San Francisco and Berkeley, California, 1992–1993. Morbidity and Mortality Weekly Report 45:215-217, 1996. PubMed; PMID 8609877
[48] Roper, W.L.; Peterson, H.B.; and Curran, J.W. Commentary: Condoms and HIV prevention—clarifying the message. American Journal of Public Health 83:501-503, 1993. PubMed; PMID 8460725
[49] Piccinino, L., and Mosher, W. Trends in contraceptive use in the United States: 1982–1995. Family Planning Perspectives 30(1):4-10, 46, 1998. PubMed; PMID 9494809
[50] Anderson, J.; Brackbill, R.; and Mosher, W. Condom use for disease prevention among unmarried U.S. women. Family Planning Perspectives 28:25-28, 39, 1996. PubMed; PMID 8822412
[51] CDC. HIV-risk behaviors of sterilized and nonsterilized women in drug-treatment programs—Philadelphia, 1989–1991. Morbidity and Mortality Weekly Report 41:149-152, 1992. PubMed; PMID 1741006
[52] CDC. Surgical sterilization among women and use of condoms—Baltimore, 1989–1990. Morbidity and Mortality Weekly Report 41:568-575, 1992. PubMed; PMID 1640923
[53] Cates, W., and Stone, K. Family planning, sexually transmitted diseases, and contraceptive choice: A literature update. Family Planning Perspectives 24:75-84, 1992. PubMed; PMID 1628715
[54] IOM. Brown, S., and Eisenberg, L., eds. Best Intentions: Unintended Pregnancy and the Well-Being of Children and Families. Washington, DC: National Academy Press, 1995.
[55] Rothenberg, R., and Potterat, J. Strategies for management of sex partners. In: Holmes, K.; Mardh, P.A.; Sparling, P.; et al.; eds. Sexually Transmitted Diseases. 2nd ed. New York, NY: McGraw-Hill, Inc., 1990, 1081-1086.
[56] CDC. Alternate case-finding methods in a crack-related syphilis epidemic—Philadelphia. Morbidity and Mortality Weekly Report 40:77-80, 1991. PubMed; PMID 1899127
[57] Engelgau, M.; Woernle, C.; Rolfs, R.; et al. Control of epidemic early syphilis: The results of an intervention campaign using social networks. Sexually Transmitted Diseases 22:203-209, 1995. PubMed; PMID 7482101
[58] U.S. Preventive Services Task Force. Guide to Clinical Preventive Services. 2nd ed. Washington, DC: HHS, 1996.
[59] Hillis, S.; Nakashima, A.; Amsterdam, L.; et al. The impact of a comprehensive chlamydia prevention program in Wisconsin. Family Planning Perspectives 27:108-111, 1995.
[60] Scholes, D.; Stergachis, A.; Heidrich, F.; et al. Prevention of pelvic inflammatory disease by screening for cervical chlamydial infection. New England Journal of Medicine 334:1362-1366, 1996. PubMed; PMID 8614421
[61] Britton, T.; DeLisle, S.; and Fine, D. STDs and family planning clinics: A regional program for chlamydia control that works. American Journal of Gynecological Health 6:80-87, 1992.
[62] Division of STD Prevention. Sexually Transmitted Disease Surveillance 1997 Supplement—Chlamydia Prevalence Monitoring Project Annual Report. Atlanta, GA: HHS, PHS,CDC, 1998.
[63] Kiviat, N.; Koutsky, L.; and Paavonen, J. Cervical neoplasia and other STD- related genital tract neoplasias. In: Holmes, K.; Mardh, P.; Sparling, P.; et al.; eds. Sexually Transmitted Diseases. 3rd ed. New York, NY: McGraw-Hill, 1999, 811-831.
[64] Jossens, M.O.; Schacter, J.; and Sweet, R.L. Risk factors associated with pelvic inflammatory disease of differing microbial etiologies. Obstetrics and Gynecology 83:989-997, 1984. PubMed; PMID 8190447
[65] Washington, A.E., and Katz, P. Cost and payment source for pelvic inflammatory disease. Trends and projections, 1983 through 2000. Journal of the American Medical Association 266:2565-2569, 1991. PubMed; PMID 1942401
[66] Rolfs, R.T.; Galaid, E.I.; and Zaidi, A.A. Pelvic inflammatory disease: Trends in hospitalizations and office visits, 1979 through 1988. American Journal of Obstetrics and Gynecology 166:983-990, 1992. PubMed; PMID 1550176
[67] NCHS. Advanced report of final mortality statistisics, 1992. Monthly Vital Statistics Report 43(Suppl. 6), 1994.
[68] CDC. 1998 guidelines for treatment of sexually transmitted diseases. Morbidity and Mortality Weekly Report 47(RR-1):1-118, 1998. PubMed; PMID 9461053